To the Editor:
Pseudohypoparathyroidism1 (PHP) is a heterogeneous condition characterised by hypocalcaemia and secondary hyperparathyroidism, whose aetiology lies in the resistance to the biological action of circulating parathyroid hormone (PTH). It is generally diagnosed during childhood. When the diagnosis is made in adulthood, it may be difficult to distinguish it from secondary hyperparathyroidism,2 especially in patients with renal failure.
CASE STUDY
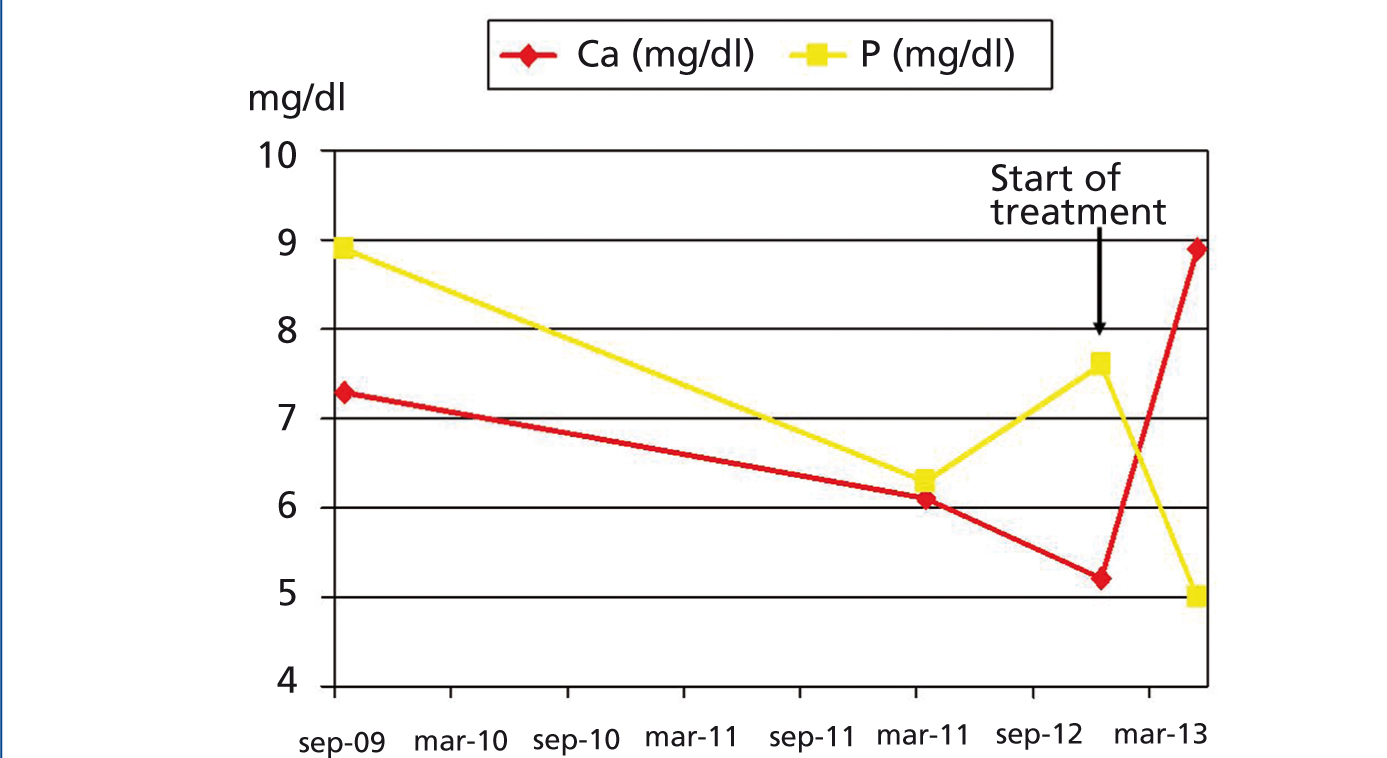
We report the case of an 18-year-old male with a history of functionally bicuspid aortic valve, who came to the Emergency Department due to colicky hypogastric pain lasting 72 hours, which did not subside when treated with non-steroidal anti-inflammatory drugs (NSAIDs) every 8 hours. The patient had previously experienced similar episodes. On admission, he had blood pressure of 120/80mmHg and I/IV early diastolic murmur, with the rest of the examination being normal. The laboratory test displayed urea 71mg/dl, creatinine 3.69mg/dl, Mg 2.1mg/dl, Ca 5.2mg/dl, P 7.6mg/dl, total protein 6.27g/dl, albumin 3.6g/dl, intact PTH 216pg/ml, 25-hydroxyvitamin D 7.3ng/ml, normal thyroid hormones, venous blood gases: pH 7.37, pO2 50mmHg, pCO2 37mmHg, bicarbonate 21mmol/l, renal function in urine: EF Na 0.71%, glucose 9mg/dl, urea 946mg/dl, Cr 86.37mg/dl, Na 27mmol/l, K 21.2mmol/l, Ca 7.8mg/day and P 850.2mg/day; systematic and normal urinary sediment, with negative haematuria and proteinuria; blood count: haemoglobin 15.1g/dl, leukocytes 11,000/ul, platelets 167,000/ul. Laboratory tests were reviewed and they revealed previous hypocalcaemia and hyperphosphataemia, with normal renal function, which had not been detected for at least three years (Figure 1). The biochemical study of his parents’ calcaemia, phosphataemia and PTH were normal. The patient’s clinical progression was good after we withdrew the NSAIDs, to which the aetiology of acute renal failure was attributed, oral and intravenous hydration, oral calcium and vitamin D, with kidney function being normal on discharge. Abdominal symptoms subsided after hypocalcaemia was corrected, without recurrences of similar episodes.
DISCUSSION
The term PHP encompasses a heterogeneous group of uncommon metabolic disorders whose common denominator is variable resistance to PTH action.1-3 Two types of PHP can be distinguished in accordance with the response of urinary cAMP after the intravenous injection of PTH: type I PHP, in which cAMP does not increase following the administration of PTH, and type II PHP, in which cAMP increases.4 Type I PHP is divided into three subtypes: Ia, Ib and Ic. Patients with subtypes Ia and Ic have an autosomal dominant inheritance pattern and generally present the Albright osteodystrophy phenotype4 (short height, obesity, learning difficulties, subcutaneous calcifications and typical skeletal defects) and multi-hormone resistance. Subtype Ib is characterised by isolated resistance to PTH, it may have a normal phenotype or the Albright osteodystrophy phenotype and the defect is usually sporadic, but it is occasionally has autosomal dominant inheritance. In type II PHP, no molecular defect has been identified, but it lacks the Albright phenotype and multi-hormone resistance and it is not usually familial.5
We performed a differential diagnosis between chronic kidney disease, vitamin D deficiency and PHP. The reversibility of renal failure and persistent hypocalcaemia, hyperphosphataemia and elevated PTH ruled out chronic kidney disease as aetiology, and the absence of hypophosphataemia ruled out vitamin D deficiency. We concluded that this patient had type Ib or II PHP, given the absence of the AHO phenotype and multi-hormone resistance. However, we cannot determine clearly whether our patient corresponded to type Ib or type II PHP.
In summary, we reported the case of a patient with renal failure, hypocalcaemia, hyperphosphataemia and elevated PTH of long progression. The nephrologists’ knowledge of the calcium-phosphorus metabolism pathophysiology allowed us to make an early diagnosis and carry out early treatment of an uncommon condition for nephrologists and, as its late diagnosis reveals, one that is also uncommon for the other medical specialties. It is necessary to emphasise the importance of early PHP treatment in order to normalise serum calcium and prevent the bone loss that can occur in the long term if a chronically high level of PTH is maintained. The objective of treatment was to normalise serum calcium levels and curb PTH hypersecretion, and as such, vitamin D derivatives and calcium supplements were used.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Figure 1. Progression of calcium and phosphorus (mg/dl) prior to diagnosis and from the start of treatment.