This case is a 44-year-old woman without previous medical history, who presented with fever of 38.7°C of 2 weeks of evolution mainly in the afternoon, without evidence of source of infection, without chills or shaking. She was treated as a flu-like syndrome with NSAIDs and antipyretics. Subsequently, she developed a non-pruriginous generalized cutaneous exanthema, went to the emergency room and the blood tests revealed anemia (11.7μg/dlhb) mild leukopenia with moderate lymphopenia (3640μleuk/μl, 18% lymph), CRP 22 units and a moderate increase high serum transaminase levels. Renal function was normal (serum creatinine 0.73mg/dl), physical exam anodyne except for a temperature of 37.7°C and confluent exanthema including palms/plants that disappear with pressure. Normal chest X-ray. With the diagnosis of exanthematic febrile syndrome with hepatic and hematological alteration, she was admitted for study, and doxycycline was prescribed.
On subsequent days hepatosplenomegaly and pericardial effusion were detected, sedimentation rate was 110 and smears without cell atypias but a 11% of LUC cells were detected. Iron, folic acid, B12, IgA, IgG, C3-4, ANCA, ASLO, normal citrullic peptide. Proteinogram: polyclonal elevation of the gamma globiulins, elevated IgM, FR 300IU/ml cryoglobulins were negative. ANA: 1/80, DNA, negative, ENA negative except 24UI/ml U1-RNP. Serology: negative for HBV, HCV, HIV, Legionella, CMV, parvovirus B19, Leptospira, C. burneti, R. coronii, pneumococcus, negative blood cultures; EBV equivocal IgG/positive IgG.
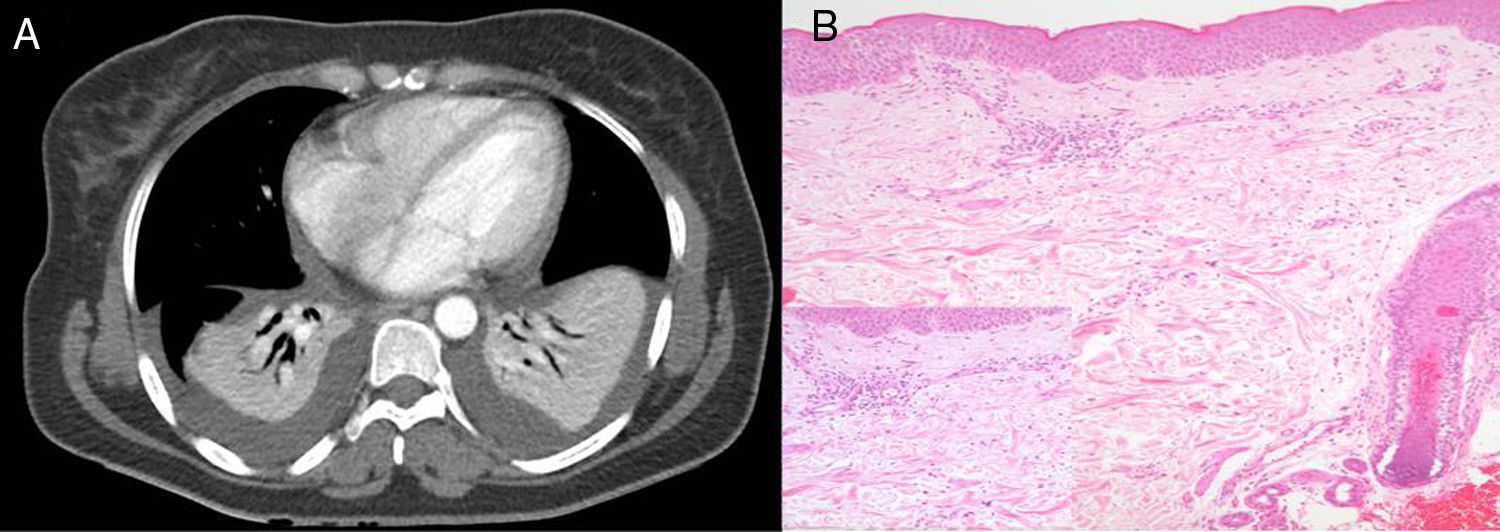
He remained febrile, the fifth day of admission the fever increased with chills/shivering and respiratory insufficiency; the patient had atelectasis/bibasal condensation with symmetrical pleural effusion (Fig. 1A) and procalcitonin 4.39μg/ml, and received broad spectrum antibiotic therapy.
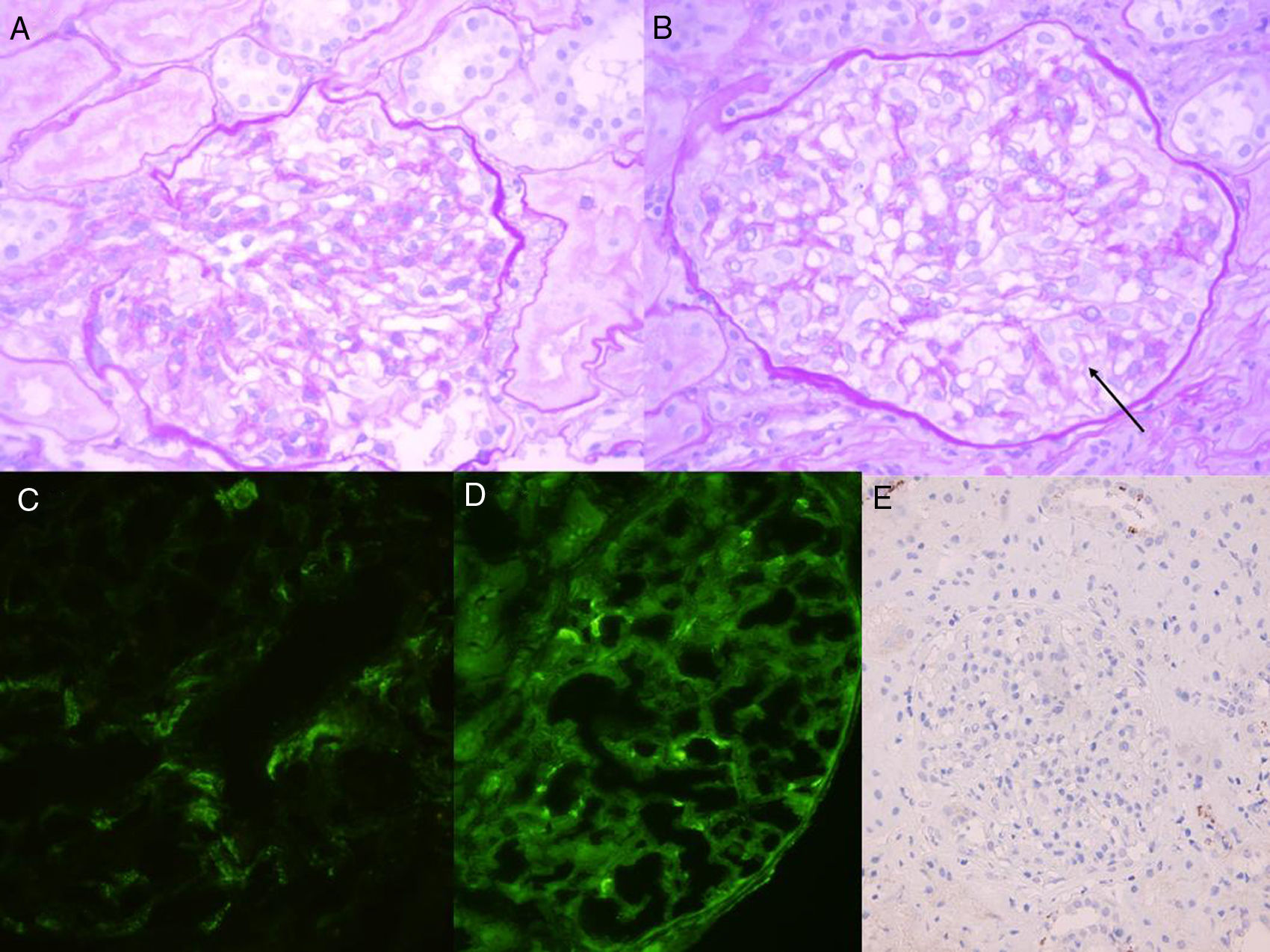
CT scan (A): atelectasis/bibasal condensation with symmetrical effusion, pericardial effusion. Skin biopsy (B): focal intracellular epidermal spongiosis, mild edema and hepatic extravasation; and; dermal vessels occupied by inflammatory cells (increase: lymphocytes and polymorphonuclear cells with eosinophilic isolates).
Urine showed a proteinuria 1.8g/day, sediment 40H/C (28% dysmorphia), the serum cholesterol was normal, albumin 2.2g/L; Minimal symmetrical pretibial edema, normal blood pressure and normal values of serum creatinine, as well as kidney morphology by ultrasound. He had no signs of systemic disease. Dermal biopsy confirms urticarial process (Fig. 1B). A renal biopsy reported a mesangial proliferative glomerulonephritis with immune deposits mainly IgM/C1q. PCR for EBV in blood was +, but in situ hybridization in the kidney being negative (Fig. 2). It is diagnosed of infectious mononucleosis (MI) with hematological, pleuropericardic, hepatic and renal involvement with mesangial proliferative glomerulonephritis by immunocomplexes. It evolves favorably, remaining asymptomatic and the PCR for EBV became negative. At the end of the year, remission persists, although anti-U1-RNP+ persists as well as generalized arthralgias treated with usual analgesia that had been present for years. He has not evidence of other autoantibody nor presented any other symptoms of systemic disease.
In adults the infectious mononucleosis (IM) is presented with atypical symptoms,1 with absence of pharyngotonsillitis, lymphadenopathy and lymphocytosis/lymphocytic atypia. Pleural or pericardial effusions are exceptional that have been described in only isolated cases.2 All this, together with the leucopenia-anemia, serositis and U1-RNP positivity, made us think of the coexistence of infection and autoimmunity.
The prevalence of renal involvement of IM is not well known, it usually goes unnoticed with urinary abnormalities that are asymptomatic (14–17%).3 The published cases are isolated and are mainly tubulointerstitial involvement. There are few cases of various types glomerulopathies, mediated or not by immunocomplexes, which may occur alone or coexisting with interstitial involvement.4 The presence of renal failure is estimated to be between 1.6 and 4.8%.3 As for its pathogenesis, several non-exclusive mechanisms have been considered: immune complexes mediated damage or direct toxic-cytopathic damage, the latter being found in interstitial lesions, in which the virus has been isolated and found to be mainly in CD8+ cells. In our case we were unable to find the virus by in situ hybridization and tubulointerstitial damage was minor, so we deduced that the damage was mediated by antibodies/immunocomplexes rather than by direct cytotoxicity. The deposits were mostly IgM/C1q. Andres et al.5 describe a similar case with IgM/C3 mesangial deposits, this being the same heterologous serum IgM against Paul Bunnell antigen. This is because the humoral immune response to EBV is primarily at the expense of IgM.6 Also, activation of the 2 complement pathways has been described in MI.7
Hyperstimulation of host immunity by EBV in some cases is unknown, but in vitro and in vivo the natural IgM produced by the polyclonal activation of B lymphocytes during MI has antihistone activity.8 Niller et al.9 related different EBV antigens with the activation of autoreactive B lymphocytes in multiple sclerosis, SLE and RA. In this respect, the positivity for U1-RNP is attributed to the virus induced activation of specific immunoglobulin secreting B lymphocytes against that protein, by cross-reactivity with antigens of the EBV itself.10 It is not know why, despite presenting this antibody, it does not develop symptoms although the title presented has never been very high. The patient's HLA was performed and predisposing alleles for autoimmune diseases have not been found.
Regarding treatment, the glomerulopathy resolved in parallel to the mononucleosis. In the literature, some cases received corticosteroids, especially those with tubulointerstitial involvement. That was not our case that only had slight renal clinical and histological involvement (although the mesangial hypercellularity was diffuse in some glomeruli, it was segmental in others and, but in general it was mild). Acyclovir was not given since bibliography reports low efficacy.
We conclude that the frequent atypical presentation of IM in the adult can lead to delay in the diagnosis. The renal involvement is usually tubulointerstitial by cytotoxicity in which the virus can be found, and virus is less frequently observed in glomeruli. Should take into account the pathogenesis by immunocomplexes and complement activation. EBV is considered a “trigger” of self-reactive phenomena that can persist over the time and it may cause an autoimmune disease in cases with a predisposing environment.
Please cite this article as: Martín-Gómez MA, Caba Molina M, Cruz Caparros G, Guerrero Sánchez E, Caballero González A, Gómez Morales M. Glomerulonefritis aguda por inmunocomplejos en mononucleosis infecciosa. Nefrología. 2017;37:439–441.