Antecedentes: La presión arterial se asocia negativamente con la percepción del dolor. Objetivos: En este estudio se comparan el dolor y las relaciones entre presión arterial y umbral doloroso al inicio y final de la hemodiálisis. Métodos: 14 pacientes con trastorno renal crónico bajo diálisis participaron en el estudio. Los umbrales de dolor fueron evaluados mediante algometría de presión de forma bilateral en dos puntos «gatillo»: la segunda costilla y la rodilla. La presión arterial y los umbrales de dolor se evaluaron: 1) 15 minutos después del inicio de la diálisis, y 2) 30 minutos antes de su final. Resultados: La presión arterial no cambió significativamente durante la diálisis. Se observó una disminución significativa del umbral de dolor en la segunda costilla izquierda y en la rodilla izquierda y derecha desde el inicio al final de la hemodiálisis. Al inicio de la diálisis no se obtuvieron correlaciones significativas entre presión arterial y dolor, mientras que al final de la diálisis la presión arterial se correlacionó positivamente con los umbrales de dolor (rs entre 0,552 y 0,806). Conclusiones: La hemodiálisis se asocia a cambios en la
sensibilidad al dolor y en las relaciones entre presión arterial y dolor, y sugiere una modificación en el mecanismo de inhibición aferente del dolor originado a nivel cardiovascular. Como posibles explicaciones de este efecto se discuten los cambios que produce la hemodiálisis en las funciones cognitivo-perceptivas, en la regulación autonómica cardiovascular y en la habituación de variables relacionadas con el estrés.
Antecedents: Arterial pressure is negatively associated to pain perception. Objectives: In this study, pain and the relations between arterial pressure and pain threshold were compared at the beginning and end of the heamodialysis. Methods: 14 patients with chronic renal disease participated in the study. Pain thresholds were evaluated with pressure algometry bilaterally at two tender points: the second rib and the knee. Arterial pressure and pain thresholds were assessed twice: 1) 15 min alter dialysis onset and 2) 30 min before dialysis ended. Results: Arterial pressure remains unchanged through the dialysis. The course of dialysis was associated to a decrease in pain threshold in the second left rib and left and right knees. At the beginning of dialysis arterial pressure were uncorrelated with pain, while at the end of the dialysis both systolic and diastolic arterial pressure were strongly associated to pain thresholds (rs between 0.552 and 0.806): increased arterial pressure was associated to lower pain in terms of increased threshold. Conclusions: Heamodialysis is associated to changes in pain sensitivity and in the relationships between arterial pressure and pain, suggesting a modification in the ascending pain inhibition system arising from the cardiovascular system. Possible explanations of this effect include the changes produced by heamodialysis in cognitive-perceptive functions, in autonomic cardiovascular regulation, and in the habituation of stress-related variables.
INTRODUCTION
The cardiovascular system modulates the central processing of pain, especially through changes in blood pressure (BP), constituting an important source of anti-nociception.1 The subjective experience of pain is inversely correlated with BP levels,1-3 such that patients with arterial hypertension perceive less pain and have lower sensitivity than normotensive subjects, a phenomenon known as hypertension-induced hypoalgesia.4 The perception of pain is also reduced in healthy people with moderately high BP values.1,2 On the contrary, people with chronic arterial hypotension have higher sensitivity and an increased perception of pain as compared to normotensive subjects.5,6 In this manner, courses of action that increase BP lead to reduced response to pain.3
Epidemiologically, some studies have shown that high BP levels protect the body against chronic pain, such as headaches7 and musculoskeletal pain.8 In the clinical setting, chest pain experienced during physical exercise is inversely correlated with BP,9 as occurs in post-operative pain.10 The baroreflex is the primary mechanism used for the short-term regulation of BP and acts as an important source of autonomic cardiovascular regulation. The central inhibitory effect that it causes is one of the fundamental mediating main mechanisms involved in explaining the pain-reducing effect of increased BP.1,4,11,12
Haemodialysis can present a favourable context for the analysis of the relationship between BP and pain. Firstly, reduced body liquid volume that is produced during haemodialysis could be associated with reduced BP, which would allow for a more direct evaluation of the relationship between BP and pain. Secondly, chronic kidney disease is associated with autonomic cardiovascular changes, which are in turn modified by the process of haemodialysis.13-15 These autonomic changes could affect the afferent pain inhibition originating in the cardiovascular system. Also, several studies have shown that haemodialysis produces acute improvements in the cognitive deficits present in chronic kidney disease, which could optimise the psychophysiological processes involved in the perception of pain and the relationships between pain and BP.16,17 Finally, given the long duration of the procedure (more than 4 hours), haemodialysis provides a large database that can facilitate habituation to the psychological stress-related variables (for example, social interactions or previous activity), reducing the effects that interfere with the relationship between BP and pain. The importance of obtaining reliable measurements of at-rest cardiovascular activity has been emphasised for a very long time in psychophysiological literature.18 These studies suggest the importance of using appropriate baseline periods before registering physiological parameters, and it is recommended that they be long enough (no less than 15min).18 The haemodialysis procedure widely complies with this requirement.
In this context, the objectives of our study were: 1) to analyse the relationship between BP and pain at the start and end of haemodialysis, and 2) to analyse the changes in BP and pain during haemodialysis from start to end. We used pressure algometry to generate pain so as to establish pain thresholds. Our hypotheses were: 1) that we would observe a positive relationship between BP and pain threshold, and that this association would be greater at the end of dialysis than at the start, and 2) that BP and pain thresholds would be reduced at the end of dialysis as compared to the start.
METHOD
Patients with chronic kidney disease undergoing haemodialysis treatment (online) were selected from the Santa Catalina dialysis centre (Jaen). The inclusion criteria were: age <56 years (in order to ensure optimal understanding of the instructions and a good general state of health) and signed informed consent. The exclusion criteria were: suffering from any type of chronic pain disorder, or the use of analgesic, antidepressive, or anxiolytic agents. All patients that complied with these criteria participated in the study. In this manner, the sample was made of 14 patients (nine men and five women) with ages ranging from 23 years to 55 years (mean: 43, standard deviation [SD]: 9.9) and a mean time on dialysis of 6.28 years. We performed two separate measurements while the patient was comfortably reclined in the dialysis chair, once at the start and another at the end of the 4-hour haemodialysis session. Fifteen minutes after the start of dialysis, we took three oscillometric BP measurements (Omron M4, Hamburg, Germany). Thirty minutes before the dialysis session ended, we took another three BP measurements. The BP readings were taken with a 5-minute interval between each. We obtained mean systolic and diastolic BP for the first (start) and second (end) measurements. After taking the BP measurements, we evaluated pain thresholds. To this end we used a patented digital algometer (dolorimeter) (http://www.recolecta.net/buscador/single_page.jsp?id=oai:digibug.ugr.es:10481/1123) with a ±1 gram precision and output values in g/cm2. This dolorimeter is composed of two units connected to a cable. In the stimulation unit, a wooden bar is inserted with a circular surface area of 1cm2 and a height of 10cm. The central unit includes a digital screen that reads out the pressure values and provides a button for interrupting the test and saving the value corresponding to that moment in time. We took individual measurements bilaterally in two tender or trigger points19: 1) the second rib (in the osteochondral junction, below the clavicle), and 2) the knee (in the medial fat pad proximal to the joint line), with the first measurements taken from the left side in each case. Pressure increased at approximately 1kg/s. Patients had to press the button on the dolorimeter at the moment that the pressure started to be painful (pain threshold). In order to avoid the influence of possible sensitisation processes, in the second pain measurement points 1.5cm away from the initial spot were stimulated. Based on these characteristics, our study can be defined as a quasi-experimental study with a pre-post design.
The pain threshold values had an asymmetrical distribution, and so we performed a logarithmic transformation so they would comply with the criteria of normality. We compared the measurements taken for each measurement (start vs end) using Student’s t-tests for related samples. We analysed the relationship between BP and pain threshold using Pearson’s correlation. We set the level of statistical significance at P<.05.
RESULTS
Effects of haemodialysis on blood pressure and pain
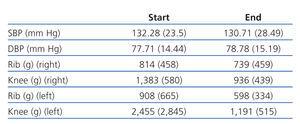
BP and pain threshold values at the start and end of dialysis are presented in Table 1. BP, both systolic and diastolic, did not vary significantly during dialysis (P>.7). However, the progression of the dialysis session was related to a decrease in pain thresholds in the second left rib (t[14]=2.17; P=.049) and left (t[14]=3.71; P=.003) and right (t[14]=3.68; P=.003) knee. The decrease in pain thresholds for the second right rib was not significant (t[14]=1.40; P<.185).
Relationship between blood pressure and pain
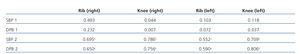
The correlations obtained between BP and pain thresholds are presented in Table 2. At the start of dialysis, we did not obtain any significant correlations (P>.7). At the end of dialysis, both systolic and diastolic blood pressure had strong correlations with pain thresholds, such that higher BP levels were associated with higher pain thresholds. In order to show this effect, we have presented a scatter plot and regression line, showing how diastolic BP is associated with pain thresholds for the left knee (Figure). Here we can observe how increases in diastolic BP are linearly correlated with higher pain thresholds (that is to say, reduced sensitivity to pain).
DISCUSSION
The results from our study show important positive relationships between BP and pain thresholds at the end of dialysis, but not at the start. Also, despite the fact that BP did not change between the two measurements performed, pain thresholds were lower in the second one as compared to the first, which would suggest increased sensitivity to pain at the end of dialysis. Our hypothesis was that BP would decrease during the course of dialysis. This hypothesis was not fulfilled, since BP values did not change between the two measurements. Whereas intra-dialysis episodes of acute hypotension are somewhat frequent, there is no agreement in the medical literature regarding the changes produced during haemodialysis in tonic BP values. In some studies, dialysis has been associated with reductions in BP,13 whereas in other studies, this effect has not been observed.14 This discrepancy is probably due to possible differences in the cardiovascular state of these patients. If an individual has optimal cardiovascular functioning, homeostatic mechanisms can be put into place (changes in vascular tone, heart rate, ventricular function, baroreceptor function, etc.).that compensate the reduced volume of body liquids. In this sense, our sample was made up of patients with renal problems of a relatively young age as compared to other studies, and our results suggest that the self-regulating mechanisms for controlling BP in these patients were conserved and could successfully compensate for the changes in liquid volumes, maintaining the integrity of BP regulation.
Although BP did not change between our two measurements, we did observe increased sensitivity to pain at the end of the dialysis session as compared to the beginning. Pain thresholds, especially for the left side, were higher at the second measurement. In the absence of changes in BP, the possible explanations for this effect are inherently speculative. In our opinion, it may be due to one of three different mechanisms.
Firstly, chronic kidney disease is associated with peripheral neuropathy and several different autonomic deficits.13-15 Due to the autonomic origin of the afferent pain inhibition system mediated by changes in BP, disorders in this system may be affecting these patients. It is known that haemodialysis improves some of the these autonomic alterations,13-15 and so one could assume a better functioning of this anti-nociceptive system at the end of haemodialysis as compared to the start. Secondly, we do know that several different neuropsychological deficits arise in patients with chronic kidney disease, and that the process of blood purifying during dialysis is associated with a normalisation of neuronal activity and improved cognitive ability in several different neuropsychological functions.16,17 In this sense, normalised blood composition and liquid volume could also favour improved functioning of the perceptive and psychophysiological processes involved in the afferent inhibition of pain mediated by the baroreflex. Finally, another explanation could be found in the factors associated with the stress-induced analgesia phenomenon.20 The dialysis procedure starts in a relatively stressful environment (nurses, machines, tubes, smells, needles, disrobing, white coat phenomenon, etc.) Among the most stressful elements of the procedure is the connection of needles to the arteriovenous fistula. In addition to the pain produced by the piercing of the needles, the patient tends to be worried about possible problems with the fistula. Additionally, the appearance of intra-dialysis pain can also have an influence, and this is relatively common.21,22 The most common causes of this phenomenon are derived from the dialysis procedure itself (fistulas can produce ischaemic and neurological pain, complications associated with catheters that result in pain, etc.) and ischaemic and musculoskeletal pain.21,22 These pains, especially those associated with the dialysis procedure, tend to be less severe at the end of the procedure. Given the long duration of dialysis sessions, one might expect a progressive habituation or reduction in stress-related factors, activation, and pain (at least in patients that are used to the procedure, such as those that have participated in this study), moreover, these adverse conditions are less severe at the end of the dialysis session than at the beginning. The stress-induced analgesia effect is mediated by several different mechanisms, such as endogenous opiates, cannabinoids, monoamines, gamma-aminobutyric acid, glutamate, CRF, cortisol, etc.20
The associations observed here between BP and pain are very interesting and perhaps the strongest described in the literature. For example, and so as to compare our results to those in other studies, Myers et al23 used the cold pressor test and found correlations between systolic BP and pain thresholds of 0.22 and pain tolerance of 0.31; Fillingham, et al24 used thermal and ischaemic pain and observed correlations between 0.02 and 0.35 in women and 0.13 and 0.50 in men for pain thresholds and tolerance, whereas the correlations with the subjective perception of thermal pain were -0.37 in women and -0.44 in men; McCubbin and Bruelhl25 found a correlation of -0.54 between systolic BP and the intensity of pain perceived during the cold pressor test; Duschek, et al6 used thermal pain and found correlations between systolic BP and pain thresholds, tolerance, and subjective perception of the intensity and discomfort of pain of 0.30, 0.42, -0.32, -0.35, respectively; using the cold pressor test, Duschek, et al5 found correlations between systolic BP and pain threshold, tolerance, and subjective intensity of 0.26, 0.26, and -0.32, respectively, etc.
One limitation to our study was the small sample size used, since we included patients from only one single haemodialysis centre. This suggests the need to replicate the results obtained in our study with a larger sample size of patients. In conclusion, haemodialysis is associated with changes in sensitivity to pain and the relationships between BP and pain, which points towards a modification to the mechanism of afferent pain inhibition originating in the cardiovascular system. The possible origin of these changes is not clear, and future research will be needed to elucidate the changes produced by haemodialysis in cognitive-perceptive functions and cardiovascular autonomic regulation (especially the baroreflex).
ACKNOWLEDGEMENTS
We would like to thank the Asociación de Enfermos Renales de Jaén (association of renal patients of Jaen) for their collaboration with this study. This research was funded by a project of the Spanish Ministry of Science and Innovation (PSI2009-09812).
Table 1. Mean ± standard deviation of systolic BP (SBP), diastolic BP (DBP), and pain thresholds at the start and end of haemodialysis
Table 2. Pearson¿s correlation between systolic BP (SBP) and diastolic BP (DBP) and pain thresholds at the start (1) and end (2) of haemodialysis
Figure 1. Scatter plot and regression line for diastolic BP (DBP) and pain thresholds in the left knee