Aunque la frecuencia de la enfermedad coronaria (EAC) en los pacientes en diálisis se estima muy elevada, existe una gran variabilidad en los estudios en la tasa de infarto agudo de miocardio (IAM). Objetivo: Establecer la incidencia IAM y analizar sus características y repercusión en la evolución de los pacientes incidentes en diálisis. Métodos: Estudiamos los pacientes incidentes en diálisis entre el 1/1/1999 y el 31/12/2007, y analizamos la presentación del primer IAM en diálisis. Valoramos diagnósticos previos de diabetes, hipertensión arterial, EAC (IAM o lesiones en coronariografía), accidente cerebrovascular isquémico, arteriopatía periférica avanzada y tabaquismo. Se analizaron urea, creatinina, hematocrito, calcio/fósforo, hormona paratiroidea intacta, lípidos y albúmina. El seguimiento fue hasta trasplante, muerte, pérdida o cierre del estudio el 31/12/2010. Resultados: De 576 pacientes incluidos (64,6 ± 16 años; 24,7% diabéticos; 82,3% hemodiálisis/17,7% diálisis peritoneal), 34 (5,9%) tenían diagnóstico previo de EAC. En un seguimiento de 40,2 ± 32 meses (1931,5 pacientes-año [pac-año]), 40 (6,9%) presentaron IAM. La incidencia fue de 2,13/100 pac-año. En los pacientes sin diagnóstico de EAC fue de 1,84/100 pac-año, y de 7,53/100 pac-año en aquéllos con diagnóstico previo de EAC. De los 40 IAM, 15 fueron con elevación de ST (incidencia 0,79/100 pac-año) y 25 sin ella (incidencia 1,33/100 pac-año). Los factores predictores de presentación del IAM en diálisis fueron la edad superior (odds ratio [OR]: 1,037; intervalo de confianza [IC] 95%: 1,009-1,067; p = 0,011), la EAC previa (OR: 3,35; IC 95%:1,48-7,16; p = 0,004) y la diabetes como causa de nefropatía (OR: 2,96; IC 95%: 1,49-5,86, p = 0,002). La mortalidad hospitalaria fue del 30% de los pacientes, 72,5% en el primer año y 82,5% en el segundo. El 80% de los pacientes a los que se efectuó coronariografía presentaban enfermedad de más de un vaso. Conclusiones: La incidencia del IAM en los pacientes que inician diálisis es muy elevada, y en los que empiezan diálisis con diagnóstico de EAC documentada es tres veces más elevada. La mortalidad posinfarto es muy alta y la enfermedad multivaso muy frecuente.
Background: Although the estimated frequency of coronary artery disease (CAD) in patients on dialysis is very high, there is considerable variation in the studies published to date regarding the rate of acute myocardial infarction (AMI) in these patients. Objective: To establish the incidence of AMI and to analyse the characteristics and consequences of this entity on the clinical progression of incident dialysis patients. Methods: We recorded AMI in the patients treated in our dialysis unit between 01/01/1999 and 31/12/07. The variables assessed were: prior diagnosis of diabetes, hypertension, CAD (AMI or lesions observed in coronary angiography), ischaemic cerebrovascular accident, advanced peripheral artery disease (PAD), atrial fibrillation and tobacco use. Biochemical analyses included: urea, creatinine, haematocrit, calcium, phosphorous, iPTH, lipids and albumin. Follow-up lasted until transplant, death, loss to follow-up or study end in Dec. 2010. Results: Of the 576 patients recruited (aged 64.6±16 years), 24.7% had diabetes, 82.3% were on haemodialysis (17.7% on peritoneal dialysis), and 34 (5.9%) had a previous diagnosis of CAD. In a follow-up lasting a mean of 40.2±32 months (1931.5 patient-years), 40 patients (6.9%) suffered an AMI. The incidence was 2.13/100 patient-years. The patients without CAD had an incidence of 1.84/100 patient-years and those with a previous diagnosis of CAD had an incidence of 7.53/100 patient-years. In 22.5% of patients, AMI happened in the first 3 months of dialysis, and 37.5% in the 1st year. Of the 40 AMI, 15 were with ST-segment elevation (incidence: 0.79/100 patient-years) and 25 were non ST-segment elevation (incidence: 1.33/100 patient-years). The factors that predicted the occurrence of AMI in dialysis were older age (OR: 1.037; 95% CI: 1.009-1.067; P=.011), previous CAD (OR: 3.35; 95% CI: 1.48-7.16; P=.004), and diabetes as a cause of nephropathy (OR: 2.96; 95% CI: 1.49-5.86; P=.002). In-hospital mortality was 30%, with 72.5% of deaths occurring in the 1st year and 82.5% in the 2nd; 80% of the patients who underwent a coronary angiography had multi-vessel disease. Conclusions: The incidence of AMI in incident dialysis patients is high. In previous coronary disease patients, the incidence is 3-fold higher. Post-infarction mortality is very high and multi-vessel disease is very frequent.
INTRODUCTION
Acute myocardial infarction (AMI) in patients on dialysis conveys a very poor prognosis, with more than half of all patients dying within the first year after occurrence.1,2 However, a precise evaluation of the contribution of AMI to the already high mortality in patients on dialysis is difficult, since the majority of studies analysing the incidence of AMI come from general patient registries,3 not studies designed for examining AMI in dialysis patients,4,5 with imprecise definitions of AMI as specific events,6,7 and in which data regarding clinical management and long-term follow-up are not available.7 Often, only patients who survive the first 90 days after the start of dialysis are included, which can lead to an underestimation of the incidence of AMI through ignoring those events that occur in the initial stages of renal replacement therapy.8 This produces wide variability between the results of different studies, hampering a true evaluation of the impact of AMI in the evolution of patients commencing chronic dialysis programmes for the first time.
The objective of this study was to analyse the incidence of AMI in the evolution of patients that start dialysis for the first time from the day they were included in the programme, the different forms in which AMI are manifested, the factors associated with AMI, and immediate and long-term post-infarction patient evolution.
METHODS
We included all patients diagnosed with stage 5 chronic kidney disease (CKD) that started dialysis (haemodialysis or peritoneal dialysis) between 01/01/1999 and 31/12/2007 at our hospital, which covers the nephrological health care for a population of 664 742 inhabitants in 2007, 17.9% of which are 65 years or older. All patients diagnosed with stage 5 CKD are treated with renal replacement therapy at our hospital, and afterwards, using criteria based on hospital organisation and the geographical location of each patient, patients either remain on dialysis at our hospital or are transferred to one of three peripheral dialysis units within the health region. The hospital receives all patients that require hospitalisations during the course of their evolution.
We excluded patients that had started dialysis treatment at another hospital, had previously received a transplant, or that recovered renal function to the degree that dialysis was no longer required.
Ours was a longitudinal, ambispective, observational study. Patients were monitored from the first day of dialysis until removal of the patient from dialysis due to transplantation, death, patient transfer out of our health region, or the end of the study on 31/12/2010.
We recorded the occurrence of the first AMI (index) during the patient’s time on dialysis, as well as all factors associated with the AMI. The variables analysed included: demographic characteristics, diagnosis of diabetes, arterial hypertension, tobacco use, coronary artery disease (CAD), stroke, advanced peripheral artery disease, or atrial fibrillation (AF) prior to inclusion in dialysis. During the first month on dialysis treatment, we measured: haematocrit, urea, creatinine, total cholesterol, triglycerides, calcium, phosphorous, intact parathyroid hormone, and albumin.
We recorded the moment of the first AMI in reference to time on dialysis, patient survival following the event, and hospital mortality after 1 month, 1 year, and every year afterwards.
We assessed the presentation of AMI using an electrocardiogram (ECG), with or without ST-segment elevation or left branch block.
Definitions
Documented coronary artery disease: history of AMI or a coronary angiography demonstrating lesions of the epicardial arteries >70%.
AMI: episode of acute thoracic pain accompanied by acute electrocardiographic alterations or curve indicating myocardial damage.
Time to AMI: time between the first dialysis session and the first AMI, or the occurrence of transplantation, death, loss of follow-up or end of the study.
Ischaemic cerebrovascular accident: persistent focal neurological deficit lasting more than 24 hours, excluding haemorrhage, measured using computerised axial tomography or magnetic resonance through image analysis or neurological report. Transient ischaemic attack was not included in this category.
Advanced peripheral artery disease: arteriopathy of the lower limbs in La Fontaine stage IV, severe ischaemia or amputation of the lower limbs due to causes not related to trauma, cancer, or vasculitis.
AF: a diagnosis of AF was made when arrythmia was present in the patient evaluation at the start of dialysis or when prior ECG results documented it. In this case, any episode documented in the ECG during the patient’s evolution was recorded as AF. An ECG was taken at the start of dialysis, every year, and whenever clinical circumstances indicated one.
Diabetes: diagnosis of diabetes with indications for pharmacological treatment at any time during the patient’s evolution, before or after entering the dialysis programme.
Arterial hypertension: indications for hypotensive medication in order to achieve blood pressure values <140/90mm Hg.
Tobacco use: active smoker within the 10 years preceding the start of the dialysis programme.
Modality of renal replacement therapy: registered as the dialysis technique used by the patient at the end of the first month of the treatment programme. When the technique was changed, any events that occurred during the first month of treatment were assigned to the previous type of treatment.
The study received the approval of the Research Ethics Committee of Jaen.
Statistical analysis
We used Student’s t-tests or non-parametric Mann-Whitney U-tests to compare means. For comparisons between qualitative variables, we used Pearson’s χ2 tests. We also performed a multivariate analysis using logistic regression to establish the relationship between AMI and factors considered for predictive value. The target prognostic variable was the development of an AMI during the follow-up period. The study was based on an analysis of predictive variables at the start of treatment through a Cox proportional hazards regression analysis. We included all possible variables, and obtained odds ratios (OR) and 95% confidence intervals (CI) for each.
We also performed a survival analysis using the Kaplan-Meier method, and compared survival curves using the Mantel-Haenszel test (long-rank). For null-hypothesis tests, a P-value <.05 was considered statistically significant. All analyses were carried out using SPSS software, version 15.0, for Windows.
RESULTS
Patients
A total of 669 patients were included on dialysis treatment during the study period. We excluded 123 patients from this population (17.5%). The causes for exclusion were: 55 (7.9%) had a previous transplant, 27 (3.8%) had started dialysis at other centres, 19 (2.7%) recovered renal function, and 22 (3.1%) died or left our health region before it could be established whether the patient suffered from stage 5 CKD or a reversible decompensation of previous CKD. The remaining 576 patients were included in our analysis.
The causal nephropathies for CKD were: glomerulonephritis: 16.7%; interstitial nephropathy: 14.2%; diabetes: 17.7%; nephroangiosclerosis: 13.2%; systemic disease: 8.9%; polycystic kidney disease: 6.5%; familial nephropathy: 1.9% unknown: 19.4%; and other: 2.3%. Diabetes as the cause of nephropathy or as a concomitant disease was present in 142 (24.7%) patients. A total of 474 (82.3%) patients were treated with haemodialysis and 102 (17.7%) were treated with peritoneal dialysis.
Mean patient age at the start of dialysis was 64.5±16 years, and the median age was 69.2 years. A total of 322 (55.9%) patients were male. The mean age of patients on haemodialysis was 66.01±15 years, and the mean age of patients on peritoneal dialysis was 57.8±18 years (P=.000).
The mean follow-up period was 40.2±32 months, and the median was 35.4 months, with 25th and 75th percentiles of 13.2 months and 59.9 months, respectively, representing a total follow-up of 1931 patient-years.
Incidence of acute myocardial infarction patients during the course of treatment
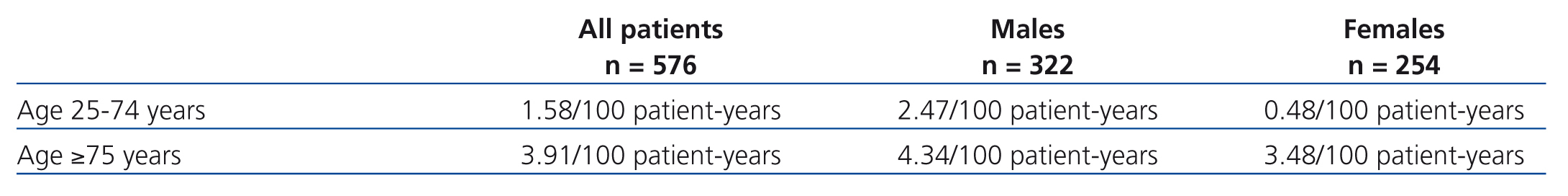
While on dialysis, 40 patients suffered one or more AMI. The incidence was 2.13 AMI/100 patient-years of follow-up. Of these, 29 were men (9% of men), yielding an incidence of 2.81 AMI/100 male-years of follow-up. Only 11 occurred in women (4.3% of women), with an incidence of 1.29 AMI/100 female-years. Table 1 displays the incidence of AMI based on age and sex.
Seven (17.5%) of the patients that suffered AMI during dialysis had a prior diagnosis of CAD, all in the form of AMI. The incidence of AMI while on dialysis in these patients was 7.53 AMI/100 patient-years. The other 33 patients that suffered AMI while on dialysis had no prior diagnosis of coronary disease. The incidence of de novo AMI in these patients was 1.84 AMI/100 patient-years.
Thirty-seven of the patients that suffered an AMI while on dialysis were treated using haemodialysis, with an incidence in these patients of 2.44 AMI/100 patient-years. Three patients on peritoneal dialysis suffered an AMI, with an incidence of 0.81/100 patient-years.
Six patients (15%) suffered their AMI during the first month on dialysis. At the end of the first year, 15 patients (37.5%) had suffered AMI, 5 of which had a prior diagnosis of CAD.
Type of presentation of the acute myocardial infarction during dialysis treatment
1. AMI with ST-segment elevation: 15 (37.5%) of the first 40 AMI during dialysis involved ST-segment elevation. The incidence of this type of AMI was 0.79/100 patient-years. Three of these had a prior diagnosis of CAD. The incidence of AMI with ST-segment elevation in patients with a prior diagnosis of CAD was 3.22AMI/100 patient-years. In those without a prior diagnosis of CAD, the incidence was 0.6/100 patient-years.
2. AMI without ST-segment elevation: 25 (62.5%) of the first AMI on dialysis were without ST-segment elevation. The incidence of this type was 1.33 AMI/100 patient-years. Four were previously diagnosed with CAD, and the incidence in this population was 4.3 AMI/100 patient-years. In those that did not have a prior diagnosis of CAD, the incidence was 1.17/100 patient-years.
Factors related to the type of acute myocardial infarction produced during patient evolution while on dialysis
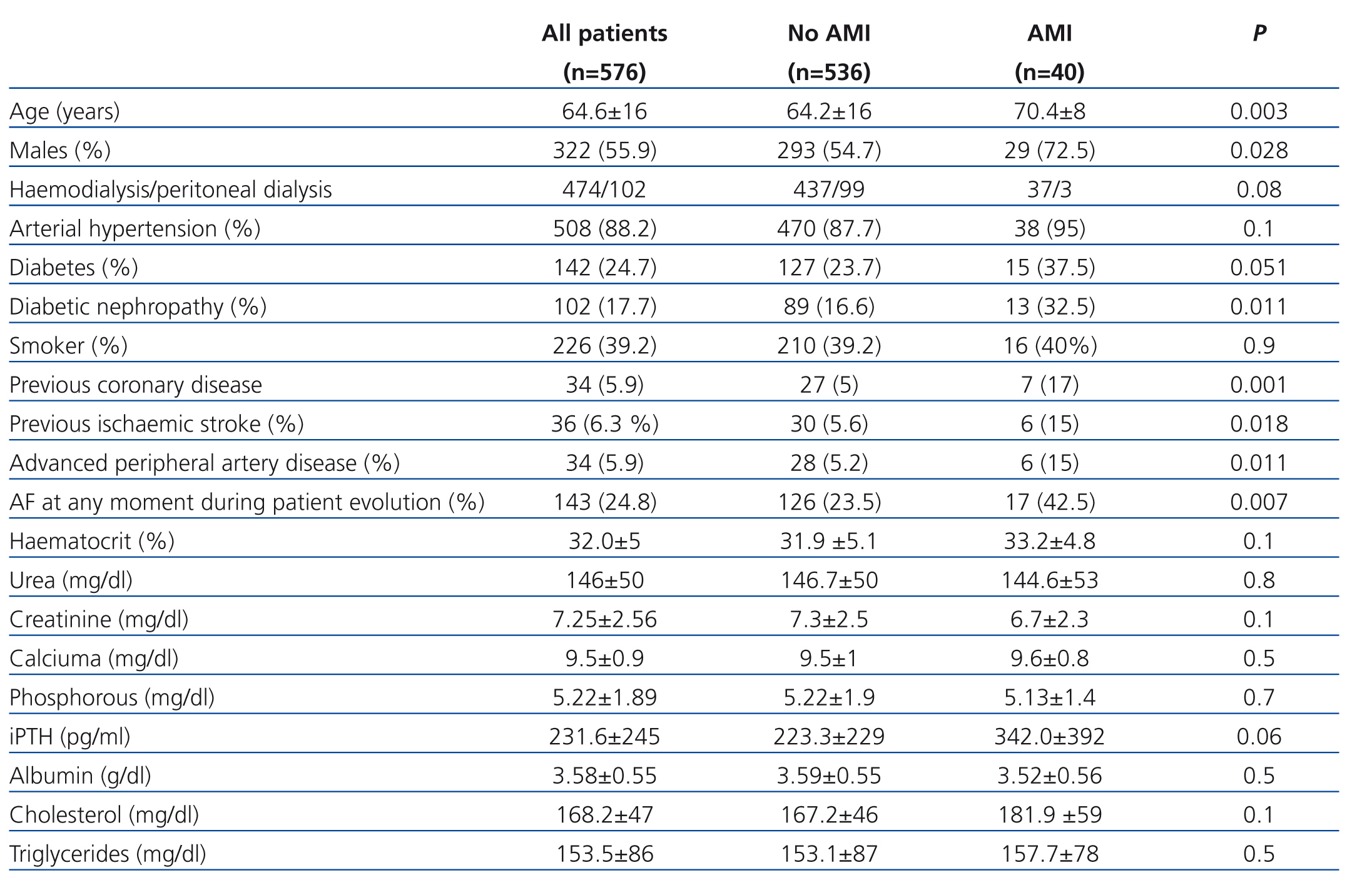
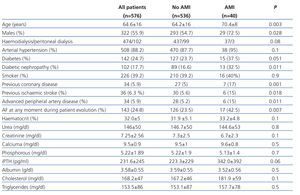
Patients that suffered an AMI were older, had a higher proportion of males, and tended to have diabetes as the cause of nephropathy. A higher proportion also had a prior diagnosis of cerebrovascular accident, peripheral artery disease, or AF at some point during their evolution, and in any form. Table 2 summarises the characteristics of all of the study variables.
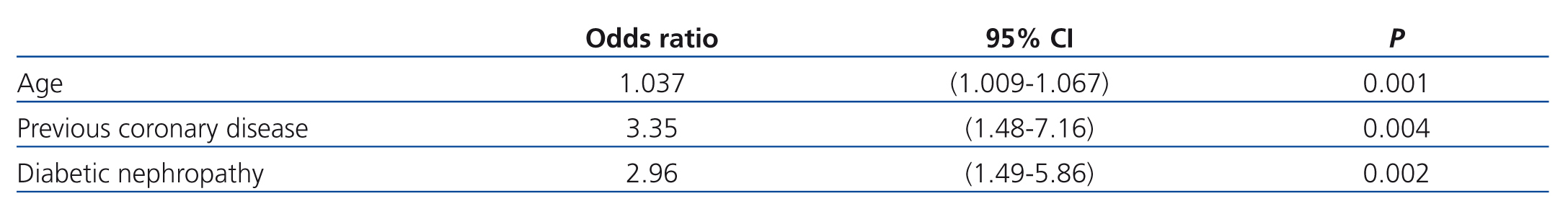
In the Cox proportional hazards multivariate regression analysis, the factors selected for predicting an AMI while on dialysis were: old age, CAD diagnosed before starting dialysis, and diabetes as the cause of nephropathy (Table 3).
The predictive factors for an AMI in the 542 patients that started dialysis without a previous diagnosis of coronary disease were: old age (P=.044 OR: 1.032; 95% CI: 1.001-1.064), lower albumin (P=.033; OR: 0.451; 95% CI: 0.218-0.936), and diabetes as the cause of nephropathy (P=.011; OR: 2.636; 95% CI: 1.244-5.584).
Patients that suffered an AMI without ST-segment elevation were older than those that suffered an AMI with ST-segment elevation, although this difference was not statistically significant. Other relevant parameters, such as diabetes, previous CAD, and AF, were similar between these two sub-groups.
Diagnostic angiography and revascularisation
A total of 15 patients (37.5%) underwent coronary angiography. Twelve had more than one affected vessel: 3 patients had 2 vessels and 9 patients had 3. Revascularisation was complete in 4 patients: in the 3 that had only one vessel affected and in 1 with 2 affected vessels. In the remaining 11 patients, revascularisation was only partial in 7 and not possible in 4.
Survival on dialysis and mortality
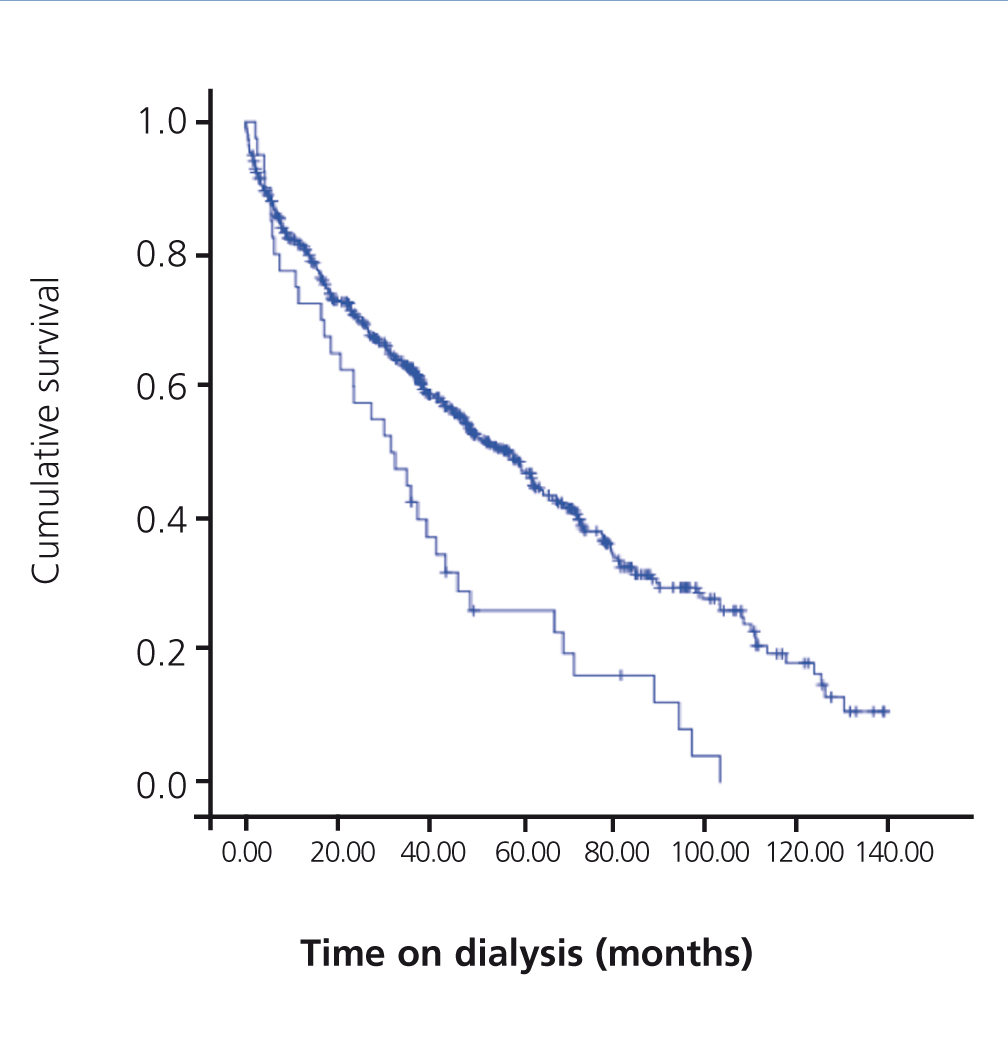
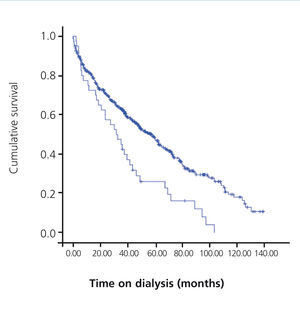
Of the 40 AMI patients on dialysis, 36 died during the follow-up period (Figure). One patient received a transplant and 3 remained on dialysis at the end of the study.
Twelve patients (30%) died in the hospital following the AMI, and 6 during the first month: 45% of all patients that suffered an AMI. The mortality rate after one year was 72.5% (29 patients), and was 90% after 5 years (36 patients).
Mean post-AMI survival was 10.8 months, and the median was 2.57 months.
A total of 29 of the 36 patients (80.5%) died from cardiovascular causes, 21 (58%) due to the AMI, and 8 due to other cardiovascular causes: three cerebrovascular accidents, three cases of sudden death, one arterial ischaemia of the lower limbs, and one mesenteric ischaemia. Four patients died due to infections, two from gastrointestinal causes, and one from cachexy.
DISCUSSION
The results of our study demonstrate the high incidence of AMI in CKD patients that start dialysis for the first time. This incidence is tripled in patients who start dialysis with a previous diagnosis of CAD as documented in the form of a prior AMI or findings in a coronary angiography. In-hospital and long-term mortality rates are very high, and multi-vessel disease is very common.
Despite the well-known high prevalence of cardiovascular disease in its various manifestations among patients on dialysis,9-11 few clinical studies have analysed the incidence of AMI in the evolution of patients in this position. In addition, the majority of these studies come from general patient registries or administrative records.3,5 In an analysis of the USRDS registry, the hospitalisation rate for acute coronary syndrome was 2.9/100patient-years.12 In a later analysis of the same registry, the incidence of AMI was approximately 5% per year,5 and in patients without a diagnosis of cardiovascular disease, the rate was 4.29/100 patient-years.13 In the HEMO study, the incidence of hospitalisation for a first AMI while on dialysis was 3.3/100 patient-years.4 These incidence rates are higher that we observed in our study, although the lower prevalence of diabetes and older age of our patients makes comparison difficult. In the European population, in a study by the Necker Hospital in Paris, the incidence of AMI in patients on dialysis with an age ≥65 years was 2.99/100 patient-years,14 similar to our results. In a study of Japanese patients on dialysis, the incidence of de novo AMI was 1.43/100 patient-years, with a similar prevalence of diabetes to that observed in our study, but a somewhat lower mean patient age.15 It is well known that the incidence of coronary events in the general population varies widely by geographic location, with differences that can be as much as five-fold lower in Mediterranean countries as compared to northern Europe.16 These differences in the incidence of atherosclerotic events in the general population also exist in patients on dialysis, with similar increases in the risk of events to those of the general population from which each patient originates, as has been observed in other anatomical regions.17-19
Although our incidence of AMI is lower than others reported for patients on dialysis, it is still higher than in the general population in Spain, which has one of the lowest rates in the world. According to the results from three populational studies: MONICA-Catalonia, REGICOR, and IBERICA, in 2002, the rate of hospitalisations due to AMI (77.6% of all AMI) for patients aged 25-74 years was 0.15/100 patient-years in males and 0.03/100 patient-years for females. For the population aged ≥75 years and hospitalised for AMI (41% of all AMI in this age range), the rate is 0.61/100 patient-years in males and 0.34/100 patient-years for females.20 These results allow us to appreciate the fact that the incidence of AMI in our population on dialysis is 16 times higher for men and women younger than 75 years, and 7 and 10 times higher in the population older than 75 years, for males and females, respectively.
The independent risk independent of the type of AMI in our patients were those typically found to be associated with a greater risk of atherosclerotic events in the general population, and are more common in patients on dialysis.21 Each year increase in age implied an increase in the risk for an AMI of approximately 3.7%.
Diabetes, which is a risk factor for ischaemic heart disease in the general population and in patients on dialysis, was also a significant predictor in our patients, although only in those in which this pathology was attributed as the cause of their entry into dialysis. In our study, diabetes was only considered if requiring pharmacological treatment, thus excluding situations of intolerance to carbohydrates. It is possible that vascular damage would be different if diabetes was considered to be the cause of the kidney disease or as a concomitant pathology.
The probability of suffering an AMI was three times higher in patients that started dialysis with a diagnosis of CAD as compared to those without objective evidence of this pathology. In a study of acute coronary syndrome in patients on dialysis, a prior history of cardiovascular disease increased the frequency of AMI by more than two-fold,13 and ischaemic heart disease as evidenced by a previous history of AMI or unstable angina were risk factors for suffering an AMI.8,22
Fifteen percent of the first AMI to occur after starting dialysis were produced in the first month of treatment, and almost 40% in the first year. In the USRDS registry, AMI occurred in the early phase of dialysis treatment, with 29% of cases occurring in the first year, and 52% in the second.1 Our results demonstrated a tendency towards a higher probability of AMI in the first year, although this was not substantially higher than in other time periods; perhaps a greater sample size would have produced results more similar to those of the USRDS study.
In a registry of AMI, the proportion of AMI with ST-segment elevation was significantly lower in patients on dialysis.3 In our study, the distribution of electrocardiographic types of AMI was similar to that of the population not on dialysis, with a greater frequency of AMI without ST-segment elevation (62.5%).23,24 It has also been described that individuals from the general population diagnosed with AMI with ST-segment elevation have greater comorbidity, older age, and a higher frequency of a prior diagnosis of ischaemic heart disease.25 In our study, no significant differences existed between AMI patients with or without ST-segment elevation, although the small sample size impedes drawing any definitive conclusions.
In-hospital mortality in our study was 30%, approximately 3-5 times higher than in the general population in Spain,26,27 and somewhat higher that the in-hospital mortality rate reported by the USRDS registry of patients on dialysis, possibly due to the fact that events that occurred in the initial phases of dialysis were not registered in this study. The mortality rate 5 years after the AMI of approximately 90% observed in our study was similar to that of the USRDS registry.1 The cause of death was cardiac-related in 66% of patients.
Coronary angiography was used in 15 patients (37.5%), a much lower rate of use than in the general population in Spain21 and the rates produced by the current procedural protocols in our hospital.24 The results showed that 60% of these patients had multi-vessel disease, as opposed to approximately 17% found in the population not on dialysis.21 Complete revascularisation was possible in only 4 of the 15 patients who underwent the procedure. Despite the limitation presented by the small sample size of our study, this confirms the well-known under-utilisation of invasive therapeutic and diagnostic measures in patients on dialysis.3,28
To conclude, the incidence of AMI in the population on dialysis is very high. The risk factors and electrocardiographic types of AMI were similar to the population not on dialysis. The high in-hospital mortality rate in these patients contributes heavily to the low survival rate and frequent cardiovascular death in patients on dialysis.
Conflicts of interest
The authors have no conflicts of interest to declare.
Table 1. Incidence of acute myocardial infarction patients during dialysis treatment based on sex and age
Table 2. Characteristics of the patients that developed acute myocardial infarction while on dialysis
Table 3. Predictive factors for the development of acute myocardial infarction during dialysis. Multivariate analysis. Cox regression analysis.
Figure 1. Survival of acute myocardial infarction patients during dialysis. Kaplan-Meier analysis.