Antecedentes: El impacto de cada episodio de peritonitis sobre la supervivencia a largo plazo de los pacientes en diálisis peritoneal (DP) está por definir. Objetivos: Establecer el riesgo que supone para la supervivencia de los pacientes y de la técnica de DP cada episodio de peritonitis. Pacientes: 1.515 pacientes incluidos en el registro Levante desde el uno de enero de 1993 hasta el 31 de diciembre de 2005. Métodos: Análisis retrospectivo de un registro multicéntrico mediante regresión de Cox para variables cambiantes en el tiempo. Resultados: Se analizaron 1609 episodios de peritonitis en 716 pacientes (47,2%). En el análisis univariante cada peritonitis tratada ambulatoriamente se asoció a un aumento de la mortalidad (hazard ratio [HR] 1,99; p <0,001) que fue mayor para los episodios que requirieron hospitalización (HR 3,62; p <0,001). La mortalidad aumentó con cada episodio sucesivo en el mismo paciente. El análisis multivariante confirmó la asociación de cada peritonitis con una menor supervivencia a largo plazo (HR 2,01; p <0,001), con un riesgo diferente para episodios por gram`positivos, gramnegativos y hongos (HR 1,73, 2,43 y 5,71, respectivamente; p <0,001). Otras variables asociadas con la mortalidad fueron la edad, una función renal residual escasa, la ausencia de acceso vascular y la comorbilidad. Las peritonitis fueron la única variable independiente asociada al fracaso de la técnica (HR 1,29; p <0,001), con un riesgo diferente para episodios por grampositivos, gramnegativos y hongos (HR 1,25, 1,30 y 3,03, respectivamente) (p <0,001). Conclusiones: Los episodios de peritonitis influyen de forma negativa en la supervivencia a largo plazo de los pacientes en DP.
Background: The impact of each episode of peritonitis on long-term survival of peritoneal dialysis (PD) patients has yet to be defined. Objectives: To determine the risk that each episode of peritonitis poses for patient survival and for the PD technique. Patients: 1515 patients included in the Levante registry from 1 January 1993 to 31 December 2005. Methods: Retrospective analysis of a multicentre registry using Cox regression for time-dependent variables. Results: We analysed 1609 episodes of peritonitis in 716 patients (47.2%). In the univariate analysis, each case of peritonitis treated in the outpatient unit was associated with an increase in mortality (hazard ratio [HR] 1.99, P<.001), which was greater for episodes that required hospitalisation (HR 3.62, P<.001). Mortality increased with each successive episode in the same patient. Multivariate analysis confirmed the association of each case of peritonitis with lower long-term survival (HR 2.01, P<.001), with a different risk for episodes due to gram-positive and gram-negative bacteria and fungi (HR 1.73, 2.43 and 5.71, respectively; P<.001). Other variables associated with mortality were age, low residual renal function, absence of vascular access and comorbidity. Peritonitis was the only independent variable associated with technique failure (HR 1.29, P<.001), with a different risk for episodes due to gram-positive and gram-negative bacteria and fungi (HR 1.73, 2.43 and 5.71, respectively; P<.001). Conclusions: Episodes of peritonitis negatively influence long-term survival of patients on PD.
INTRODUCTION
Peritonitis currently constitutes one of the primary causes of death and technique failure in peritoneal dialysis (PD) patients, in spite of the continued decrease in the incidence rate of this complication.1-6 Fortunately, the direct mortality associated with episodes of peritonitis is low, below 4% according to most studies.5,6 This rate of lethality depends greatly on the causative micro-organism, and is highest for fungal peritonitis, followed by those due to gram-negative bacteria.6-10 The potential influence of episodes of peritonitis on the mortality of PD patients on a long-term basis is much less well understood. In fact, we only know one study in which this specific aspect has been analysed in detail.11 This study was published in 1996 when only 30% of patients used disconnect systems, a situation quite different from the current one.11 Additionally, until now, no study has been carried out in the survival of PD patients that has analysed the incidence of peritonitis as a time-dependent variable, with the previous literature on the subject limited to studies using the final rate of peritonitis as their study variable.11,12 As such, from a methodological point of view, no study has been able to estimate the increased risk of death or technique failure that each episode of peritonitis causes when these infections occur. We must keep in mind that in addition to the direct mortality attributable to peritonitis, each case also involves an inflammation state that will generate both a deleterious effect on the peritoneal membrane and a decrease in the PD patient’s general health and immunological and nutritional states. This could potentially affect the survival of the large majority of patients that overcome their episodes of peritonitis and remain on the dialysis technique.
Since 1991, the Levante registry has prospectively compiled an ample database of demographic and clinical information on all patients that start renal replacement therapy with PD in the public sector in the three provinces of the Community of Valencia (Alicante, Castellón, and Valencia), the community of Murcia, and the provinces of Albacete and Cuenca. In the present study, we analysed a large cohort of patients included in the Levante registry to estimate the long-term survival of PD patients after each case of peritonitis using analysis techniques for time-dependent variables. We also estimated the potential differences in long-term mortality based on the type of micro-organism causing the infection.
MATERIAL AND METHOD
We performed a retrospective analysis of all episodes of peritonitis registered in a total of 1515 incident patients from the Levante registry that started PD using disconnect systems between 1 January 1993 and 31 December, 2005. In addition to the information provided on the episodes of peritonitis (date of diagnosis, culture from the dialysis effluent, and the need for hospitalisation), we used demographical and clinical data from all patients upon starting PD, and at least one analysis of peritoneal permeability and adequacy in a sample of 1180 patients (77.9% of the total). Some 2577 studies were performed during the follow-up period. We considered peritonitis to be any episode of turbid peritoneal effluent with a pathological cell count, defined as more than 100 leukocytes/mm3 with a polymorphonuclear neutrophil percentage greater than 50%.13 Comorbidity at the start of PD was estimated by calculating the Davies index14 for the 14 comorbidities compiled in the Levante registry.
Statistical analysis
We performed a descriptive analysis of the continuous variables of the sample using means and standard deviations, comparing between groups using the Mann-Whitney U test. Qualitative variables were analysed using chi-square tests. In all cases, the null hypothesis was rejected whenever its probability was less than 0.05 (P<.05).
Survival analysis
We performed a survival analysis, considering only patient death. We estimated technique survival by considering only the event of switching to haemodialysis (HD). All other events in both cases were censored. We calculated mortality rate (deaths/100 patient-years) by dividing the total number of deaths registered in a period of time by the number of at-risk days for all patients within that period, dividing by 365.25 and multiplying by 100. The rate of technique failure within a given period was calculated in the same way, considering the number of patients that switched to HD during that time. Those patients that died during the first month after transferring to HD were considered to have died on PD. Direct mortality from peritonitis was defined as all deaths that occurred within 4 weeks of an episode of peritonitis, regardless of the immediate cause of death. For the univariate analysis of continuous variables, we performed a “dummy” transformation into categorical variables according to statistical and/or clinical criteria for later analysis using Kaplan-Meier curves, comparing between strata using log-rank tests. We analysed the impact of episodes of peritonitis as well as other time-dependent variables (PD technique used, use of icodextrin, and variables associated with peritoneal kinetics and adequacy) on survival, using Cox-regression models for time-dependent covariates. In this analysis, each event is related to the value of the previous variable, such that the resulting Cox model represents the instantaneous relative risk when comparing two different patients with the same follow-up time when one of them changes levels. In order to represent the univariate effect of the time-dependent variables, we used Kaplan-Meier curves with delayed-entry study. They represent survival as if a patient was in the same category of the study variables during the entire study period. The proportionality of risks that the Cox regression analysis requires was confirmed using Kaplan-Meier curves and a graphical representation of the log-transformed incidence rate by time according to each case. All fixed or time-dependent variables with a significant (P<.05) or almost significant (P≤.1) value for survival in the univariate study were selected for a multivariate analysis using backwards stepwise conditional Cox regression. We developed two different multivariate models: the first was to estimate the risk of mortality associated with each episode of peritonitis, and the second was to analyse patient survival based on the causative micro-organism. In this last model, we decided to exclude episodes caused by mycobacteria (because of the small number: 7 cases) and those that produced a negative cell culture, since this was a heterogeneous group. Additionally, in accordance with previously existing literature on the subject, we decided to consider mixed infections as gram-negatives whenever a gram-negative bacteria was isolated, and fungal whenever at least one fungal species was isolated.11 We performed all statistical analyses using “R” statistical software, version 2.8.0 (The R Foundation for Statistical Computing) and SPSS version 13.0 (SPSS Inc., Chicago, Illinois, USA).
RESULTS
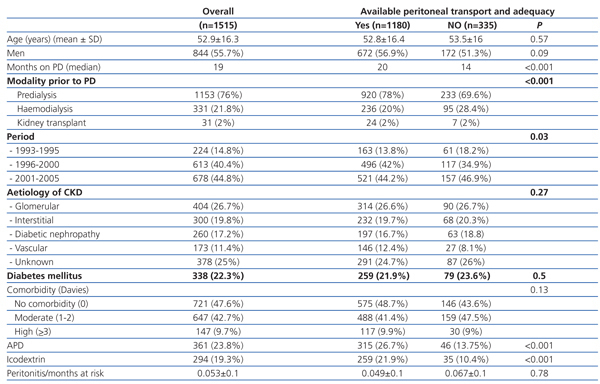
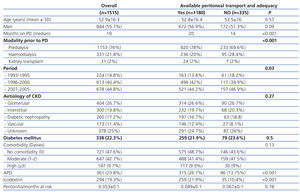
We analysed a total of 1515 incident patients with a cumulative time on PD of 3213.7 years. The primary characteristics of the cohort are compiled in Table 1. In a sample of 1180 patients (77.9%), we had access to at least one peritoneal transport and adequacy study. The characteristics of this sample and the differences with other patients appear summarised in Table 1. The baseline peritoneal transport and adequacy values were the following: weekly peritoneal Kt/V: 1.54±0.4; weekly renal Kt/V: 0.9±0.7; estimated glomerular filtration rate (average of urea and creatinine clearance rates): 5.08±4.08ml/min; nPCR: 1.08±0.3g/kg/day; D/P creatinine: 0.67±0.1. At the end of the study, 402 patients (26.5%) were still on PD, 386 (25.5%) had died, 367 (24.2%) received a kidney transplant, 308 (20.3%) were transferred to HD, and 52 (3.4%) were lost during the follow-up period. Mean patient survival was 63 months (95% confidence interval [CI]: 53.8-72.2), with a survival rate of 91%, 72%, 52%, and 23% at 1, 3, 5, and 10 years, respectively. Global mortality was 11.7 deaths per 100 patient-years. The cause of death was cardiovascular in 128 cases (33.2%), associated with peritonitis in 58 cases (15%), cachexia in 51 cases (13.2%), non-peritoneal infection in 47 cases (12.2%), miscellaneous in 30 cases (7.8%), and unknown in 72 cases (18.6%). Mean technique survival was 89.14 months (95% CI: 82.22-96.07), with a rate of 92%, 74%, 63%, and 37% at 1, 3, 5, and 10 years, respectively. The rate of transferral to HD was 9.4 cases per 100 patient-years on PD. Peritonitis was the primary cause of technique failure with 111 cases (36.4%).
During the follow-up period, we diagnosed 1609 episodes of peritonitis in 716 patients (47.2%); 339 patients (22.3%) developed one episode, 163 patients (10.7%) had two, 91 patients (6%) had three, and 123 patients (8.1%) had four or more episodes. The global rate of peritonitis was one episode per 24 patient-months (one episode for every 18.3, 24.5, and 29 patient-months for the periods of 1993-1995, 1996-2000, and 2001-2005, respectively). The lethality rate was 3.6%. Gram-positive bacteria were the most common causative micro-organisms with 902 cases of peritonitis (56% of the total), 129 of which were Staphylococcus aureus (8%). Gram-negative bacteria showed up in cultures in 339 episodes (21%), including 87 cases of Pseudomonas spp. (5.4%). In 63 cases, we observed a mixed culture of gram-positive and gram-negative bacteria (4.3%). The episode was caused by a fungus in 59 cases (3.6%), and mycobacteria were implicated in 7 cases (0.7%). The culture of the effluent was negative in 239 cases (14.8%). In 956 cases (59.4%), treatment was given in an outpatient setting, whereas 653 episodes (40.6%) required hospitalisation.
Patient survival
Univariate analysis
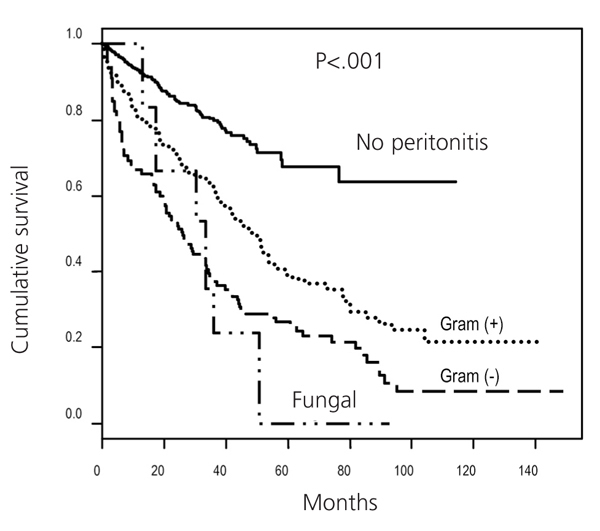
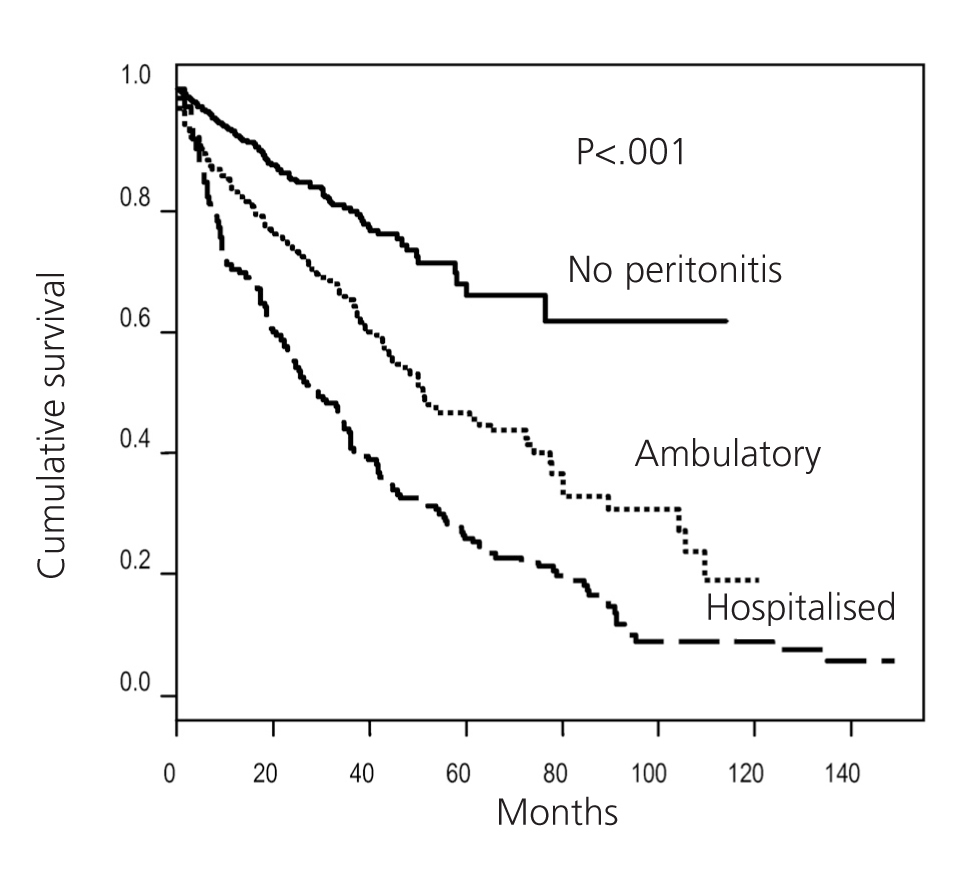
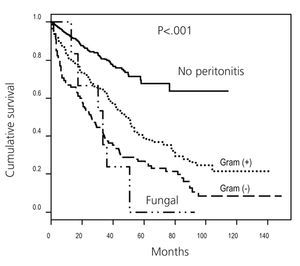
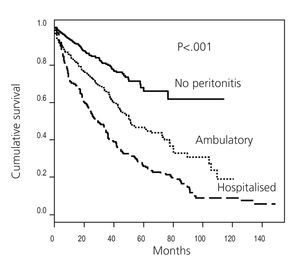
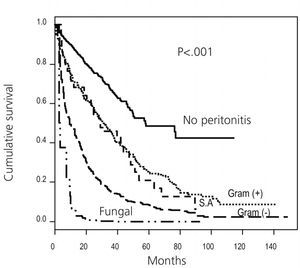
Mean patient survival with a rate of peritonitis equal to or greater than one episode every 24 months was 57 months (95% CI: 51.1-62.9), significantly lower than patients with a lower incidence of peritonitis (83 months; 95% CI: 74.9-91.1; P<.001). The analysis of each case of peritonitis as a time-dependent variable confirmed that each episode was associated with a higher risk of death that increased progressively as episodes occurred to the same patient. Thus, the first episode was associated with a hazard ratio (HR) of 2.08 (95% CI: 1.59-2.72; P<.001); the second had a HR of 2.72 (95% CI: 1.92-3.85; P<.001), the third had a HR of 3.18 (95% CI: 2.07-4.88; P<.001), the fourth had a HR of 4.76 (95% CI: 2.94-7.62; P<.001), and the fifth and the following ones had a HR of 7.87 (95% CI: 5.16-12; P<.001). This increased risk of mortality was greatest for patients with fungal infections (HR: 14.29; 95% CI: 7.97-25.65; P<.001), followed by episodes caused by gram-negative bacteria (HR: 3.56; 95% CI: 2.62-4.83; P<.001), with the lowest risk associated with episodes caused by gram-positive bacteria (HR: 2.23; 95% CI: 1.72-2.90; P<.001) (Figure 1). The estimated long-term risk of mortality after an episode of peritonitis from Staphylococcus aureus (HR: 2.25; 95% CI: 1.37-3.70; P=.001) was similar to the rest of the gram-positive bacteria (HR: 2.23; 95% CI: 1.69-2.93; P<.001). Additionally, the need for hospitalisation during the episode of peritonitis was also associated with increased long-term mortality (HR: 3.62; 95% CI: 2.78-4.72; P<.001), although even those episodes treated in the outpatient setting were associated with a significantly lower long-term survival rate (HR: 1.99; 95% CI: 1.53-2.60; P<.001) (Figure 2). In addition to the cases of peritonitis, the variables that showed a significant association in the univariate analysis with increased mortality were age (P<.001), inclusion on PD before 2001 (P<.001), previous time spent on HD (P<.001), the absence of an adequate vascular access for HD as the reason for choosing PD (P<.001), the cause of the CKD (P=.002), comorbidity as measured by the Davies index (P<.001), the use of icodextrin (P=.035), a D/P creatinine index (D/P creat) greater than 0.65 (P=.002), a nPCR less than 1g/kg/day (P<.001), and residual renal function (RRF) less than 3ml/min (P<.001).
Multivariate analysis
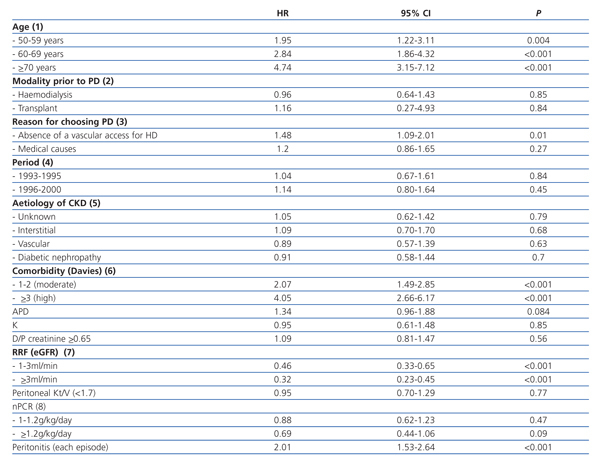
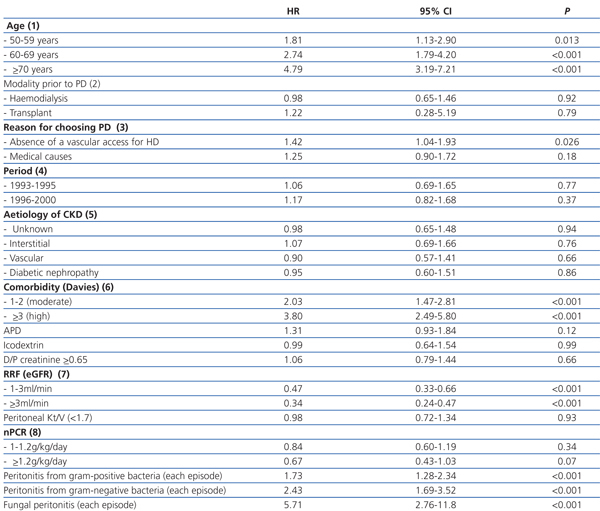
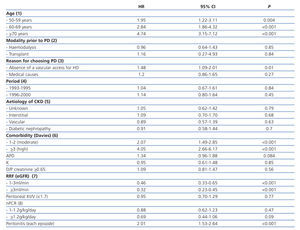
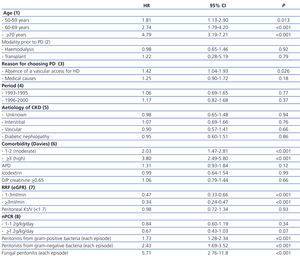
In the first multivariate model, we confirmed that each case of peritonitis increases the long-term risk of mortality with an adjusted HR of 2.01 (95% CI: 1.53-2.64; P<.001) (Table 2). The second multivariate model demonstrated how the risk of death appears after fungal peritonitis cases (adjusted HR: 5.71; 95% CI: 2.76-11.8; P<.001), with lower rates associated with cases of gram-negative bacteria (adjusted HR: 2.43; 95% CI: 1.69-3.52; P<.001) and gram-positive bacteria (adjusted HR: 1.73; 95% CI: 1.28-2.34; P<.001) (Table 3). Other independent risk factors associated with reduced survival in both models were age, the absence of an adequate vascular access point for HD, comorbidity, and a low or non-existent RRF (Table 2 and Table 3).
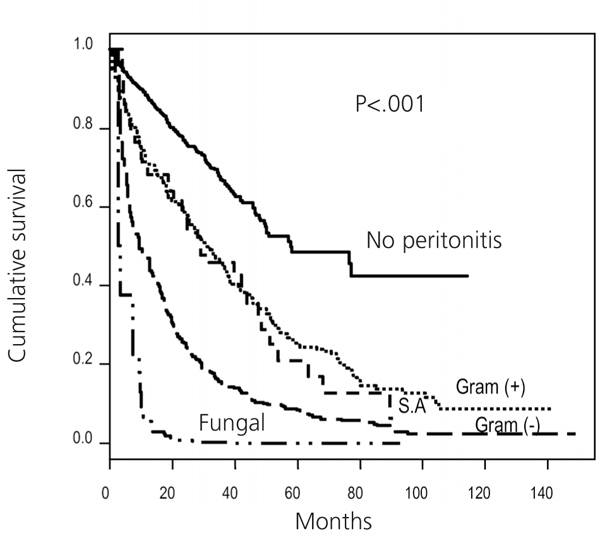
Technique survival
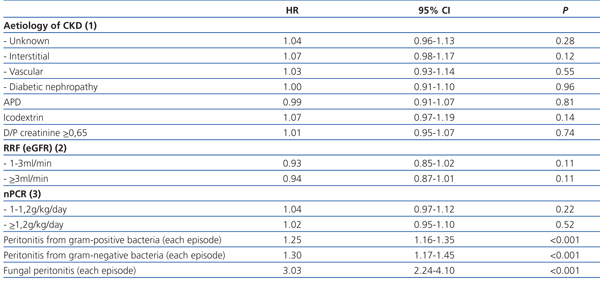
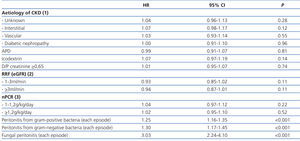
Mean technique survival was significantly lower in patients with a higher incidence of peritonitis than the mean of one episode every 24 months (69.9 months; 95% CI: 61.8-78) as compared to patients with a lower incidence of peritonitis (101.2 months; 95% CI: 92.8-109.5; P<.001). The univariate analysis also showed that the risk of technique failure increased in relation to the number of episodes of peritonitis experienced by the same patient, with an HR of 2.21 for the first episode (95% CI: 1.80-2.70; P<.001), 3.35 for the second (95% CI: 2.60-4.31; P<.001), 4.19 for the third (95% CI: 3.09-5.69; P<.001), 4.46 for the fourth (95% CI: 3.02-6.59; P<.001), and 8.50 from the fifth episode on (95% CI: 6.11-11.81; P<.001). Additionally, the risk of transferring to HD was different for the episodes resulting from gram-positive bacteria (excluding Staphylococcusaureus) (HR 2.09; 95% CI: 1.69-2.59; P<.001), Staphylococcus aureus (HR: 2.34; 95% CI: 1.61-3.39; P<.001) gram-negative bacteria (HR: 4.01; 95% CI: 3.20-5.03; P<.001), and fungal infections (HR: 29.76; 95% CI: 21.31-41.58; P<.001) (Figure 3). Other factors associated with technique failure in the univariate analysis were the cause of the chronic kidney disease (CKD) (P=.04), the use of automated peritoneal dialysis (APD) (P=.001), the use of icodextrin (P=.02), a D/P creatinine index greater than 0.65 (P=.002), an RRF less than 3ml/min (P=.001), and nPCR values less than 1g/kg/day (P=.04). The multivariate analysis confirmed that the episodes of peritonitis were the only factor independently associated with technique survival, with an adjusted HR of 1.29 (95% CI: 1.21-1.38; P<.001), and this risk varied by the type of infectious micro-organism involved (Table 4).
DISCUSSION
The lack of a correct analysis of time-dependent variables is the cause of serious bias that can affect the results of many observational studies published even in upper-tier journals.15 In this study, we analysed episodes of peritonitis for the first time as a time-dependent variable with the objective of estimating the potential impact of this occurrence on mid-long-term technique failure and mortality in PD patients. Our results show that peritonitis does not only affect short-term patient survival, but also that it has long-term impact on the majority of patients that respond to treatment and overcome the original infection. Additionally, this increased risk of death and/or technique failure associated with peritonitis is independent of the presence of other well-known prognostic factors, such as advanced age, comorbidity, and absence of RRF.16-18 Until now, very few studies have evaluated the impact of peritonitis on long-term survival of PD patients.11,12 Fried, et al studied the influence of peritonitis on mortality in 516 patients in a single PD unit, demonstrating lower survival rates in patients with more than one episode of peritonitis every 25 months.11 More recently, Sipahioglu et al published their experience with 423 patients, also from one single centre, demonstrating an increased risk of death in patients with a higher incidence of peritonitis (adjusted HR: 1.87 for each increase of one episode per year on PD).12 For the first time, and through the application of regression techniques for time-dependent variables, our study has been able to estimate the mean increase in risk of death that each episode of peritonitis accounts for, also adjusting for other significant variables (HR: 2.01; 95% CI: 1.53-2.64). Even more so, our results show that the several episodes of peritonitis in the same patient progressively increase the negative impact of this complication on survival. It is important to point out that even those episodes that are treated in the outpatient setting (because the patient has a good clinical situation with proper response to treatment) are later associated with a significant increase in mid-long-term mortality. The deleterious effect of peritonitis episodes on mid-long-term patient survival could be explained by their potential contribution to the development of malnutrition-inflammation-atherosclerosis syndrome (MIA).19 In this context, a recent study showed that each episode of peritonitis causes an increased inflammatory state in PD patients that lasts much longer than the clinical resolution of the peritonitis itself.20 This inflammation state, with the serological translation of increased PCR levels, is accompanied by nutritional deterioration that manifests itself in the form of decreased body mass index, which could also be caused by the concomitant increase in serum leptin levels because of the known anorectic activity of this compound.20 All of these alterations would still be present even six weeks after the complete clinical remission of the episode, with continued nutritional deterioration and prealbumin levels still below those from before the infectious event.20 Thus, each case of peritonitis would lead to a deteriorated nutritional state of the patient and would exacerbate the previous inflammatory state, enhancing the development of atherosclerosis and increasing cardiovascular risk.19 Precisely, the persistence of increased serum PCR levels following the resolution of the episode of peritonitis has be correlated with lower survival a posteriori both in the short and long term.20-22 In this context, it is interesting to point out how even in studies that only analysed direct short-term mortality attributed to each episode of peritonitis a cardiovascular complication was the immediate cause of death in as many as 41.5% of cases.8 Finally, it has been suggested that the sustained inflammation and its exacerbations during episodes of peritonitis could contribute to the progressive loss of RRF, thus indirectly affecting patient survival.23,24 In any case, our study shows that the association between peritonitis and long-term patient survival is independent of the patient’s RRF at the time of the episode. Even more so, our study was able to detect significant differences in survival from each episode of peritonitis based on the causative micro-organism. Thus, fungal peritonitis episodes have the greatest impact on mortality, followed by episodes caused by gram-negative bacteria and finally gram-positive bacteria (Figure 3 and Table 3). Until now, only the study mentioned by Fried et al had analysed the impact of the causative micro-organism on long-term patient survival in PD patients, with similar conclusions.11 All other studies have focused on the immediate mortality rates associated with the episode or the rate of lethality,4,7,25 all of which resulted in greater mortality rates for cases of fungal peritonitis, followed by those caused by gram-negative bacteria. As such, an in accordance with the previously published studies and our own results, we can conclude that the different short-term profile of clinical aggressiveness of the different causative micro-organisms is maintained if we consider a more long-term evaluation of patient survival.
In our study, the episodes of peritonitis are the only variable that was independently associated with technique survival on PD. Although increased peritoneal transport and loss of RRF were significantly associated with technique survival in the univariate analysis, both factors lost this association in the multivariate analysis, which suggests that the use of APD could contribute to the treatment of high transporters and anuric patients to facilitate remaining on the technique under proper conditions.26,27 Additionally, if we take into consideration that the incidence of peritonitis was not included in the majority of previous studies on survival, it is plausible to consider that the association described in other studies between low RRF and technique failure could be explained at least in part by the lower incidence of peritonitis described in patients with a higher RRF,28 or even by the contribution that these episodes make to the loss of RRF.23,24 In a similar manner, the fact that the use of icodextrin solutions and APD is associated with lower technique survival in the univariate analysis, but not the multivariate analysis, suggests a probable selection bias of both therapeutic options for those patients with less favourable conditions for the long-term application of PD.
Given the important negative impact that peritonitis has on patient survival and PD technique failure, it is important to point out that our study observed a progressive decrease in peritonitis rates throughout the study period.
Our analysis of data from a registry had several limitations. Although all of the data used were compiled prospectively, the retrospective nature of our analysis and the fact that we did not have information regarding the adequacy of treatment and peritoneal transport in 335 patients (22.1%) may lead to a possible selection bias. However, the large sample analysed, the long follow-up period, and the fact that the sample analysed using the multivariate analysis had no significant differences in the primary variables associated with survival show that the results obtained were absolutely representative. On the other hand, we should also point out that although the models for time-dependent variables that we used allowed for estimating long-term risk of technique failure or death, the resulting indexes are also influenced by events that occur in the short-term, which should be taken into account in the interpretation of the results.
In summary, our study showed that each episode of peritonitis is independently associated with an increase in mortality and technique failure, both on the short and long term. As such, our results suggest that the incidence of peritonitis should be a key risk factor in all survival analyses in the field of PD. Finally, the importance of minimising the incidence of peritonitis in order to improve patient survival must be prioritised.
Table 1. Characteristics of the 1515 incident patients on peritoneal dialysis and the sample of 1180 patients with information on peritoneal transport and adequacy included in the multivariate analysis
Table 2. First multivariate model using Cox regression with the predictive factors for mortality in 1180 incident patients on peritoneal dialysis
Table 3. Second multivariate model using Cox regression with the predictive factors for mortality in 1180 incident patients on peritoneal dialysis
Table 4. Cox multivariate regression analysis of the predictive factors for technique failure in 1180 incident patients on PD
Figure 1. Estimate of patient survival after each episode of peritonitis based on the result of the effluent culture
Figure 2. Estimate of patient survival after each episode of peritonitis based on the need for hospitalisation.
Figure 3. Estimate of technique survival after each episode of peritonitis based on the result of the effluent culture.