To the Editor,
Over time, peritonitis has been the main complication of peritoneal dialysis. The episodes produced by coagulase-negative staphylococci have decreased since the start of the technique in relation to the improvements made in connection systems and the preoperative and postoperative catheter care.
Advances in connection systems over the last decades, as well as prophylaxis for S. aureus, have allowed an important reduction in the incidence of peritonitis caused by gram-positive bacteria. However, the incidence of gram-negative peritonitis has barely changed, which makes these proportionally more important. Meanwhile, gram-negative peritonitis is generally more severe and associated with a worse prognosis, including loss of catheter, failure in the technique and even death. Factors that can predict a poor response to treatment are: prior antibiotic treatment, use of just one antibiotic and use of an aminoglycoside versus a third or fourth generation cephalosporin. Beta-lactamase producing germs also have, in general, a poorer prognosis.1,2
It has been proven that local application of mupirocin in the exit site prevents infections caused by S. aureus, but does not reduce Pseudomonas aeruginosa infection nor infection with other gram-negative germs that, on the other hand, are associated with considerable morbidity and mortality. Several studies have reached the conclusion that local daily application of gentamicin on the exit site of the peritoneal catheter reduces infections of P.aeruginosa and other gram-negative bacteria in the catheter and reduces peritonitis by 35%, especially those caused by gram-negatives.3,4
An important increase in the percentage of gram-negative peritonitis was observed in our centre, reaching up to 40.62% in 2008; 38% of these cases presented the same bacteria in the peritoneal fluid and exit site. Given the progressive increase in this type of infections and the data that suggests that some episodes of gram-negative peritonitis could come from hidden peritoneal catheter infection, it was decided in January 2009 to change the healing protocol for exit sites, which was previously performed with saline solution, by applying topical gentamicin once a day.
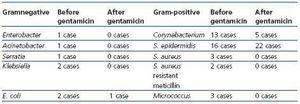
Before the change in protocol, pus or fluid was exuded from the catheter exit site in all the patients to evaluate its colonisation, without presenting any acute infection. After 4-5 months of healing with topical gentamicin, the exit site exudation was repeated, observing a decrease in the percentage of gram-negative germs, from 14% to 3% (table 1).
Of the 49 initial patients, 41 were monitored; the rest were excluded due to transfer to haemodialysis, transplant or death.
No differences were observed in the percentage of negative cultures after the initial treatment with gentamicin (5 pre-treatment and 6 post-treatment cases).
Of the 41 patients monitored, 9 cases presented exit site infection; the bacteria responsible were: E. coli in 2 cases and 7 cases of gram-positive bacteria. In our sample, no cases of yeast infection in the exit site were reported nor were there any other side effects to the use of topical gentamicin.
The percentage of peritonitis caused by gram-negative bacteria in our centre decreased from 40.65% in 2008 to 21.6% in 2009. Only one case in our sample presented the same bacteria in the exit site and in the peritoneal fluid, this patient was also careless in the healing process as well as in administering the topical antibiotic, admitting that they administered it irregularly.
In a high percentage of cases of peritonitis caused by gram-negative bacteria, the catheter had to be removed (above all if the bacteria produced beta-lactamases). In our centre, removal percentage was 80% in 2007. Return to peritoneal dialysis, in these cases, tends to be difficult, either because of the formation of multiple adherences or because of peritoneal membrane injury.5 The gentamicin probably does not influence the incidence of gram-negative peritonitis where the source of infection is intestine contamination, but it does affect the relationship with pericatheter contamination.
Furthermore, topical gentamicin is associated with few side effects. The most significant are Candida infections, that are generally resolved with an oral antifungal treatment with no major consequences.3
Table . Exit site colonisation