To the Editor:
Distal renal tubular acidosis (DRTA) is an acid-base balance disorder defined by the inability of the kidneys to compensate for the production of acids from protein metabolism by eliminating them, due to decreased glomerular filtration (GF).
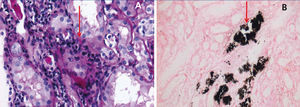
We report the case of a 33-year-old male patient with a history of hypokalaemia without study two years previously, who was admitted to the Emergency Department due to 10 days of progressive weakness in his limbs, fatigue, asthaenia and myalgia and he denied experiencing urinary symptoms. He self-medicated with potassium salts with no improvement, and as such he decided to seek medical assistance. On examination, he had blood pressure of 119/66mmHg, heart rate of 67 beats/minute, respiratory rate of 22 breaths/min, a temperature of 37°C, with 3/5 weakness in 4 limbs and diminished tendon reflexes. His laboratory tests on admission showed serum creatinine of 1.36mg/dl, serum sodium of 137mEq/l potassium of 3.2mEq/l, chloride of 114mEq/l, calcium of 8.8mg/dl, phosphorus of 3.5mg/dl, magnesium of 2.2mEq/l, bicarbonate of 19mEq/l, pCO2 of 30mmHg, venous pH of 7.36, lactate of 0.8mEq/l, serum albumin of 4.1g/dl, urine with a pH of 6.5 without glucosuria and urinary sediment with minimal erythrocyturia and leukocyturia, without nitrites or bacteria apparent in the microscope and proteinuria of 550mg/24 hours. We obtained a urine culture; normal complement levels, negative viral profile for human immunodeficiency virus and hepatitis B and C. A renal ultrasound was performed and there were hyperechogenic images suggestive of medullary calcification (Figure 1), calciuria of 4.2mg/kg/day, positive urinary anion gap (sodium of 58mEq/l, potassium of 16mEq/l, chloride of 23mEq/l), fractional excretion of potassium of 12%, fractional excretion of bicarbonate of 7%, but a urinary pH that failed to decrease to <5.5 over a period of more than 8 hours and reduction of the urinary gap, but without becoming negative (sodium of 47mEq/l, potassium of 12mEq/l, chlorine of 43mEq/l) after oral administration of ammonium chloride, and as such it was classified as distal renal tubular acidosis (DRTA) (type 1). The urine culture was negative and as such percutaneous renal biopsy was performed, which reported chronic tubulointerstitial nephritis with interstitial and intratubular nephrocalcinosis (Figure 2). The patient was therefore treated with 1mg/kg/day of prednisone and 1mEq/kg/day of potassium citrate. A week later, given a reduction in leukocyturia, immunological studies reported positive anti-nuclear antibodies, with a titre of 1:2560, positive anti-SSA and anti-SSB. We performed Schirmer’s test, which was positive, curiously without dry eye symptoms. In the outpatient follow-up after 16 weeks on 5mg/day of prednisone, the patient had creatinine of 0.88mg/dl and a decreased potassium salt requirement, maintaining normal levels of potassium, urinary pH at around 5, calciuria of 3.9mg/kg/day, negative urinary anion gap (sodium of 21mEq/l, potassium of 8mEq/l, chlorine of 47mEq/l), with the absence of leukocyturia, erythrocyturia and proteinuria.
Renal manifestations classified as renal tubular acidosis usually occur with a variable proportion between 3.6% and 73.1% in the series of patients with Sjögren's syndrome (SS) studied.1 Acute and/or chronic tubulointerstitial nephritis is the most common histopathological form in 54%-80% of cases.1-3
In DRTA, or type 1, hypercalciuria is usually multifactorial (release of bone calcium, suppression of the calcium-sensing receptor [CaSR], increased distal sodium load and acidosis), which along with alkaline urine and hypocitraturia favours calculi and nephrocalcinosis. Initially normal GF may decrease over time due to dehydration, nephrocalcinosis, obstructive calculi and/or infection.4,5
The objective of its treatment should be to normalise calciuria and citraturia to prevent nephrocalcinosis and progressive renal damage. As such, the underlying acidosis must be corrected.5 Nevertheless, this treatment is a palliative measure when its cause is secondary, such as in SS, where corticosteroids and cyclophosphamide have been used in accordance with the severity of renal involvement, with reports of stabilised renal function, a reduction in proteinuria and reversibility of various clinical manifestations deriving from renal tubular acidosis, therefore preventing the extension of nephrocalcinosis and reducing the risk of progression to end-stage chronic kidney disease.1,2. In our case, we used prednisone, which was gradually reduced, with a remission of clinical manifestations being achieved when the autoimmune tubulointerstitial nephritis deriving from SS was controlled.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Figure 1. Renal ultrasound with medullary hyperechogenicity suggestive of calcifications.
Figure 2. Renal histopathology showing tubulointerstitial lymphoplasmacytic infiltrate (A) and intratubular and interstitial nephrocalcinosis with Von Kossa stain (B). Images at 40X.