The Bajo Lempa is an impoverished rural coastal region of El Salvador affected by the chronic kidney disease (CKD) epidemic known as Mesoamerican nephropathy. The local community organisation Fondo Social de Emergencia para la Salud (FSES) (Emergency social fund for health) is helping to fight the epidemic in 42 communities of the region (19,223 inhabitants; average age 26.7 years; 48.5% male; 40.2% <18 years).
ObjectivesTo report annual rates of end-stage renal disease (ESRD) incidence and patient mortality in these communities during a 10-year period (2004–2013), and the prevalence of patients receiving renal replacement therapy (RRT) as of 31 December 2013.
MethodsThe FSES recorded new ESRD cases, basic patient history, form of RRT if received and patient deaths.
ResultsWe registered 271 new ESRD cases (annual average 27.1; 89% male; average age 55.6 years, four <18 years). Average annual ESRD incidence rate: 1409.8 per million population (pmp). Two-thirds did not report diabetes or hypertension. 94 patients (34.7%) received RRT: 58 in the Ministry of health, 26 in private services, 9 in social security and 1 in the military health system. 246 patients died (annual average 24.6 deaths; 89.4% male; average age 56.1 years; 92.3% at home). Average annual mortality rate: 128/100,000 population. Prevalence of patients receiving RRT in 2013: 1300.5pmp (N=25; 84% male; average age 51 years).
ConclusionsThis region has a high incidence of ESRD. Few receive RRT. Patient mortality is high even with RRT. Most patients are male (9:1). Social determinants influence the high mortality.
El Bajo Lempa es una región rural costera pobre de El Salvador afectada por la epidemia de enfermedad renal crónica (ERC) denominada nefropatía mesoamericana. La organización local comunitaria Fondo Social de Emergencia para la salud (FSES) colabora contra la epidemia en 42 comunidades de la región (19.223 habitantes; edad promedio 26,7 años; 48,5% masculino; 40,2% < 18 años).
ObjetivosReportar tasas anuales de incidencia de ERC terminal (ERCT) y de mortalidad de pacientes en estas comunidades durante 10 años (2004-2013), más la prevalencia de pacientes en tratamiento sustitutivo renal (TSR) al 31 de diciembre del 2013.
MétodosEl FSES registró casos nuevos de ERCT, sus antecedentes básicos, la modalidad de TSR recibida y sus fallecimientos.
ResultadosRegistramos 271 nuevos casos de ERCT (promedio anual 27,1; 89% masculino; edad promedio 55,6 años; 4 < 18 años). Tasa de incidencia de ERCT anual promedio: 1.409,8 por millón de población (pmp). Un 66% no reportaba diabetes ni hipertensión. Recibieron TSR 94 (34,7%) pacientes: 58 en el Ministerio de Salud, 26 en servicios privados, 9 en la seguridad social y uno en la sanidad militar. Fallecieron 246 (promedio anual 24,6; 89,4% masculino; edad promedio 56,1 años; 92,3% en su domicilio). Tasa de mortalidad anual promedio: 128/100.000 habitantes. Prevalencia de pacientes en TSR al 2013: 1.300,5 pmp (N=25; 84% masculino; edad promedio 51 años).
ConclusionesEn esta región la incidencia de ERCT es elevada. Pocos reciben TSR. La mortalidad es alta, aun con TSR. Son mayormente varones adultos (9:1). Los determinantes sociales inciden en la alta mortalidad.
Mesoamerican nephropathy (MeN) is an epidemic form of chronic kidney disease (CKD) of unknown origin that primarily affects adult males living on the Pacific coast of Central America and in southern Mexico.1,2 One of the affected areas is the Bajo Lempa region in Usulután, El Salvador,3–5 an impoverished rural coastal area at the estuary of the Lempa River. In El Salvador there are 5 healthcare providers: the Instituto Salvadoreño del Seguro Social (ISSS) [Salvadoran Social Security Institute] serves those with permanent employment and their families; the Comando de Sanidad Militar (COSAM) [Military Health Service] covers the military personnel; the Instituto Salvadoreño de Bienestar Magisterial [Salvadoran Institute for Teachers’ Welfare] serves public sector teachers; there are private services for those who can afford it; and, finally, the Ministerio de Salud (MINSAL) [Ministry of Health] provides free services to those without access to any of the above alternatives. In 2013, the closest facilities for renal replacement therapy (RRT) to the Bajo Lempa region were located in the city of San Miguel and in the capital, San Salvador at a distance of 75km and 90km, respectively.
The Fondo Social de Emergencia para la Salud (FSES) [Emergency Social Fund for Health] in the Tierra Blanca region in Usulután is a community initiative set up in 1994 in response to poor access to health services, a solidarity fund to improve the health of local residents and people in the surrounding communities in the Bajo Lempa region. Hundreds of families actively collaborate with the fund, which is enhanced thanks to charitable contributions. Even with limited resources, the FSES struggles for delivering basic health care visiting the sick, providing transportation for patients and promoting the recovery of self-esteem and dignity, and also provides education and promotion of health, and collaborates with MINSAL, non-governmental organisations and national and international voluntary organisations and programmes, conducting blood-donation and breast-screening campaigns and helping coordinate eye surgery, amongst other initiatives. According to the census of 2013, the 42 communities in the area covered by the FSES have 4795 households and a population of 19,223 people, 9890 (51.5%) females and 9333 (48.5%) males. The average age is 26.7±20 years and 7728 (40.2%) are under the age of 18. The most common occupation is agriculture (corn, beans, vegetables, sugar cane, etc.), on which the livelihoods of 79% of households depends. Also common are trade, fishing, prawn farming and salt extraction. Less than 5% have access to the ISSS because the men mostly work in agriculture and the women in household duties. Lastly, many of the inhabitants are people repopulated from other regions and repatriated from Nicaragua and Panama who were relocated after the end of the civil war in 1992.
The FSES started to face the epidemic of CKD in the region in 2001 and has been previously involved on research of the MeN.3,4 In 2003, samples from kidney biopsies obtained from patients with MeN were sent to the Puigvert Foundation in Barcelona, Spain, describing tubulointerstitial lesion with glomerulosclerosis, a finding that was later confirmed.6,7 The FSES has been conducting campaigns in the communities on early detection of CKD since 2004. It also runs a kidney-patient care programme and keeps a registry of these patients. Up to 2013, a total of 5371 serum creatinine tests had been performed on 3896 people, with 1043 cases of CKD diagnosed, mostly in early stages. Because there is not a nation registry of patients with kidney disease the real impact of the epidemic in this region is unknown. However, in this study, we present the results of the first 10 years of the FSES registry of patients with stage 5 CKD or end-stage renal disease (ESRD).
MethodsOur aim was to report the number of new cases of ESRD per year in this population (N). Information includes: demographic characteristics, medical history, the type of RRT they received and the number of deaths. The report includes the period from January first 2004 until 31st of December 2013. We defined the incidence of ESRD as the need for RRT (dialysis or transplantation)8 prescribed by a nephrologist or by any of the health service providers described. We recorded as death all patients diagnosed with ESRD who died from any cause after the need for dialysis had been prescribed or after being started. The direct causes of death were not registered.
Information was recorded at the time of the event for those who were under FSES medical care, and at the time of death for all others. The data were provided by the local residents, collected by FSES collaborators and compiled in Microsoft Excel sheets at the offices of the Tierra Blanca Center called “Monseñor Oscar Arnulfo Romero Centre”. Uncertain cases were visited and verified at home. We also recorded demographic data, such as age, gender and occupation, and basic medical history, such as a prior diagnosis of diabetes or hypertension. If the patient received RRT, we recorded the type, place and care provider. For deaths, we recorded the date and place. We also recorded the prevalence of patients receiving RRT on 31 December 2013 and the type of therapy. The results are expressed as mean±standard deviation or as percentages, as applicable. The incidence of ESRD and prevalence of RRT are reported number per million population (pmp) and the mortality as number of deaths per 100,000 population (pop).
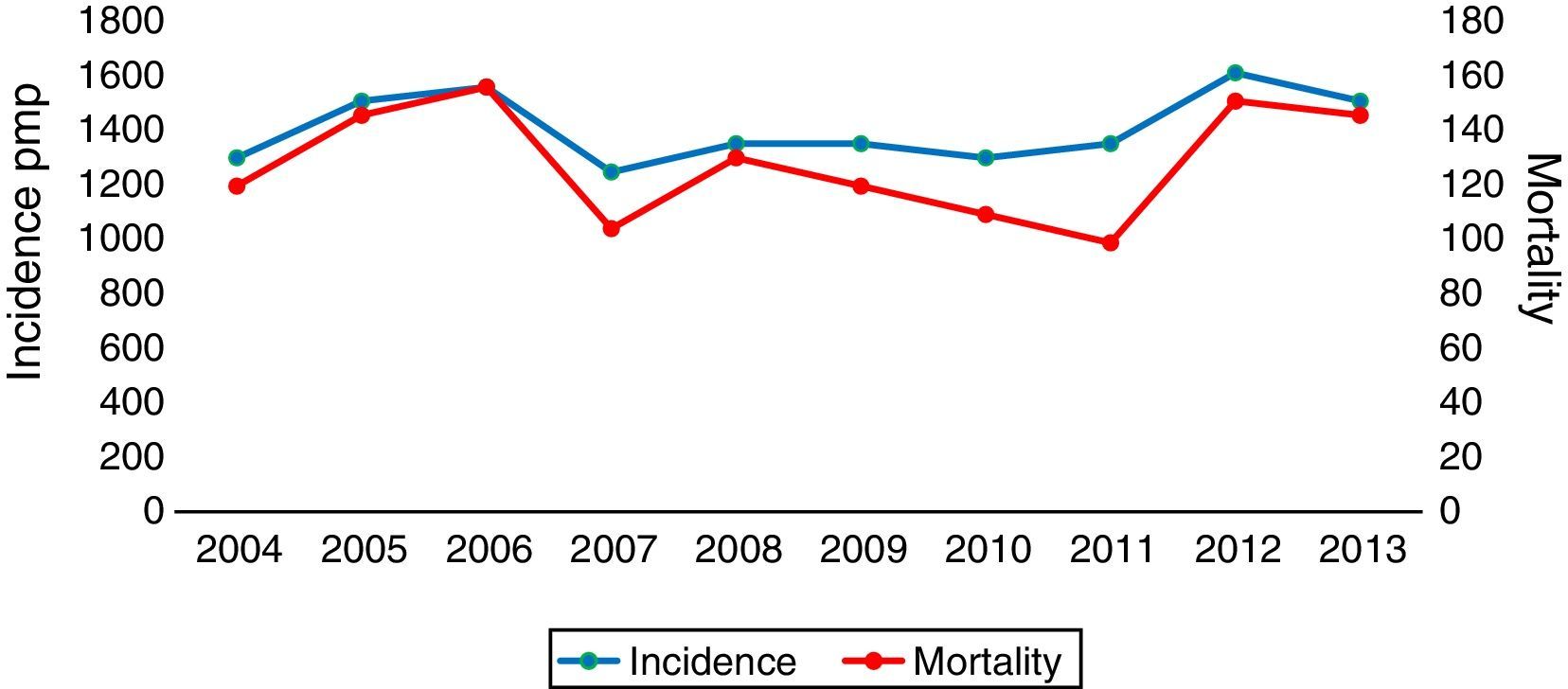
ResultsOver the 10-year period we registered 271 new cases of ESRD: 30 (11%) females and 241 (89%) males, with an average of 27.1±2.4 new cases per year. Age was recorded in 264 patients (97.4%), the average age was 55.6±15.5 years. Four (1.5%) were under the age of 18. The average annual incidence rate of ESRD for the 10-year period was 1409.8pmp. The annual incidence rates are shown in Fig. 1.
We registered the employment history for 196 cases (72.3%); a 75.5% worked or had worked in agriculture. Among men, 84.7% were farmers. Basic medical history for 165 (60.9%) cases revealed that 18.2% were diabetic and 29.7% hypertensive. In 66% of cases, there was no history of diabetes or hypertension and these were mostly men (97%) and 76% were farmers.
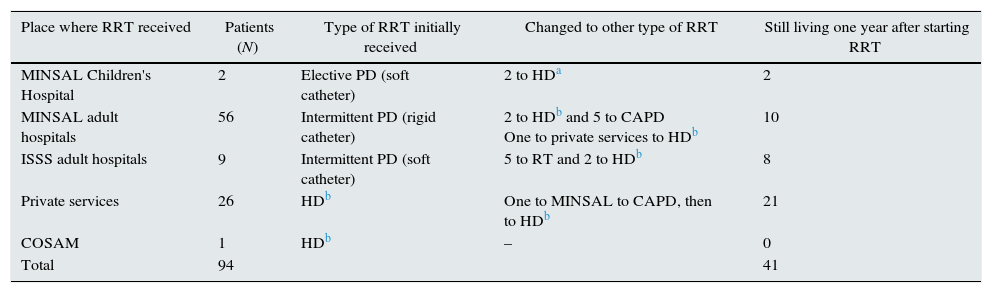
Out of the 271 patients with ESRD, 94 (34.7%) received some form of RRT and 177 (65.3%) were unable or unwilling to receive it. The average age of those receiving RRT was 51.9±14.2 years; eight (8.5%) were female and 86 (91.5%) male. One year after starting RRT, 41 (43.6%) of the 94 patients were still alive. The type of RRT received, the service provider and survival after year are shown in Table 1.
Renal replacement therapy (RRT) received by 94 patients with ESRD in the Bajo Lempa region from 2004 to 2013.
| Place where RRT received | Patients (N) | Type of RRT initially received | Changed to other type of RRT | Still living one year after starting RRT |
|---|---|---|---|---|
| MINSAL Children's Hospital | 2 | Elective PD (soft catheter) | 2 to HDa | 2 |
| MINSAL adult hospitals | 56 | Intermittent PD (rigid catheter) | 2 to HDb and 5 to CAPD One to private services to HDb | 10 |
| ISSS adult hospitals | 9 | Intermittent PD (soft catheter) | 5 to RT and 2 to HDb | 8 |
| Private services | 26 | HDb | One to MINSAL to CAPD, then to HDb | 21 |
| COSAM | 1 | HDb | – | 0 |
| Total | 94 | 41 |
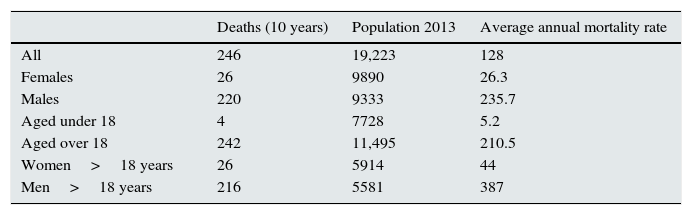
From year 2004 to 2013 246 (90.8%) of the 271 patients died: 26 (10.6%) females and 220 (89.4%) males, with an average of 24.6±4 deaths per year. The average age of those who died was 56.1±15.6 years. The annual mortality rates are shown in Fig. 1. The average annual mortality rate for the 10 years was 128×100,000pop. Table 2 shows the mortality rates by gender and for adults and under 18 years old.
Mortality rates per 100,000 population of patients with ESRD in the Bajo Lempa region, 2004–2013.
| Deaths (10 years) | Population 2013 | Average annual mortality rate | |
|---|---|---|---|
| All | 246 | 19,223 | 128 |
| Females | 26 | 9890 | 26.3 |
| Males | 220 | 9333 | 235.7 |
| Aged under 18 | 4 | 7728 | 5.2 |
| Aged over 18 | 242 | 11,495 | 210.5 |
| Women>18 years | 26 | 5914 | 44 |
| Men>18 years | 216 | 5581 | 387 |
Out of the 246 deaths, 227 (92.3%) occurred at home, 12 (4.9%) in MINSAL hospitals, one while being transported to a hospital, one in a private clinic and one in an ISSS clinic; information was not available in four deaths.
On December 31st 2013, 25 of the patients were alive on some type of RRT; four (16%) females and 21 (84%) males, average age 51±12.9 years, with a prevalence rate of patients on RRT of 1300.5pmp. The patients on RRT who were still alive by the end of 2013 were: five patients who received kidney transplantation through the ISSS between 2006 and 2008; 14 patients on restricted haemodialysis (1 through MINSAL, 2 through the ISSS and 11 in private services); and six patients on peritoneal dialysis (PD) through MINSAL, of whom 3 had recently started intermittent PD (IPD) with rigid catheter and three had managed to move on from rigid catheter IPD to continuous ambulatory PD (CAPD).
DiscussionTo our knowledge, this is the first study on incidence, mortality rates and prevalence in patients with stage 5 CKD or ESRD conducted specifically in a MeN-epidemic region. Yet, the characteristics we found are very similar to previous reports by other studies in the same region, but including patients with all stages of CKD.3–5 The disease is more common in adult males (male-to-female ratio 9:1) of productive age (55 years). Many are farmers (75.5%) and only one third had a previous diagnosis of diabetes or hypertension, classic causes that might explain the kidney damage. This may be due to the epidemic of MeN in the region, which mostly affects adult male farmers,1–5,9,10 poor access to diagnosis and control of the classic causes of ESRD, or both.
The sustained high annual incidence of ESRD rates registered in this Bajo Lempa population over this 10-year period (average 1409.8pmp) is 7 fold increased as compared with the average Latin American rate of incident RRT patients (190.8pmp).11 Despite the poverty of the region and the poor access to RRT, the prevalence of patients on RRT as of 31 December 2013 (1300.5pmp) is also higher than that of Spain12,13 and almost double the Latin American average (660.3pmp).11 This high number of patients could also be due to the reasons previously mentioned.
Of the 271 incident patients, initially only 35 (12.8%) had access to modern RRT through the ISSS or private services: the greatest burden of patients fell on the MINSAL, where IPD with rigid catheter is offered initially and there is no transplantation programme for adults. In recent years, MINSAL has improved the quantity and quality of their RRT provision and five of these patients were helped at some point from the recent introduction of CAPD at Hospital de San Miguel. However, the annual mortality rates have not changed and they are on average (128×100,000pop) 10 times higher than those reported by other countries in the Americas which, with the exception of neighbour Nicaragua, also affected by the MeN epidemic,1,2 do not usually exceed 13×100,000pop.14 Notably, the average annual mortality rate for adult males alone (387×100,000pop) is 30 times that figure. The world needs to start paying attention to this silent slaughter that has remained hidden for decades,9,10 overshadowed as it has been by the poverty of the affected regions and the lack of official registries.
The social determinants of health, particularly gender, poverty and lack of information, play an important role in the high mortality rate among these patients. In relation to gender, we have previously commented on the fact that in this region there is an unusual reverse gender discrimination against males in terms of access to health services,3 possibly bound by the prioritisation of scarce resources to care for women and children, while the MeN epidemic primarily affects adult males.1–7,9,10 Indeed, when we breakdown the incidence, prevalence and mortality rates by age and gender, it is clear that these are not high for either women or children; the marked increase in all rates is pushed up by large numbers of adult male patients. In relation to poverty and lack of information, two thirds of the patients (65.3%) were either unable or unwilling to receive RRT. When asked about the reasons why they did not seek or rejected the RRT, the most common responses from patients and their families were that they did not have the financial resources to pay for transportation to the medical centres and that, based on previous experiences with relatives and neighbours, they considered that either way the disease is fatal, but “the dialysis (peritoneal with rigid catheter) kills them faster”. For this reason, many people are reluctant to have their serum creatinine checked and even prefer not to know if they are in early stages of CKD. This complicates early detection and appropriate nephrology control. The few patients who had permanent employment and, therefore, access to the ISSS or were financially able to afford private services, did have access to transplantation or modern dialysis techniques and, as a result, had better survival; all transplanted patients and over half of those receiving haemodialysis were still alive and were included in the RRT prevalence as of 31 December 2013. In contrast, the poorest, generally agricultural labourers with no access to ISSS or private services, died without receiving any RRT (65.3%) or sought free assistance through MINSAL (21.4%), where the incidence and mortality rates were almost equal for virtually all those who were treated with IPD with rigid catheter, regardless of the cause of their ESRD, whether classic (diabetes, hypertension) or not (MeN).
Importantly, because of these social determinants, MINSAL attends mainly agricultural workers and not other patients working in other occupations who seek care though the ISSS or private services. In addition, almost all patients (92.3%) died in their homes and therefore were not registered by the MINSAL hospital surveillance systems. For these reasons, official data may be underestimating the true extent of the epidemic and showing a preference towards agricultural occupations.
For more than a decade, the FSES has worked hard in the community and in recent years, MINSAL has implemented initiatives to address the epidemic, but they are not yet sufficient. With poor access to RRT, prevention and early detection become more important. We need to disseminate information, a message of hope for people not to be afraid to have themselves checked in the early asymptomatic stages so they can access nephroprotection programmes earlier, but we also need to improve RRT options and bring them closer to the people, in order to increase quality of life and survival for those who could not be diagnosed in time.
LimitationsWe recognise that this community registry could be incomplete and we may have not covered all deaths. In addition, because there is no previous data, it is very possible that we are overestimating the population when calculating rates and that these rates are somewhat higher than reported. We should also point out that, by not having the previous medical history for a third of the patients, the characteristics described may vary and so should be interpreted with caution.
Conflict of interestsThe authors declare that they have no conflicts of interests.
Please cite this article as: García-Trabanino R, Hernández C, Rosa A, Domínguez Alonso J, en nombre del Fondo Social de Emergencia para la Salud (FSES) del cantón Tierra Blanca, departamento de Usulután, El Salvador. Incidencia, mortalidad y prevalencia de enfermedad renal crónica terminal en la región del Bajo Lempa, El Salvador: 10 años de registro comunitario. Nefrología. 2016;36:517–522.