La mitad de los enfermos que comienzan tratamiento con hemodiálisis periódica lo hacen con un catéter venoso como acceso vascular (inicio no programado). Un objetivo del Grupo de Gestión de Calidad de la Sociedad Española de Nefrología es conseguir que el 80% de los enfermos comiencen la hemodiálisis a través de una fístula arteriovenosa. Hemos querido revisar las causas que condicionan en la actualidad el inicio no programado, para analizar cuáles pueden ser corregibles. En el año 2010, 43 enfermos comenzaron tratamiento con hemodiálisis periódica en el Hospital Ramón y Cajal de Madrid. La edad media fue de 61 años, el 79% eran hombres, la etiología más frecuente fue la diabetes mellitus (23%) y el índice de Charlson era de 6,3 ± 2,6. El inicio no programado de la hemodiálisis ocurrió en 20 enfermos (47%), sin objetivarse diferencias con los 23 enfermos que comenzaron hemodiálisis de forma programada, en ninguno de los diferentes parámetros clínicos o sociodemográficos analizados. La causa más frecuente de inicio no programado fue la reagudización de una enfermedad renal crónica en estadio 3 o 4, previamente estable, por un proceso intercurrente imprevisible (ocho enfermos, 40% de los casos). Un enfermo comenzó hemodiálisis periódica por un fracaso renal agudo no recuperado y en otros seis el motivo de inicio no programado no fue achacable al funcionamiento del sistema sanitario (enfermedad renal crónica no conocida en tres casos y causas achacables al propio enfermo en otros tres). Solamente en el 25% de todos los casos (cinco enfermos), la causa de inicio no programado pudo ser corregible. La mayoría de las causas de inicio no programado de hemodiálisis son ajenas a la organización sanitaria y, por tanto, difíciles de subsanar. Estas circunstancias deben tenerse en cuenta cuando se revisen los objetivos del Grupo de Gestión de Calidad.
Half of patients starting chronic hemodialysis used a transient vascular catheter as a vascular access (unplanned initiation). An objective of the Quality Management Group of the Spanish Society of Nephrology is to achieve that 80% of the patients starting hemodialysis do it with an arteriovenous fistula. We want to review the causes of non-planned hemodialysis nowadays. In 2010, 43 patients had started chronic hemodialysis in the Hospital Ramón y Cajal in Madrid (Spain). Mean age was 61 years, 79% were men, the most frequent cause of chronic renal disease was the diabetes (23%) and Charlson Comorbidity Index was 6.3 ± 2.6. The unplanned hemodialysis occurred in 20 patients (47%), without any differences with the 23 patients who began planned hemodialysis, in none of the clinical or demographic parameters analyzed. The main cause of unplanned hemodialysis was the acute exacerbation of chronic kidney disease stage 3 or 4, previously stable, secondary to an unforeseeable intercurrent process (8 patients, 40% of the cases). One patient began after a non-recovery acute renal failure and in other 6 patients, the reason of unplanned hemodialysis initiation was not attributable to the operation Health System (in 3 cases unknown kidney chronic disease and in the other 3 cases it was patient´s responsibility). Only in 5 cases (25%), the cause could be corrigible. Most causes of unplanned hemodialysis does not come from the healthcare organization and therefore not easy to resolve it. Consequently, the objective of the Quality Group will be difficult to be achieved.
INTRODUCTION
The data from the Registro Catalán de Enfermos Renales (Catalan Renal Patient Register) and from a multi-centre Spanish study, both compiled in 1996-97, agreed that almost half of all patients (48% in the first study and 48.6% in the second one) started chronic haemodialysis treatment using a temporary vascular catheter.1,2 This unscheduled form of starting treatment is associated with increased morbidity and mortality rates, as well as higher health costs. Late transfer to the nephrology department was the primary risk factor for unscheduled initiation of haemodialysis.2
The Spanish Society of Nephrology (SEN) decided that the start of haemodialysis treatment under a scheduled protocol should be a priority objective for the efforts made in chronic kidney disease, which was reflected in various guidelines and documents. The consensus document of the Spanish Society of Family and Community Medicine indicated that all stage 4 chronic kidney disease patients should be referred for evaluation to a nephrology department.3 The Guía del Acceso Vascular (vascular access guidelines) recommends programming dialysis when the glomerular filtration rate drops below 20ml/min in order to ensure a four-six month window in the case of a native arteriovenous fistula, or four-six weeks in the case of a prosthesis.4 The Quality Management Group proposed the objective of at least 80% of the incident population starting haemodialysis with a definitive vascular access.5
Despite these measures, later publications indicate that the rate of patients that start unscheduled treatment using a venous catheter has not changed.6-9 The DOPPS study demonstrated a similar mean rate, which varied between 23% and 73%, according to country.10
The nephrology department has a specific predialysis unit that receives referred patients with stage 4/5 chronic kidney disease that are candidates for renal replacement therapy, excluding those with kidney transplants, where they receive information about the different dialysis modalities. The objective of this study was to analyse the current causes of unscheduled initiation of dialysis treatment. To this end, we have analysed all patients that started renal replacement therapy at our hospital during 2010.
MATERIAL AND METHOD
Ours was an observational, retrospective study of all patients that started periodical haemodialysis during 2010 at the Ramón y Cajal Hospital in Madrid, which corresponds to a health area of 536 000 inhabitants. Between 1 January and 31 December 2010, 66 patients required chronic renal replacement therapy. Four of them underwent a cadaveric kidney transplant before starting dialysis treatment, and 19 received scheduled peritoneal dialysis. The 43 remaining patients who started haemodialysis treatment were our study population.
We used the hospital data system to collect the following data: 1) baseline patient characteristics: age, sex, aetiology of the chronic kidney disease, Charlson’s comorbidity index, return to dialysis following failed kidney transplant, occupational situation, and follow up time by the nephrology department; 2) start of haemodialysis: scheduled (vascular access or definitive peritoneal access) or unscheduled (temporary venous catheter); 3) haemoglobin concentration and glomerular filtration rate (using the MDRD-4 formula) before the first haemodialysis session, and 4) causes for unscheduled initiation, defining five different categories: unrecovered acute renal failure; exacerbated chronic kidney disease, defined as stage 3/4 chronic kidney disease patients diagnosed within the 12 weeks prior to starting dialysis treatment, that were in an apparently stable clinical situation, but who suffered an unpredictable intercurrent process that triggered a deterioration of renal function; late transferral, defined as patients unknown to the nephrology department that were transferred for initiation of dialysis; delayed planning of the vascular access, defined as patients with stage 5 chronic kidney disease diagnosed in the nephrology department for more than 12 weeks before starting dialysis; and other causes.
Statistical analysis
Qualitative variables are expressed as percentages, and quantitative variables as mean (standard deviation [SD]). We compared quantitative variables using Student’s t-test, analysis of variance (ANOVA), and the non-parametric Mann-Whitney test, as appropriate. We used the chi-square test for qualitative variables. Values of P<.05 were considered to be statistically significant.
RESULTS
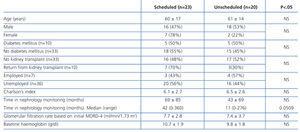
During 2010, 43 patients started haemodialysis treatment in our health area. Patients were male in 34 cases (79%) and nine were female (21%), with a mean age of 61 years (range: 32-85 years). The most common aetiology for renal failure was diabetic nephropathy (23%). The mean Charlson’s index value was 6.3 (2.6) (range: 2-11). At the time of starting haemodialysis treatment, seven patients were employed and manifested a desire to continue working. Ten patients (23%) had developed graft failure, and the remaining 33 (77%) were incident patients.
The start of HD treatment was scheduled in 23 patients (53%) and unscheduled in 20 (47%). We observed no differences between the two groups in terms of sex, age, aetiology of the nephropathy, transplant history, occupational situation, Charlson’s comorbidity index, glomerular filtration rate, or haemoglobin concentrations at the start of dialysis. The time spent previously in the nephrology department was higher in scheduled patients, with borderline statistically significant difference (Table 1). Of the 33 patients that did not have a kidney transplant, 16 had been attended to in a predialysis setting, and 81% of them had a scheduled start to dialysis, whereas this value was only 18% for patients who were not cared for at that unit (P<.001).
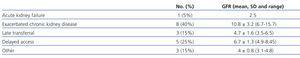
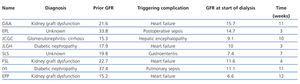
Table 2 shows the reasons for unscheduled initiation of haemodialysis. One patient suffered acute renal failure in the context of a multiple myeloma, with no functional recovery. Three patients were unknown to the nephrology department, and had been referred from the emergency department with uraemic symptoms (one of these was a foreigner that had been diagnosed with end stage renal disease in their country of origin and had come to Spain for treatment, and the other patients had not been seen in the hospital before either). The delay until the vascular access or peritoneal catheter was available was the cause in five patients, all of which had been monitored for more than one year in the nephrology department. A catheter was supposed to be implanted for peritoneal dialysis in two of these patients, but haemodialysis had to be started using a central venous catheter when uraemic symptoms appeared. The three other patients were awaiting arteriovenous fistulas that were scheduled four, five, and seven weeks before the start of renal replacement therapy. We should mention that the cause of unscheduled initiation of dialysis was the patient’s refusal to undergo dialysis treatment in one case, and two other cases had been lost to follow-up in nephrology and primary care programmes. The most common cause of unscheduled initiation was exacerbations of chronic kidney disease due to unpredictable intercurrent processes (40%). Table 3 summarises the characteristics of these patients. The 8 that started treatment for exacerbated chronic kidney disease did so with higher glomerular filtration rates than the other 12 patients (10.8 [3.2] vs 5.2 [1.8] ml/min/1.73m2; P=.0015).
Of the 20 patients that started unscheduled HD, four were later transferred to peritoneal dialysis by decision of the patient.
DISCUSSION
Of our patients, 53% started scheduled chronic HD treatment. This rate is similar to that described in other studies,6-9 but far from the objective of 80% proposed by the Quality Management Group of the SEN.5
In general, late transfer to the nephrology department and delayed vascular access or implantation of the peritoneal catheter were the two primary causes for the lack of scheduled initiation of renal replacement therapy, and are the targets for action plans to avoid the need for starting HD with a vascular catheter.10,11 However, in our study, none of these were primary causes. In 40% of our patients, the cause for unscheduled initiation of dialysis was exacerbations of clinically stable and diagnosed chronic kidney failure due to an intercurrent process that precipitated the need for starting dialysis. A recently published study obtained similar results to ours: rapid and unexpected decrease in renal function is the primary cause of unscheduled initiation of HD, this being more relevant than the length of time under monitoring by a nephrologist.12 The subpopulation of patients with chronic kidney graft dysfunction is a good example of this situation.
Patients that started unscheduled HD due to an exacerbation of diagnosed chronic kidney disease did so with a higher glomerular filtration rate than other patients. Two different causes could explain this fact: firstly, these patients required dialysis because of symptoms derived from associated complications, and secondly, the estimated glomerular filtration rate using formulas that use serum creatinine concentrations could be overestimated in situations where it increases rapidly.
Late transfer to nephrology did not stand out as a relevant cause: the three cases from our study had not previously been detected by the outpatient health care system and, as such, this cause cannot be attributed to defects in health care organisation. The delay in creating a vascular or peritoneal access was the cause for unscheduled initiation of haemodialysis in five cases (25%); they were patients with stage 5 chronic kidney disease found within the past 12 weeks, who were waiting for an arteriovenous fistula in three cases and a catheter for peritoneal dialysis in two patients. A vascular access should be available early, and patients frequently receive an arteriovenous fistula several months in advance; unscheduled initiation of dialysis due to delays in creating the vascular access is a very correctable cause. Peritoneal catheters present a different situation; they are not usually implanted several months in advance, but rather just one month before dialysis is to be started.13 This type of programming requires very strict patient monitoring and involves a risk of starting unscheduled renal replacement therapy, as occurred in two of our patients. In this situation, we prefer to start temporary HD treatment over unscheduled acute peritoneal dialysis.
It is said the unscheduled start of renal replacement therapy practically excludes the use of peritoneal dialysis as a therapeutic option.7,11 However, this is not an insurmountable obstacle, as four of the 20 patients that had unscheduled initiation of HD were later transferred to peritoneal dialysis.
In summary, our study shows that delayed planning of vascular access or peritoneal catheters was responsible for only 25% of unscheduled initiations of HD treatment. The other causes were out of the reach of hospital organisation, many of which were unpredictable and therefore difficult to ameliorate. The objectives of the Quality Management Group will be difficult to reach.
Table 1. Baseline characteristics of each subgroup according to the conditions for starting haemodialysis treatment
Table 2. Causes of unscheduled treatment with haemodialysis and glomerular filtration rates (ml/min/1.73 m²)
Table 3. Patients that started haemodialysis due to exacerbations of chronic kidney disease