Potentially inadequate prescription (PIP) are prescription with a risk of adverse effects that are superior to the clinical benefit. PIP is also considered if doses or duration of treatment are more that optimal, with potential interactions with other medications and with the patient's diseases, also includes therapeutic duplicities. In addition, it is inadequate the omission of medications with established indication in a specific patient.
One of the most used tools in Europe for the detection of PIP is the criteria of Screening Tool of Older Person's inappropriate Prescription (STOPP)/Screening Trial to Alert Doctor to Right Treatment (START) proposed by Gallagher et al. in 20081 and accepted by the Spanish Society of Geriatric.2 They have been recently updated with incorporating new data, or the arrival of new drugs and identification of drugs considered potentially inadequate.3,4
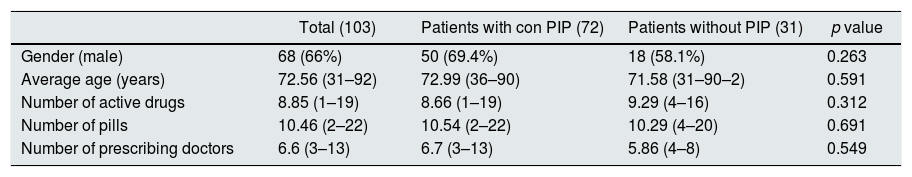
There is little information about PIP in patients with chronic renal failure.5–7 Therefore, we decided to perform a study aiming to detect systematically the PIP, according to the STOPP/START criteria, in the 103 dialysis patients followed in our hospital. For this, the pharmacotherapeutic records of all these patients were reviewed, considering the following variables shown in Table 1: age, sex, number of active ingredients, number of pills, number of prescribing doctors and STOPP/START criteria identified.
Characteristics of the studied population (n=103).
| Total (103) | Patients with con PIP (72) | Patients without PIP (31) | p value | |
|---|---|---|---|---|
| Gender (male) | 68 (66%) | 50 (69.4%) | 18 (58.1%) | 0.263 |
| Average age (years) | 72.56 (31–92) | 72.99 (36–90) | 71.58 (31–90–2) | 0.591 |
| Number of active drugs | 8.85 (1–19) | 8.66 (1–19) | 9.29 (4–16) | 0.312 |
| Number of pills | 10.46 (2–22) | 10.54 (2–22) | 10.29 (4–20) | 0.691 |
| Number of prescribing doctors | 6.6 (3–13) | 6.7 (3–13) | 5.86 (4–8) | 0.549 |
PIP: potentially inadequate prescription.
It was found that 69.9% (n=72) of the patients had at least one potentially inappropriate prescription and a total of 231 inappropriate prescriptions were detected (132 START and 99 STOPP).
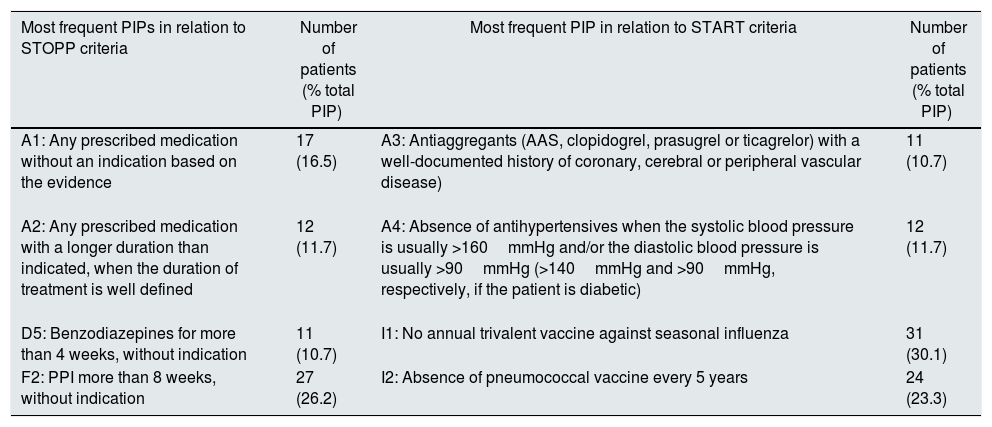
According to the STOPP criteria (tool for the detection of potentially inappropriate prescriptions) the most frequent causes of PIP were (see Table 2): A1 (any prescribed medication without an indication based on evidence); A2 (any prescribed medication with a longer duration than indicated, when the duration of treatment is well defined); D5 (benzodiazepines for more than 4 weeks, without indication); F2 (proton pump inhibitor for more than 8 weeks, without indication). For the START criteria (instrument to call the doctor's attention about treatments that were indicated and appropriate): A3 (absence of antiplatelet agents such as ASA, clopidogrel, prasugrel or ticagrelor in patients with a well-documented history of coronary, cerebral or peripheral vascular disease); A4 (absence of antihypertensive medication if the systolic blood pressure is usually >160mmHg and/or the diastolic blood pressure is usually >90mmHg, and in the case of diabetes mellitus >140mmHg and >90mmHg, respectively); I1 (annual trivalent vaccine against seasonal influenza), and I2 (absence of pneumococcal vaccine every 5 years).
The most common PIP errors according to the STOPP/START criteria.
| Most frequent PIPs in relation to STOPP criteria | Number of patients (% total PIP) | Most frequent PIP in relation to START criteria | Number of patients (% total PIP) |
|---|---|---|---|
| A1: Any prescribed medication without an indication based on the evidence | 17 (16.5) | A3: Antiaggregants (AAS, clopidogrel, prasugrel or ticagrelor) with a well-documented history of coronary, cerebral or peripheral vascular disease) | 11 (10.7) |
| A2: Any prescribed medication with a longer duration than indicated, when the duration of treatment is well defined | 12 (11.7) | A4: Absence of antihypertensives when the systolic blood pressure is usually >160mmHg and/or the diastolic blood pressure is usually >90mmHg (>140mmHg and >90mmHg, respectively, if the patient is diabetic) | 12 (11.7) |
| D5: Benzodiazepines for more than 4 weeks, without indication | 11 (10.7) | I1: No annual trivalent vaccine against seasonal influenza | 31 (30.1) |
| F2: PPI more than 8 weeks, without indication | 27 (26.2) | I2: Absence of pneumococcal vaccine every 5 years | 24 (23.3) |
PPI: inhibitor of proton pump; PIP: potentially inadequate prescription.
Inadequacy was associated with the number of pills (p<0.031) only for STOPP criteria. It was not related to age, gender or number of prescribing doctors in any of the cases. These results are similar to those obtained in other studies in different populations.5–8
The STOPP/START7 criteria have proven to be a good tool for detecting potentially inadequate prescriptions and improve the quality of treatments in all healthcare settings (including dialysis patients that in general are elderly, multi-pathological and polymedicated), also provides a common language that allows the comparison and the adoption of educational and corrective measures.
The greatest limitation is that these criteria are under the constant evolution of knowledge and exposed to a periodic update.7 It would be desirable to establish specific STOPP/START criteria for patients with chronic kidney disease and/or dialysis.
Please cite this article as: Gonzalez-Lopez A, Nava-Rebollo A, Chocarro-Martinez A, Andres-Martin B, Santana-Zapatero H, Herrera-Gomez F, et al. Prescripción potencialmente inapropiada en pacientes en diálisis utilizando los criterios STOPP-START. Nefrologia. 2019;39:92–94.