Objetivo: Valorar la calidad de vida relacionada con la salud (CVRS) de los pacientes con insuficiencia renal crónica sometidos a tratamiento sustitutivo de diálisis, así como evaluar la capacidad predictiva de algunas variables psicosociales (apoyo social, autoeficacia, optimismo disposicional, depresión, ansiedad y estrategias de afrontamiento) sobre los niveles de CVRS. Método: Se evaluó la CVRS de 39 pacientes en hemodiálisis mediante el instrumento SF-36. La capacidad predictiva de las variables evaluadas se analizó mediante correlaciones bivariadas y análisis de regresión múltiple. Resultados: Los pacientes mostraron niveles de CVRS inferiores a los valores normativos del instrumento. La depresión es el principal predictor de la CVRS, asociándose negativamente a todas sus dimensiones. El grado de preocupación, así como las estrategias de afrontamiento pasivo del estrés como la indefensión-desesperanza y el fatalismo, también se asocian a menores niveles de CVRS. Por el contrario, la autoeficacia, el optimismo, el apoyo social y el espíritu de lucha se asociaron a mayores niveles de CVRS. Conclusiones: Estos resultados tienen unas claras implicaciones clínicas respecto a los aspectos a los que debe orientarse la intervención psicológica destinada a la mejora de la CVRS en los enfermos renales.
Objectives: To assess health-related quality of life (HRQOL) of chronic renal failure patients undergoing dialysis replacement therapy, and to evaluate the predictive power of psychosocial variables (social support, self-efficacy, optimistic outlook, depression, anxiety and coping strategies) on the different levels of HRQOL. Methods: We evaluated the HRQOL of 39 haemodialysis patients using the SF-36 instrument. The predictive ability of the evaluated variables was analysed using bivariate correlations and multiple regression analysis. Results: Patients showed lower levels of HRQOL than the reference values for the instrument. Depression is the main predictor of HRQOL, associated negatively with all of its components. The degree of concern and the use of passive coping strategies for stress such as helplessness-hopelessness and fatalism are also associated with lower levels of HRQOL. By contrast, self-efficacy, optimism, social support, and fighting spirit were associated with higher levels of HRQOL. Conclusions: These results have clear clinical implications regarding the ways in which psychological interventions should be aimed at improving HRQOL in renal patients.
INTRODUCTION
In recent decades, several medical advancements have been made in optimising haemodialysis techniques. However, chronic kidney disease and dialytic treatments continue to produce physical, psychological, and social changes in patients.1 In order to evaluate the interference that renal disease and its treatments produce in the adaptive functioning of these patients, health-related quality of life (HRQOL) was developed as a method of measurement. HRQOL is an evaluation of individual health and functioning in terms of daily activities, including physical, psychological, and social function, and the patient’s general perception of health, mobility, and emotional well-being.2 HRQOL is becoming a fundamental component of providing integrated care for patients with chronic disease.1
In its use in chronic kidney disease, HRQOL indicators have proven to have a tight relationship with morbidity and mortality rates.3,4 In addition, dialysis produces several changes in patient lifestyle, which if left unattended, can decrease HRQOL.5,6 Several studies have evaluated HRQOL in renal patients on renal replacement therapy with dialysis.2,7-11 The results from these studies have shown that deterioration in HRQOL is associated with clinical,12-14 sociodemographic,13,15,16 and dialysis characteristics variables,16 as well as cognitive deterioration17 and emotional alterations.18,8
In order to provide integrated care to renal patients, it is essential that psychosocial variables that could affect HRQOL be identified, modulating the interference that the disease produces in the patient’s capacity for adaptive functioning. In our study, we focused on the following components: social support, self-efficacy, dispositional optimism, depression, anxiety, and coping strategies.
Social support consists of obtaining resources (whether material, cognitive, or emotional) through interaction with other people or sources of support. These resources reduce the perception of bodily threat and facilitate a more effective approach to coping with stressful situations.19 In renal patients, social support influences survival, adherence to treatment, and the intensity of symptoms of depression.18,20-22
Self-efficacy refers to the patient’s own concept of his/her capacity for carrying out actions that will lead to the desired results.23 In renal patients, self-efficacy is associated with self-care of the disease, adherence to treatment,10,24-26 and decreased physical and psychological symptoms.27
Dispositional optimism refers to the generalised belief or expectation that life brings positive occurrences.28 Optimism affects health through coping mechanisms, being associated with more active and effective coping29,30 as well as by decreasing physical symptoms.30 In renal patients, optimism is associated with increased social support and decreased levels of depression.31
In light of the particular life situations experienced by renal patients (loss of renal function, well-being, place in family and work, time, financial resources, and sexual function), and the continuing uncertainty surrounding their circumstances, anxiety and depression are relatively common. Depression in renal patients has been associated with immunological and nutritional dysfunction,32,33 a more negative perception of disease,9,18 and decreased HRQOL.8 Anxiety has also been associated with decreased HRQOL, primarily in the first few months of haemodialysis and in elderly patients.12
Coping strategies refer to mechanisms commonly used by the individual to deal with stress and everyday issues. These concrete strategies are used in different contexts and can change based on the situation experienced by the patient in each given moment.34 In renal patients, the coping mechanism used influences adaptation to disease and adherence to treatment.7,35,36
The objective of our study was to evaluate HRQOL in renal patients on dialysis, 55 year old or younger, from the province of Jaén, and to analyse the association between HRQOL and psychosocial variables (anxiety, depression, self-efficacy, dispositional optimism, social support, and coping strategies). The results of this study may suggest what factor(s) are the most relevant for focusing psychological interventions in order to increase HRQOL in these patients.
METHOD
Patients
Our study sample was composed of 39 chronic kidney disease patients on dialysis. The dialysis technique received was on-line in all cases, with three sessions per week (and an extra session for overweight patients) lasting four hours each (blood flow [Qb]: 250-350ml/m; dialysate flow rate [Qd]: 500ml/m; polysulfone dialyser; infusion volume: 30% dry body weight, and target Kt/V: 1.5). All sociodemographic and clinical variables are summarised in Table 1. The inclusion criteria were: age equal to or less than 55 years, on dialysis for at least 6 months, no recent severe clinical situations (hospitalisations, recent obstruction of a vascular access), psychiatric disorders, or cognitive deterioration. These criteria were used in part to ensure a better comprehension of the evaluation instruments.
Evaluation instruments
In addition to a semi-structured interview to compile information regarding sociodemographic, clinical, and lifestyle variables, we used the following questionnaires
- Short-form health and quality of life survey SF-3637. This instrument evaluates the impact of the disease on adaptive functioning. The scale consists of 36 items referring to 8 basic levels of function: physical function (self-care, walking, climbing stairs, bending over, lifting weight, etc.), physical role (work and daily activities), bodily pain (intensity of pain, in which a lower score indicates more severe pain), general health (personal evaluation of health), vitality (feelings of energy and vitality), social function (normal social life), emotional role (emotional issues), and mental health (depression, anxiety, control of behaviour, and general disposition). The internal consistency of the different sub-scales ranges between 0.7 and 0.94.
- Hospital anxiety and depression scale (HAD)38. This scale evaluates anxiety and depression without referencing somatic symptoms, which limits the possibility that symptoms derived from the underlying disease might interfere with scores. This scale consists of 14 items related to anxiety (7) and depression (7). This scale has a high internal consistency, with an α coefficient of 0.82 for the anxiety component and 0.84 for the depression component.
- Bárez scale of concerns and self-efficacy.39 This scale was developed in order to analyse the beliefs patients hold regarding their own concerns and abilities to manage certain life situations related to their disease, family, work, social activity, and finances. The scale is composed of 25 items and produces two types of scores: one related to the level of concern generated by the different situations presented, and another concerning the degree to which the patient feels capable of coping with these situations (self-efficacy). The internal consistency of this scale ranges between 0.71 and 0.86.39
- Social support scale (AS-25).40 Consists of 25 items scored on a scale of 1 to 4. The objective of this scale is to quantify the availability of social support for the patient. The internal consistency of this instrument (Cronbach’s α coefficient) is 0.87.
- Revised lifestyle orientation scale41. This is the most commonly used instrument for dispositional optimism in a patient’s disposition. The scale is composed of 10 items with a Likert-type response format. The test-retest reliability is 0.74, and internal consistency (α coefficient) is 0.87.
- Mental adjustment to disease or coping strategies42. This scale evaluates the level of a patient’s adjustment to the suffering produced by disease. It has commonly been used in cancer patients, and so we adapted the scale for use in our study by eliminating three of the items. The scale is comprised of 4 sub-scales concerning fighting spirit, anxiety, helplessness/hopelessness, and fatalism. The internal consistency of this scale ranges between 0.55 and 0.80.
Procedure and statistical analysis
Upon approval of the study protocol by the hospital administrations, patients were recruited from the four dialysis departments located in the province of Jaén (Unidad de Hemodiálisis del Hospital Médico Quirúrgico, Centro de Hemodiálisis Santa Catalina, NefroLinares, and Centro de Diálisis Playa de la Victoria). All patients that complied with inclusion criteria and were treated within the study area were invited to participate (45 patients). Of these, 39 accepted participation in the study. Once the patients were selected, we explained the research objectives and obtained signed informed consent. For the evaluation of the results, we first compiled information regarding sociodemographic, clinical, and lifestyle variables through a direct interview with each patient. We then provided each patient with a folder with each questionnaire in a counterbalanced order.
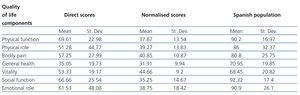
For the interpretation of the HRQOL values, the direct scores of the SF-36 were transformed into standardised scores using the available standards for the general Spanish population43 and then normalised (mean [M] =50, standard deviation [SD] =10). We analysed the relationship between predictive variables and the dependent variable (HRQOL) using an exploratory correlational analysis with bivariate Pearson’s correlation coefficients, and then performed a multiple regression analysis with a step-wise procedure. With a collinearity diagnosis, we eliminated all predictive variables with a total tolerance value less than 0.4: anxiety, which was correlated with depression (r=0.64), and fatalism, which was correlated with helplessness/hopelessness (r=0.62). The resulting predictive variables (depression, concern, self-efficacy, optimism, social support, helplessness/hopelessness, fighting spirit, and anxiety)* all had tolerance values greater than 0.5. The regression analyses produced a corrected r2 value as predictive value index of the model and standardised β values as the slope of the regression line. The level of statistical significance was set at P<.05.
* This number of predictive variables could be considered to be too large for the sample size. However, we must keep in mind that the regression model used (step-wise) does not include all predictive variables together in the model at once, but rather incorporates each one in turn if it contributes significantly to an increase in the amount of variance explained. In this sense, the maximum number of predictive variables that entered into the analyses was 4.
RESULTS
a) Quality of life levels
The scores for the different dimensions of the HRQOL (SF-36) are summarised in Table 2. As we can see, the values reported by the patients in our study are below those from the reference study in which the instrument was initially tested, with particularly low values for general health, social function, emotional role, physical function, and physical role.
b) Exploratory correlational analysis
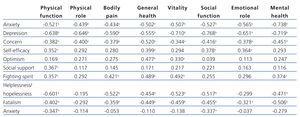
Table 3 presents the correlations between predictive variables and the various components of HRQOL. The results indicate that there were significant, negative associations with depression, anxiety, concern, and the coping strategies of helplessness/hopelessness and fatalism. On the other hand, we observed significant, positive associations with self-efficacy, optimism, social support, and the fighting spirit coping strategy.
c) Multiple regression analysis for predicting health-related quality of life
The results from the multiple regression analysis for predicting HRQOL using the psychosocial variables studied are presented in Table 4. These were the principal results we obtained:
- Depression predicts a lower HRQOL in all of the components of the SF-36.
- The level of concern predicts a lower HRQOL in the majority of the components of the HRQOL scale (physical function, physical role, general health, and mental health).
- The helplessness/hopelessness coping strategy and anxiety predict lower levels of HRQOL in the components of physical function, physical role, and social function.
- Optimism is a predictor for better general health.
DISCUSSION
Our primary objective was to evaluate HRQOL in dialysis patients in the province of Jaén. Based on our results, there appears to be a substantial impairment to HRQOL in our sample. All components of HRQOL were below the reference values established by the SF-36 questionnaire, the most heavily affected components being general health, social function, and physical function. This reflects the psychological impact that this disease has in daily activity. The worst HRQOL score was for the general health section, which implies that patients on dialysis have a negative self-assessment of current health and the possibility of future improvements. The results from our study are comparable to those from other studies that have used the SF-36 scale in patients with chronic renal failure,44 and generally corroborate the previously available evidence on the subject.1,17,36
Our second objective was to identify the psychosocial variables that could be significant predictors of HRQOL. The results clearly demonstrate that depression was the primary predictor for HRQOL in our sample, with negative correlations with all components of the SF-36 scale and accounting for approximately 50% of variance for physical function, physical role, vitality, social function, and mental health. According to our results, depression produced a highly significant impediment in daily activities, producing lower productivity than desired, increased interference of bodily pain in normal tasks, a more negative appraisal of current health and future prospects, a heightened perception of fatigue and weariness, decreased social life, and greater emotional problems that interfere with daily activities and decrease the mental health of the patient. These results are similar to those presented by other authors, who showed that depression negatively affects the quality of life of renal patients,8,45,46 their nutritional state at the start of dialysis,47 and the level of physical and mental deterioration in general, along with morbidity and mortality rates.48,49
Our results also indicated that the degree of concern professed by the patient is negatively correlated with the majority of the components of the HRQOL. This finding corroborates the results from previous studies that showed that, when renal patients are worried about situations regarding their disease, HRQOL diminishes.10,24,26 On the other hand, the correlational analysis demonstrated that the level of self-efficacy is positively associated with increased physical function, general health, social function, and emotional role. These results also reflect those from previous studies,27 where the level of self-efficacy was found to be associated with increased adherence to treatment and behaviours that promote health, and decreased physical and psychological symptoms experienced by renal patients. All of these results support the theory proposed by Bandura,23 which states that a strong sense of self-efficacy increases personal well-being and that, in contrast, individuals that doubt their own capacities shun difficult tasks, considering them to be a threat against their person. In this sense, renal patients are constantly faced with the perception of a lack of control over the situations they are experiencing in life.
Focusing our attention on optimism, this factor predicts perceptions of increased general health, including both the current state of health and perspectives for future health. In addition, as the correlational analysis showed, optimism is associated with increased vitality scores. These results concur with those from Maruta50 and suggest that optimism effectively aids in coping with the disease in a more adaptive manner.28,30 Optimism is associated with increased subjective well-being,51 which translates into positive effects on patient behaviour and HRQOL.
As regards coping strategies, when strategies such as helplessness/hopelessness are used, we can predict decreased physical and social function. In addition, as the correlational analysis showed, helplessness/hopelessness and fatalism were negatively associated with the majority of the components in the SF-36 scale. On the other hand, we also observed that fighting spirit was associated with increased physical function, general health, vitality, and mental health, and decreased pain. In conclusion, and in agreement with previously published studies,7,30,36 we can affirm that active coping strategies (when the patient deliberately works to solve his/her problems through action) predict an increase in HRQOL, whereas passive coping strategies (when the patient does nothing to improve or resolve his/her problems, reacting with inhibition) predict a decrease in HRQOL.
As regards social support, the correlational analysis demonstrated that this component was associated with increased physical function, such that patients with greater social support find fewer limitations in the physical activity of their everyday lives. Remember that physical function was one of the dimensions of HRQOL that was most heavily deteriorated in our sample. This suggests the possible usefulness of promoting physical groups activities or activities geared towards generating social support.
As regards anxiety, the correlational analysis demonstrated that this factor was negatively associated with all dimensions of HRQOL. Several studies have pointed out the importance of mental health in chronic kidney disease. For example, patients on dialysis with a better perception of their mental health adapt better to disease and treatment progression.52 This suggests the relevance of implanting strategies for detecting depression/anxiety disorders in these patients, which would facilitate an improved HRQOL and clinical results.
The primary limitation of our study was the small sample size. However, our research protocol was proposed to all patients that complied with the inclusion criteria (45), and the majority of these accepted participation in the study (39). The main cause of the relatively small number of patients lies in our inclusion criteria based on age (equal to or younger than 55 years), which drastically reduced the potential pool of participants. The objective of this criterion was to ensure optimal comprehension of the psychological tests, and in this manner to achieve maximum validity of the results obtained. The impact of age on HRQOL is well documented, and so our results cannot be directly extrapolated to other age ranges. Another limitation could lie in the fact that we had no control group. Even so, our primary objective was to evaluate the possibility of predicting HRQOL using a series of psychosocial variables, and not to compare these variables between patients with renal disease and healthy subjects. Finally, we must keep in mind that our study was carried out within a multidimensional, biopsychosocial perspective, where health and disease are considered as the mutual interaction of several variables at many levels (bio-psycho-social), and can be explained through various levels of analysis. Picking up on these subtle relationships and mutual influences is a very difficult task. As such, the direction of causality may be interactive or inverse to that presented in this study.
To conclude, the results of our study suggest that intervention in several psychosocial aspects may be useful for improving HRQOL in renal patients. Firstly, given the fact that depression appeared as the primary predictor of HRQOL, our results demonstrate the need for evaluating (and treating, if necessary) the emotional state of renal patients (including states of anxiety or excessive worrying). This would have the impact of improving HRQOL and aiding the patient in adapting to the disease, thus facilitating a better prognosis and response to treatment. Depression was also negatively correlated with optimism and self-efficacy, variables that have been shown to correlate positively in our study with several aspects of HRQOL. In this context, we currently have several tools with demostrated effectiveness for simultaneously treating depression and improving optimism and self-efficay through cognitive behavioural therapy,53-55 which is known to lead to long-term improvements, decreased anxiety, and decreased apprehension. As regards social support, we might suggest implementing programmes for physical activity that are stimulated by social support networks (for example, involving a family member or creating patient groups for carrying out activities). Finally, our results also indicate an important role played by the coping mechanisms used in determining HRQOL. Any intervention in this context must be directed towards reducing the use of passive coping strategies (such as fatalism and helplessness/hopelessness) and increasing the use of active strategies. In this context, self-efficacy is associated with active coping strategies, and so interventions in this aspect can produce improved coping profiles.
Conflicts of interest
The authors have no potential conflicts of interest to declare.
Table 1. Sociodemographic and clinical characteristics of the study sample
Table 2. Mean and standard deviation for the different sub-scales of the SF-36
Table 3. Associations between the different components of health-related quality of life and predictive variables
Table 4. Results of the step-wise regression analysis for predicting the different components of quality of life