Dear Editor,
The chronic use of immunosuppressive agents is associated with the long-term risk of a wide variety of malignancies, including Kaposi’s sarcoma (KS), in renal transplant recipients compared with those of the general population. KS occurs after transplantation of 5 to 21 months and more commonly in males. The dose reduction or cessation of immunosuppresive drugs is the mainly approach for the treatment of KS in renal transplant patients, and switching calcineurin inhibitors to mammalian target of rapamycin inhibitors should be considered. Herein, we aimed to announce a 30-year-old male kidney transplant patient who had developed KS despite use of sirolimus after transplantation of 4 month and to the best of our knowledge this is the earliest onset case of KS after kidney transplantation.
CASE REPORT
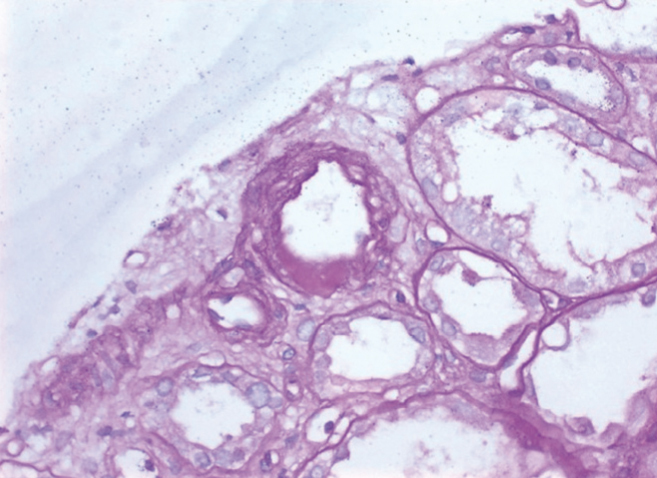
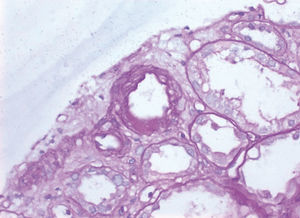
A 30-year-old male patient with end stage kidney disease received a cadaveric kidney transplant and discharged with a maintenance immunusuppresive therapy consist of the combination of prednisolone, tacrolimus and mycophenolic acide. The patient was hospitalized after transplantation of 10 week because of 2-fold increase in plasma levels of creatinine and diagnosed with calcineurin inhibitor nephrotoxicity based on renal allograft biopsy findings (Presence of nodular hyaline sclerosis in the arteriolar walls of kidney in biopsy and high blood levels of tacrolimus facilitate our ability to make diagnosis of calcineurin inhibitor nephrotoxicity) (Figure 1). Tacrolimus therapy was switched to sirolimus therapy. The patient had a purple red lesion located on the pretibial area of the left leg and diagnosed to be chronic dermatitis by dermatology. In the fourth month after transplantation the patient admitted to hospital because of progression of the lesion and lympedema on the left leg (Figure 2) and recent occurrence of bilateral lymphadenopathy. Paraaortic, parailiac and bilateral inguinal lymphadenopathies were detected by computer tomography imagination. Excisional lymph node biopsy was performed and reported as KS because of presence of spindle cells consistently stained for CD31 and CD34, and detection of HHV-8 latent antigen within those cells by immunohistochemical staining of biopsy specimen. Because of the high risk of acute rejection we did not consider to discontinue or reduce dosage of immunusppresive drugs and the patient was refered to oncology clinic for receiving chemotherapy due to rapidly progression of cutaneuos lesions. The inguinal lymphadenopathy disappeared with chemotherapy regimen that consist of combination of vinblastine and bleomycine but skin lesions persisted.
KS is an angioproliferative neoplasm characterized by reddish-brown or purple-blue plaques or nodules on cutaneous or mucosal surfaces, including the skin, lungs, gastrointestinal tract and lymphoid tissue. Due to high incidence of HHV-8, majority of cases of posttransplant KS has been reported in patients from Mediterranean, Jewish, Arabic, Carribean, or African descent.1,2 Recent advances in immunosuppresive era provide significant benefits in preventing acute rejection episodes in kidney allograft recipients (5). However, there is an increased risk of certain cancers as well as KS with use of long term immunusuppresant agents. The ennounced reports has revealed a time ranging from 5 to 21 months after transplantation for time of diagnosis of KS in those patients with kidney transplantation. In our case, KS has occurred in the 4th month of the kidney transplantation.
To the best of our knowledge, this is the earliest onset case of KS that has occurred after the 4th month of the kidney transplantation.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Figure 1. Arteriolar hyalinosis due to calcineurin inhibitor toxicity in a renal biopsy specimen.
Figure 2. The Kaposi&