Patients with chronic renal failure may present multiple cutaneous manifestations such as pruritus, xerosis, cutaneous pigmentation, metastatic calcinosis cutis, calciphylaxis, pseudoporphyria and late cutaneous porphyria. Grover's disease (GD) must also be included in the differential diagnosis of cutaneous lesions in these patients.
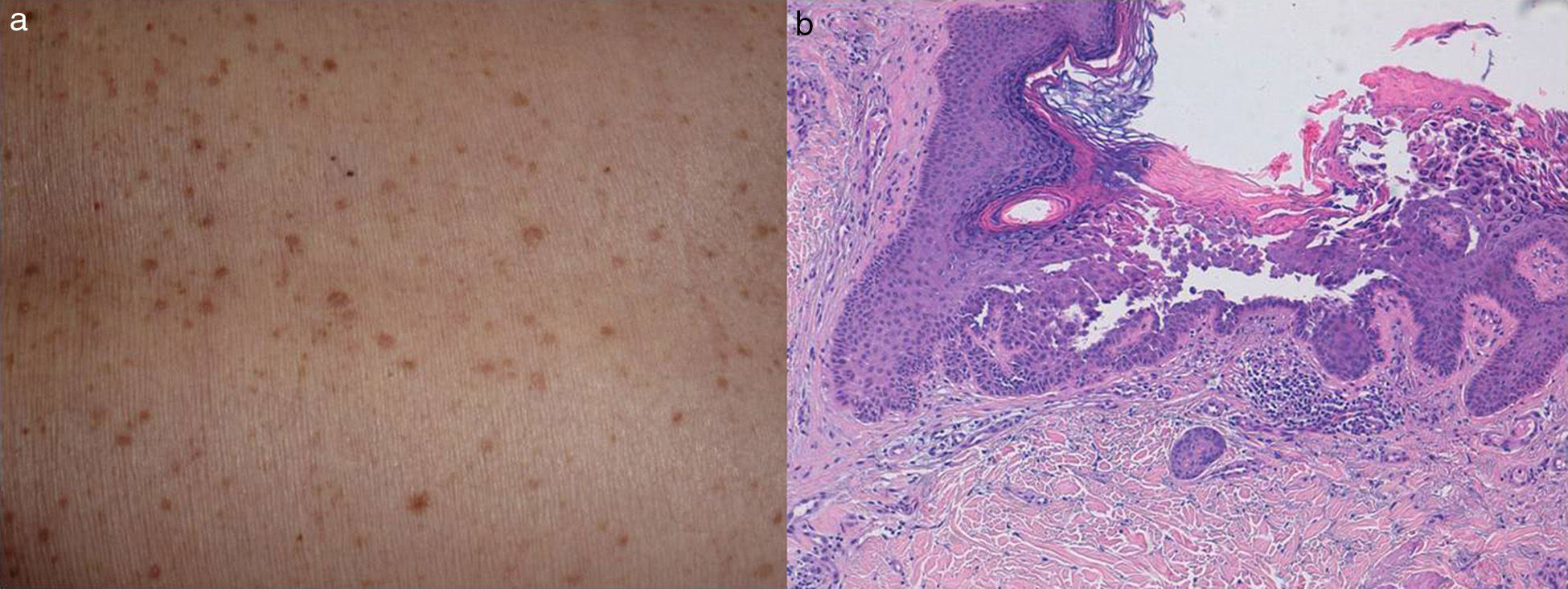
We are presenting a case of a 69-year-old woman who presented with one and a half moth of cutaneous lesions in the back with moderate itching. She had no personal or family history of skin pathology. She had been receiving haemodialysis for five months due to Good pasture syndrome induced rapidly progressive renal failure. During the previous months, she had been treated with plasmapheresis, IV cyclophosphamide and IV methylprednisolone. At the time of consultation, her treatment included prednisone 5mg/day, calcitriol 0.25mg/day, omeprazol 20mg/day, enoxaparin sodium 20mg 3days/week and darbepoetin alfa 30mcg weekly. Physical examination shows non-confluent papular erythematous lesions with keratotic surface, located in the back (Fig. 1a). She did not have lesions on palms or soles, back of the hands or the oral mucosa. She did not have a facial or scalp lesions either. Microscopic evaluation showed areas of hyperkeratosis with parakeratosis, acanthosis and focal acantholysis with presence of round and granular lesions (Fig. 1b). Taking into account the almost asymptomatic character of the lesions, the patient preferred to adopt an expectant attitude. Three months later, the lesions disappeared spontaneously. The absence of a previous family history, the onset at an adult age, and the spontaneous resolution of the symptoms led to the diagnosis of GD.
GD, also known as persistent or transient acantholytic dermatosis, is a rare condition characterised by the presence of small papules and papulo-vesicles, of the same color as normal skin or erythematous and pruritic, which usually affect the back. The disease is usually transient and resolves spontaneously within weeks. In some cases, lesions may be recurrent or persist throughout years. The histological changes are characterized by focal acantholysis and dyskeratosis. Four histological patterns have been identified: Darier type, Haley–Haley type, pemphigus and spongiotic type.1
The aetiology of GD is unknown. Fever or prolonged bed rest, sweating or excessive heat, exposure to UV radiation, treatment with ionizing radiations, xerosis, some drugs, chronic renal failure and immunosuppression have been associated with this disease.2
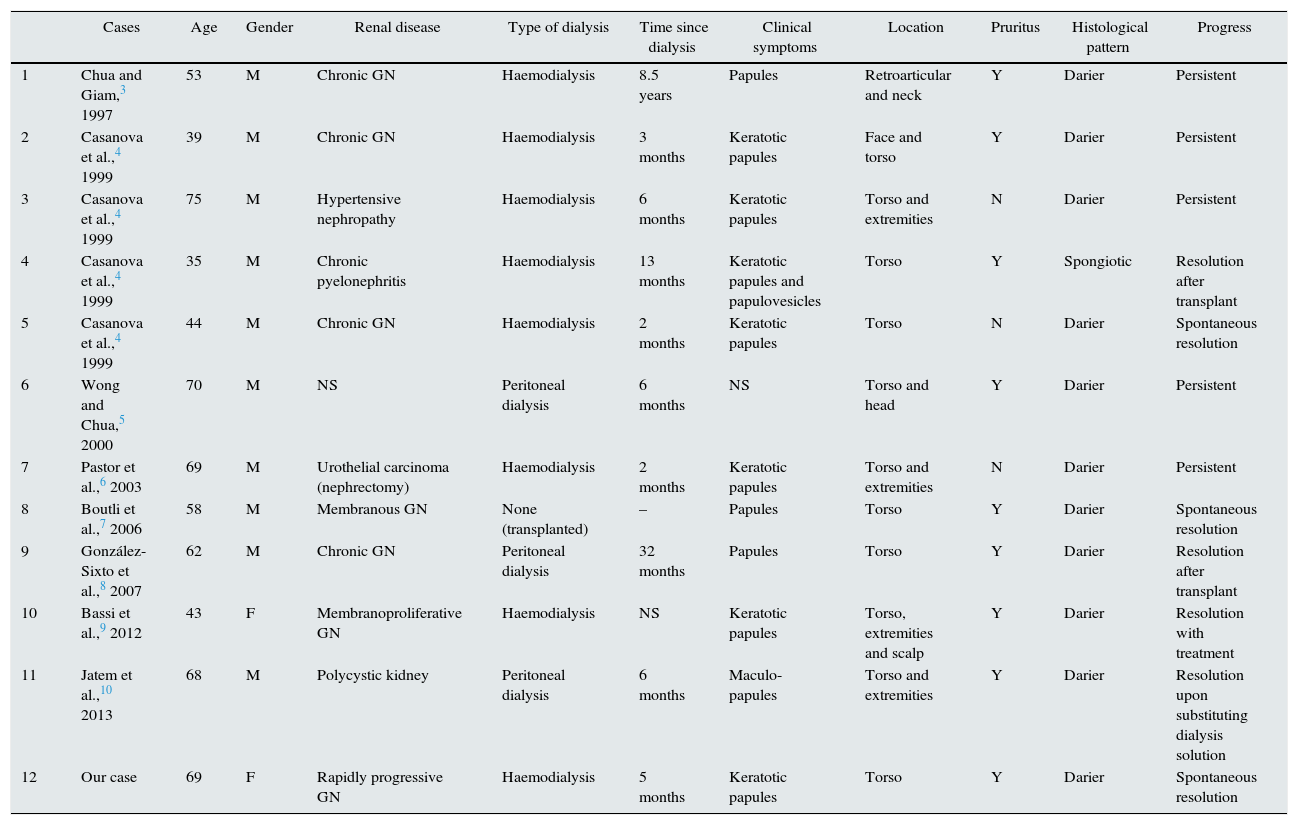
To date, including our case, there has been twelve cases published of GD associated tochronic renal failure (Table 1).3–10 The mean age has been 57 years and, except for two cases, all of them were men. The normal presentation was keratotic, pruritic papules located in the back. In three cases, the lesions were asymptomatic.4,6 The head was affected in four patients3–5,9 and in one of them it was the only location.3 The cause of renal failure was variable. In eleven cases the lesions appeared when the patient on regular haemodialysis (7 cases) or peritoneal dialysis (3 cases) and in one case the disease manifested itself after kidney transplant. The mean time from the beginning of dialysis until the appearance of the lesions varied from months to eight and a half years. The most frequent histopathological pattern was the Darier type. Evolution was variable and there is a poor response to the treatment. In seven cases the lesions were transient and in five persisted. Among patients with transient lesions, in three cases resolved spontaneously,4,7 in one after treatment,9 in two cases the lesions reoccur after kidney transplant4,8 and in one patient they resolved after changing the dialysis solution.10
Grover cases of chronic renal failure disease reported in literature.
| Cases | Age | Gender | Renal disease | Type of dialysis | Time since dialysis | Clinical symptoms | Location | Pruritus | Histological pattern | Progress | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Chua and Giam,3 1997 | 53 | M | Chronic GN | Haemodialysis | 8.5 years | Papules | Retroarticular and neck | Y | Darier | Persistent |
| 2 | Casanova et al.,4 1999 | 39 | M | Chronic GN | Haemodialysis | 3 months | Keratotic papules | Face and torso | Y | Darier | Persistent |
| 3 | Casanova et al.,4 1999 | 75 | M | Hypertensive nephropathy | Haemodialysis | 6 months | Keratotic papules | Torso and extremities | N | Darier | Persistent |
| 4 | Casanova et al.,4 1999 | 35 | M | Chronic pyelonephritis | Haemodialysis | 13 months | Keratotic papules and papulovesicles | Torso | Y | Spongiotic | Resolution after transplant |
| 5 | Casanova et al.,4 1999 | 44 | M | Chronic GN | Haemodialysis | 2 months | Keratotic papules | Torso | N | Darier | Spontaneous resolution |
| 6 | Wong and Chua,5 2000 | 70 | M | NS | Peritoneal dialysis | 6 months | NS | Torso and head | Y | Darier | Persistent |
| 7 | Pastor et al.,6 2003 | 69 | M | Urothelial carcinoma (nephrectomy) | Haemodialysis | 2 months | Keratotic papules | Torso and extremities | N | Darier | Persistent |
| 8 | Boutli et al.,7 2006 | 58 | M | Membranous GN | None (transplanted) | – | Papules | Torso | Y | Darier | Spontaneous resolution |
| 9 | González-Sixto et al.,8 2007 | 62 | M | Chronic GN | Peritoneal dialysis | 32 months | Papules | Torso | Y | Darier | Resolution after transplant |
| 10 | Bassi et al.,9 2012 | 43 | F | Membranoproliferative GN | Haemodialysis | NS | Keratotic papules | Torso, extremities and scalp | Y | Darier | Resolution with treatment |
| 11 | Jatem et al.,10 2013 | 68 | M | Polycystic kidney | Peritoneal dialysis | 6 months | Maculo-papules | Torso and extremities | Y | Darier | Resolution upon substituting dialysis solution |
| 12 | Our case | 69 | F | Rapidly progressive GN | Haemodialysis | 5 months | Keratotic papules | Torso | Y | Darier | Spontaneous resolution |
Although the reason why GD appears in patients with chronic renal failure is unknown, it has been stated that the decrease in sweat secretion, cutaneous xerosis and the obstruction of sweat ducts may act as triggering factors. In our patient, the treatment with cyclophosphamide and methyl prednisolone previously administered in order to treat her kidney disease could also have played a role in the development of the lesions. The association of GD with other states of immunosuppression,, such as HIV infection, bone marrow transplant, and several haematological and non-haematological malignancies has been described.
With respect to treatment, in the mildest cases, an expectant attitude can be adopted since the disease usually resolves spontaneously. Sun exposure and other triggering factors such as physical exercise and heat should be avoided. If treatment is necessary, corticosteroids, calcipotriol, or calcineurin inhibitors may be used topically as the first-line of drugs. Antihistamines should be used to reduce symptoms. For refractory cases, corticosteroids, oral retinoids and phototherapy can been used.
GD should be taken into account in the differential diagnosis of the cutaneous lesions in patients with chronic renal failure, specifically in those patients on haemodialysis or peritoneal dialysis.
Please cite this article as: Rodríguez-Pazos L, Vilas-Sueiro A, González-Vilas D, Durana C. Enfermedad de Grover en fracaso renal crónico. Nefrologia. 2015;35:331–334.