In recent years, the field of therapy in oncological has expanded significantly with the introduction of new immunomodulatory therapies that have resulted in an important change in patient survival; in addition there is an increase in the spectrum of adverse effects which are the consequence of its own mechanism of action.
We present the case of a 55-year-old woman with a history of active smoking who came to the emergency room for right frontoparietal headache, a non quantified weight loss and progressive focal neurological deterioration in the form of behavioral changes, paraphasia-dysphasias, gait instability and urinary incontinence. A cranial scan was performed, which revealed lesions suggestive of malignancy at the right temporal and left frontal levels with displacement of the midline and subfalcine herniation. These lesions, together with the presence of a pulmonary nodule in the left upper lobe seen in chest radiography, established a diagnosis of suspected intracranial metastasis due to a possible primary lung tumor. Several days later resection surgery of the right temporal lesion was performed. The histological study of the surgical specimen showed the presence of a pulmonary adenocarcinoma with non-mutated EGFR, and negative ALK and ROS1. The extension study was completed with a complete scan that confirmed the presence of a mass of 7cm in the posterior segment of the left upper pulmonary lobe that encompassed the left pulmonary artery and an ipsilateral mediastinal adenopathy of 12mm. Due to the fact that it was a stage IV pulmonary adenocarcinoma, a combined treatment with radiotherapy was decided on the left unresected left lesion and the administration of chemotherapy within an experimental protocol with nivolumab and ipilimumab achieving a maintained partial response according to morphological criteria by control image tests.
Six months after initiation of the immunomodulatory therapy, the patient developed nephrotic syndrome by biochemical data and no edema. The renal function remained normal. The oncology service decided to discontinue the drugs temporarily because of the possible causal relationship with the nephrotic syndrome. However, in view of the persistence of proteinuria, it was decided together with the nephrology service, to perform a renal biopsy to establish a histological diagnosis and the possibility of subsequent treatment.
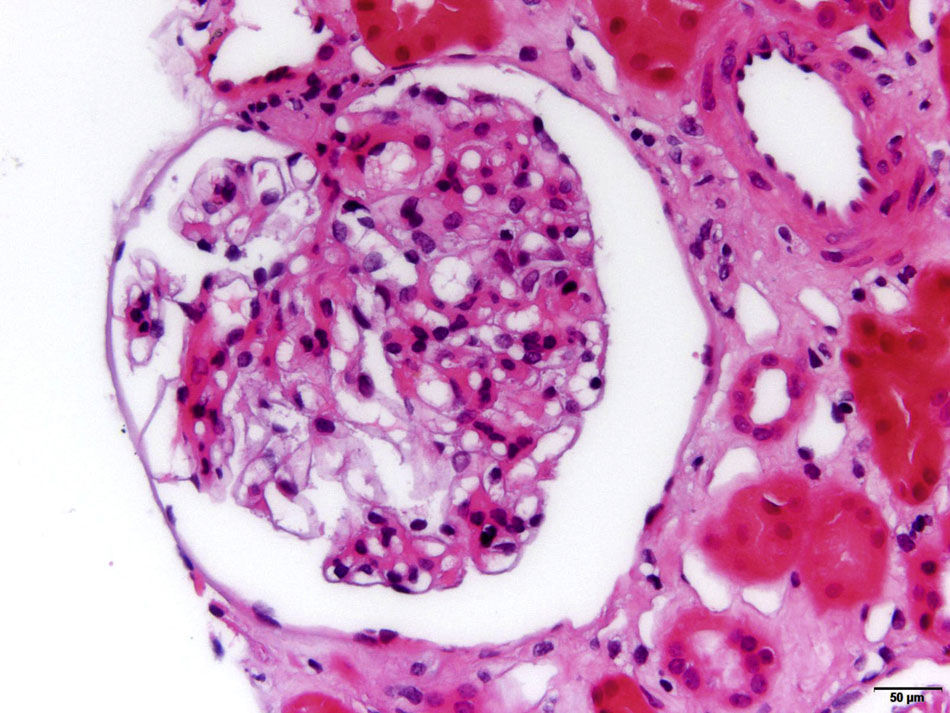
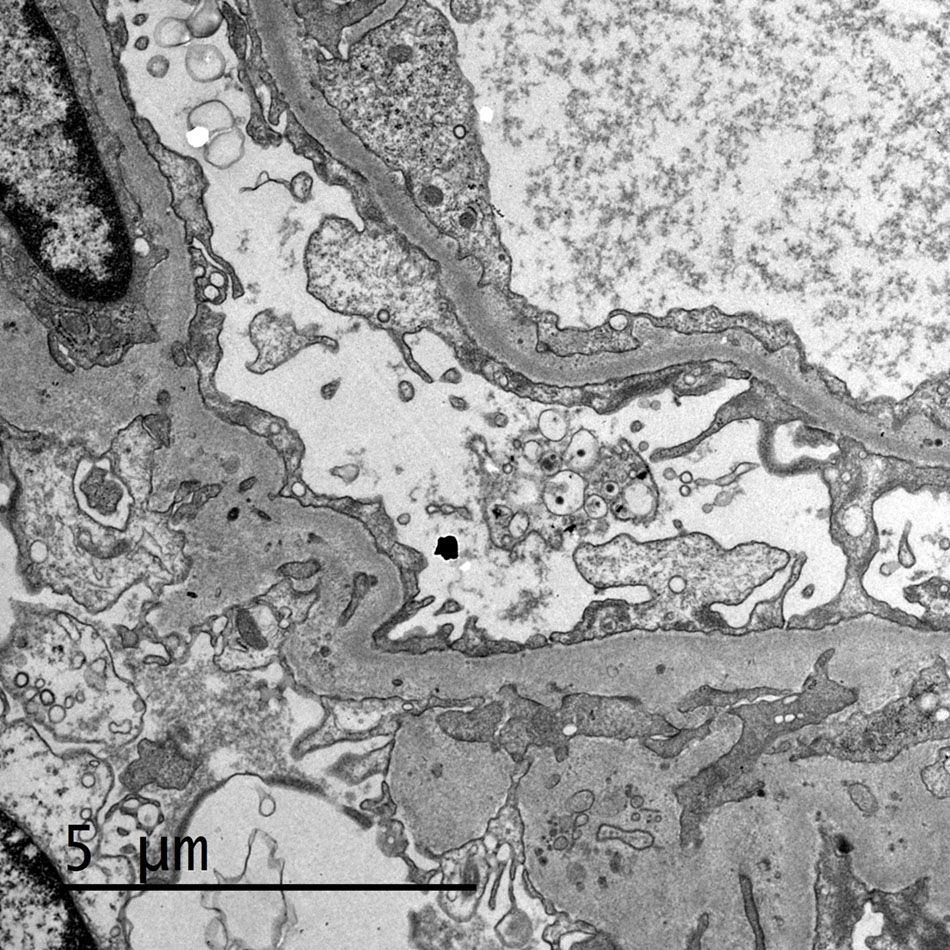
The renal biopsy showed the presence of a renal parenchyma with 8 glomeruli, one of which was sclerotic, with no relevant lesions in the remaining glomeruli(Fig. 1). The renal interstitium presented moderate fibrosis and areas of tubular atrophy with a discrete nonspecific inflammatory infiltrate. The arteries showed a 25% reduction of their inner diameter due to an atherosclerotic process, together with occasional hyalinosis in arterioles and without damage in the tubular capillaries. The immunohistochemical study did not demonstrate the presence of deposits, but the ultrastructural study (Fig. 2) identified a 60% fusion of foot processes of the capillary surface with rearrangement of the actin filaments. Combining the clinical and anatomopathological data, it was assumed the diagnosis of a disease due to minimal changes secondary to immunomodulatory treatment, so treatment with prednisone was started at a dose of 1mg/kg/day in a 10-mg regimen every 15 days, reaching a complete remission in the first 4 weeks of treatment.
The drugs inhibiting the “checkpoint”, such as nivolumab and ipilimumab, are monoclonal antibodies that act by inhibiting the receptors expressed on the surface of T lymphocytes (CTLA-4 and PD-1/PD-L1), responsible for inhibiting the stimulation that prevents the attack and the lysis of own cells. Overexpression of these receptors is frequent to evade immune control over tumor proliferation. By blocking these two receptors, there is an increase in the response of the immune system with loss of tolerance to tumor cells with a demonstrated beneficial effect against solid and hematological tumors.1 Previous studies have described the presence of acute renal failure (together with involvement of other organs, mainly glandular in the form of hypophysitis, adrenalitis and sialadenitis) with non-nephrotic proteinuria and predominantly interstitial damage in the renal histological study.2 However, glomerular involvement in this context is scarcely described in the literature. Some cases similar to our patient have been described, highlighting as common elements: the latency time from the beginning of the treatment, the excellent renal response to the administration of steroids and the suspension of the drug, the recurrence of the clinical picture after the reintroduction of the drug. treatment and extensive fusion of foot processes as a histological finding in the ultrastructural study.3–5 As already described in cases of idiopathic nephrotic syndrome,6 the proposed etiopathogenic mechanism of this entity is a direct damage of podocyte induced by self-reactive T lymphocytes through the expression and function of the podocyte CD80 (B7-1) receptor. The increase in the use of these therapies in oncology, should increase the incidence of cases similar the one presented here. Finally, we believe that it is necessary to monitor renal function and proteinuria in this group of patients in order to make an early diagnosis and establish an effective treatment.
Please cite this article as: Redondo B, Moliz C, Alonso M, Paz-Ares L, Praga M, Morales E. Inmunoterapia en el cáncer: grandes expectativas en el mundo de la oncología, pero un motivo de preocupación renal. Nefrologia. 2019;39:94–96.