To analyze evolution of Chronic Kidney Disease stage 4–5 (ACKD) patients and influence of the information they receive (educational process, EP) in modality Renal Replacement Therapy (RRT) or conservative treatment (CT) in multidisciplinar ACKD outpatient clinic.
Material and MethodsProspective, multicenter study (3 centers). Inclusion: from June-01-2014 to October-01-2015; observation: 12 months or until start RRT or death if they occur before 12 months; ends October-01-2016.
Results336 patients were included (60 % males), median and intercuartile rank 71.5 (17), 55 % ≥70 years; Follow up initiation eGFR CKD-epi: 21 (9)ml/min/1.73m2; Charlson Index (ChI) with/without age 8 (3)/4 (2); Diabetic patients: 52,4%. The EP was carried out in 168, eGFR 15 (10)ml/min/1.73m2. The initial treatment election: Kidney trasplant 3%, 26 % peritoneal dialysis (PD), 45 % hemodyalisis (HD), 26 % CT; 60 patients started RRT: 3.3% kidney traspant; 30% PD, 66% HD; 104 hospital admissions in 73 patients, the most frequent cause: cardiovascular disease (42 %). Decesed: 23 patients (6.8 %). Age higher 78.4 (6) vs 67.8 (13.4) years p<0.001, ChI higher 9.8 (2.1) vs 7.4 (2.5) p<0.001. All deceased who received EP had chosen CT; 61 % of deceased had at least one hospital admission vs 39 % alive (p<0.001). Cox regression: age and hospital admissions were the predictive mortality variables.
ConclusionsThe population of ACKD patients is elder, comorbid, with high hospitalizations rate. The PD election is higher than usual. The EP has been very useful tool and has favored the PD choice.
Analizar la evolución de los pacientes con enfermedad renal crónica estadios 4 y 5 (ERCA) e influencia de la información (proceso educativo: PE) recibida para la elección de la modalidad de tratamiento renal sustitutivo (TRS) o tratamiento conservador (TC) en la consulta multidisciplinar de ERCA.
Material y MétodosEstudio prospectivo, multicéntrico (3 centros españoles). Pacientes incidentes consulta ERCA desde 1-6-2014 a 1-10-2015; observación: 12 meses o inicio del TRS o exitus si antes de los 12 meses; finaliza 1-10-2016.
Resultados336 pacientes (60% varones), mediana y rango intercuartil: edad 71,5(17) años (55% ≥ 70 años. FGe CKD-epi inicio 21(9)ml/min/1,73m2, Índice de Charlson (ICh) con/sin edad 8 (3) / 4 (2). Pacientes diabéticos: 52,4%. Recibieron PE 168 pacientes, FGe al inicio 15(10)ml/min/1,73m2. Tratamiento inicial elegido: trasplante renal 3%, 26% diálisis peritoneal (DP), 45% hemodiálisis (HD), 26% TC; 60 pacientes iniciaron TRS: 3.3% trasplante renal, 30% DP, 66% HD. Ingresos:104 en 73 pacientes, la causa más frecuente fue por patología cardiovascular (42%). Fallecidos: 23 pacientes (6.8%), mayor edad (78,4 (6), vs 67,8 (13,4) años p<0,001), ICh más elevado 9,8 (2,1) vs 7,4 (2,5) p<0,001). Todos los fallecidos con PE habían decidido TC; 61% de los fallecidos tenían al menos un ingreso hospitalario vs 39% vivos (p<0,001). Regresión Cox: variables predictivas mortalidad: edad e, ingresos hospitalarios.
ConclusionesLa población de ERCA es añosa, comórbida y con elevado índice de ingresos hospitalarios. La inicidencia de DP es mayor a la habitual. El PE ha sido una herramienta de gran utilidad y favorece la elección de diálisis peritoneal.
Chronic kidney disease (CKD) is a public health problem with a progressive increase in prevalence mainly due to the aging of the population, with a significant associated morbidity and treatments of high economic cost.1,2 In Spain, in the EPIRCE3 study it was estimated that approximately 10 % of the adult population had some degree of chronic renal impairment, a 6.8 % had CKD stages 3–5, although there were significant differences with the age (3.3 % between 40–64 years and 21.4 % for older than 64 years), and a 0.3 % of have advanced CKD (CKD stages 4 and 5 or ACKD). In the ACKD outpatient clinic, a multidisciplinary team initiates a process of information and training of the patient and family environment, with the purpose of involving them in the disease and in the choice of the different options of renal replacement therapy (RRT) available or conservative treatment (CT). The idea is to improve the health status of patients, delay the onset of RRT, and once it is necessary the choice of modality of RRT which is the best for the patient and his environment.
The evaluation of the quality of care of these patients may be measured by the results in health. The implementation of a common, standardized structured process for decision-making in relation to the choice of RRT or CT will allow the evaluation and comparison of the results between different groups and, in addition it pursues the compliance with Law 41/2 002 of 14 November 2002,4 regarding the rights and values of patients. As a result, it is expected to achieve a better adaptation of the treatment to the patient, a better development of their disease, a reduction of patients with unscheduled start of dialysis and its consequences, as well as a better preparation of the environment and the patient for transplantation, home treatments or for the choice of CT.5–7
There are several studies published, some of them conducted in our country, prospective and with a high number of patients,8 showing the influence of the information they receive on the choice of the RRT modality, however morbidity and mortality and evolution have not been considered. The present work, analyzes the baseline characteristics of the incident patients in the ACKD outpatient clinic, the result of applying a tool that includes standardized structured information for the choice of the type of TRS/CT and its evolution in one year (initiation of TRS, hospital admissions and mortality).
MethodThe present study is observational, prospective, multicenter, in 3 Spanish hospitals (2 in Andalusia and one in the Canary Islands, serving a population of 1,400,000, 600,000 and 600,000 inhabitants, respectively). All patients ≥18 years of age that start care in the ACKD outpatient clinic (eGFR <30ml/min/1.73m2) during inclusion period and who signed the informed consent (these are the only inclusion criteria) were included. Inclusion period: from June 1, 2014 to October 1, 2015. Observation period of 12 months or until the beginning of the RRT or death, if they occur before 12 months. The study was completed on October 1, 2016. In all cases standardized laboratory methods were used for the determination of creatinine (Cr) (Jaffé method compensated in 2 hospitals and enzymatic method in a third hospital) and eGFR was estimated according to the CKD-EPI equation. Demographic data and comorbidity were also recorded according to Charlson's index (with and without age). In the case of patients who received structured information (educational process: EP, it were collected the dates at starting and ending the EP, the decision adopted and the eGFR in that date. In the case of patients who initiated RRT (home and in center hemodialysis [HD], peritoneal dialysis [PD], transplant), it was collected the date of initiation, the eGFR at the time of initiation, vascular or peritoneal access and the context (scheduled or urgent initiation, as the one that motivates hospital admission or urgent care for its initiation by an unpredictable intercurrent process). Logically, the date and the initial eGFR were not considered in the case of patients choosing CT. It was also recorded the evolution during the first 12 months after the first visit to the ERCA clinic including hospital admissions and death with dates and causes.
The EP carried out has been described in detail in previous publications.8 In summary, the objective is to provide information and help to the patient to identify his personal values and preferences to facilitating the choice. This process is performed by trained nursing staff, in 4 sequential phases, in a visits of 30–60min. In the first one, the preferences and the scale of values of the patient are identified, in the second, the patient and his relatives are informed of the different options of RRT in the center and at home, CT and transplant. After this phase, the patient takes with him a variety of material on digital media or paper to complete the information; in the third phase, the patient consults with the personnel that carries out the EP the doubts generated after the information received and commented with his relatives at home; in the fourth phase the patient makes a decision. According to the protocol, all patients of the ACKD outpatient clinic would receive the EP throughout their follow-up, being at the discretion of the responsible nephrologist the time chosen to give the EP (clinical circumstances or eGFR).
The statistical analysis was performed with the statistical package SPSS 22 (IBM, Chicago, Illinois). Quantitative variables are expressed as median and interquartile range, since they did not follow a normal distribution. For independent samples, non-parametric statistical tests (Mann-Whitney) were performed. Kruskal-Wallis was used in the case of variables with more than 2 categories. Wilcoxon test for related samples. The chi-square test was used for analysis of the contingency tables, as well as for the comparison of proportions or frequency distributions. The Spearman coefficient has been obtained to study the correlation between two continuous variables.
It was analyzed which variables independently influenced the probability of death through Cox regression analysis, considering death as event and time to the event the time elapsed since the first visit to the date of death. Independent variables: age and Charlson index without age, sex, diabetes and admissions. All non-deceased patients were considered as censored and the time is the maximum time elapsed between the date of the first visit and the date of the study completion visit or the date of the visit at 12 months, the end of the observation period.
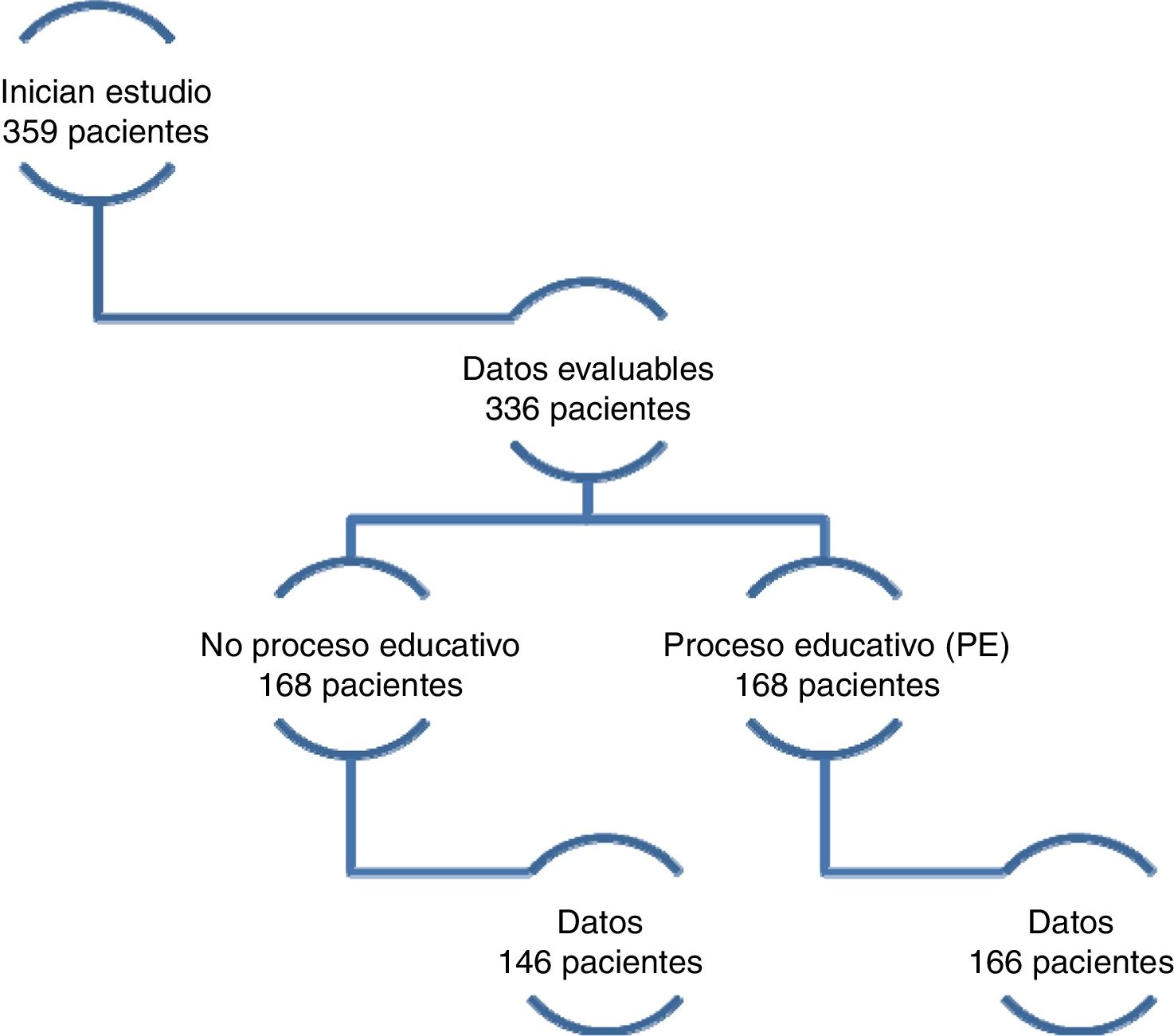
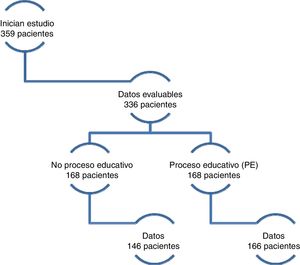
ResultsClinical characteristics (baseline)From June 1, 2014 to October 1, 2015, 359 patients start follow up in the ACKD outpatient clinic and signed the informed consent, 16 other patients refused to participate and did not sign the consent. There were 23 that were not included because of deficiency in the identification data, remaining 336 evaluable patients (60 % male) with a median age of 71.5 (17) years (55 % of patients were 70 years or older). Of the patients who received EP (168 patients), there was data of the evolution throughout the observational period in166 patients. From the 168 who did not receive EP, we had the evolution data in 146; so the total number of patients was 312 (Fig. 1).
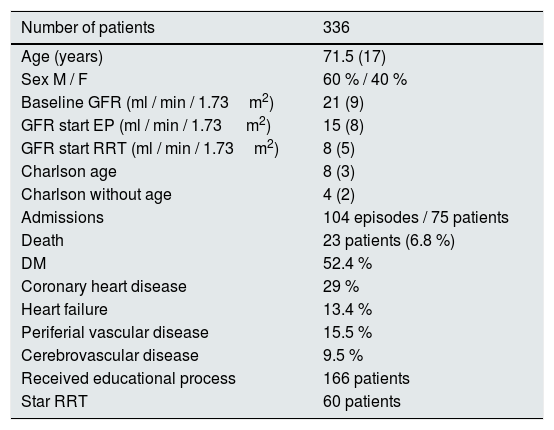
The most frequent cause of CKD was vascular nephropathy (35 %) and diabetic nephropathy (32 %). 86.4 % of patients were referred to ACKD from the General Nephrology outpatient clinic. Other patients were referred from the Nephrology Service after hospital discharge: 1.8 %; from the outpatient clinic of another specialty (Internal Medicine): 5.4 %; after hospital discharge from a specialties other than Nephrology: 4.5 %, from Primary Care: 1.5 %, unknown origin 0,4%. The baseline eGFR was 21 (9)ml/min/1.73m2, at the beginning of the EP was 15 (9)ml/min/1.73m2. The Charlson index with age: median 8 (3), without age: median 4 (2). Only 7 patients had previously received RRT (had recovered of renal function, none due to previous renal transplantation). Table 1 summarizes the baseline characteristics of patients.
Baseline characteristics of the patients.
| Number of patients | 336 |
|---|---|
| Age (years) | 71.5 (17) |
| Sex M / F | 60 % / 40 % |
| Baseline GFR (ml / min / 1.73m2) | 21 (9) |
| GFR start EP (ml / min / 1.73 m2) | 15 (8) |
| GFR start RRT (ml / min / 1.73m2) | 8 (5) |
| Charlson age | 8 (3) |
| Charlson without age | 4 (2) |
| Admissions | 104 episodes / 75 patients |
| Death | 23 patients (6.8 %) |
| DM | 52.4 % |
| Coronary heart disease | 29 % |
| Heart failure | 13.4 % |
| Periferial vascular disease | 15.5 % |
| Cerebrovascular disease | 9.5 % |
| Received educational process | 166 patients |
| Star RRT | 60 patients |
EP: educational process; RRT: renal replacement therapy.
Quantitative variables are expressed as median and interquartile range.
A 54 % of the patients were diagnosed with diabetes mellitus (DM). When comparing with the group of patients without DM, the following stand out: age 72 (14) vs. 70 (21) years (p=0.03) and Charlson greater than non-diabetics: Charlson without age: 5 (2) vs. 3 (2), p<0.001, and with age: 8 (3) vs. 6 (3), p<0.001, eGFR at the beginning of the EP: 17 (9) vs. 14 (7)ml/min/1.73m2, p=0.04; no differences in baseline eGFR, hospital admissions or death. An initial choice of CT was more frequent in patients with DM: 51 % vs. 42 % (p=0.01).
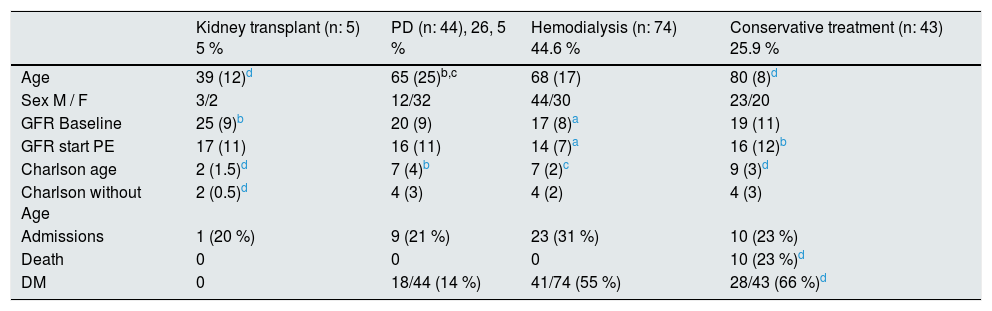
Educational processAs mentioned, throughout the year of follow-up the EP was performed in 50 % of the patients (data available for 166 patients), the time elapsed to make a decision was 3 (5) months. The eGFR at the beginning of this process was 15 (9)ml/min/1.73m2. The initial treatment chosen by the patients was as follows: PD 44 patients (26 % of the total corresponding to 37 % of the patients who decide RRT), HD 74 patients (44 % of the total, reaching 63 % of those who decide RRT), CT 43 patients (26 %) and living donor renal transplant: 5 patients (3 %). In some comparisons the transplant was not included due to the small number of patients. In all cases, the choice of HD was in the center and in none of the patients decided home HD.
It should be noted that the patients who choose CT are older (p<0.05), with higher Charlson index (p<0.05) and higher eGFR at baseline and at the beginning of EP along with those choosing PD (p<0.05 as compared with those who choose HD). Among the patients with at least one hospital admission throughout the follow-up (a 26 % of the total), there were no differences in the choice of treatment. A 6 % (10 of the 166 subjects) of the patients who received EP died, all had chosen CT. Table 2 describes the profile of the patients choosing each of the options of RRT and their evolution.
Characteristics of the patients according to the initial option after the educational process (n=166).
| Kidney transplant (n: 5) 5 % | PD (n: 44), 26, 5 % | Hemodialysis (n: 74) 44.6 % | Conservative treatment (n: 43) 25.9 % | |
|---|---|---|---|---|
| Age | 39 (12)d | 65 (25)b,c | 68 (17) | 80 (8)d |
| Sex M / F | 3/2 | 12/32 | 44/30 | 23/20 |
| GFR Baseline | 25 (9)b | 20 (9) | 17 (8)a | 19 (11) |
| GFR start PE | 17 (11) | 16 (11) | 14 (7)a | 16 (12)b |
| Charlson age | 2 (1.5)d | 7 (4)b | 7 (2)c | 9 (3)d |
| Charlson without Age | 2 (0.5)d | 4 (3) | 4 (2) | 4 (3) |
| Admissions | 1 (20 %) | 9 (21 %) | 23 (31 %) | 10 (23 %) |
| Death | 0 | 0 | 0 | 10 (23 %)d |
| DM | 0 | 18/44 (14 %) | 41/74 (55 %) | 28/43 (66 %)d |
Quantitative variables expressed as median and interquartile range.
A comparison of patients that receive EP with those that did not receive it showed significant differences in baseline eGFR, being higher in patients who did not receive PE: 24 (7) vs. 18 (8)ml/min/1.73m2 (p<0.001); there significantly older those who did not receive PE: 72 (14) vs. 70 (3) years (p: 0.03), and there were no differences in the Charlson index with and without age, gender and DM.
Evolution (initiation of renal replacement therapy, hospital admissions and mortality)Initiation of renal replacement therapyAs mentioned in the methods section, data on the evolution at one year are available in 312 patients (out of the initial 336 patients), which are those evaluated in this section. Throughout the follow-up, 60 patients started RRT. All had received EP, with the exception of 3 of them, the distribution being: 2 patients (3.3 %) had preemptive renal transplant (both from living donor); 18 patients in PD (30 %); 40 patients receiving HD (66.6 %), all of them in HD center, no one home HD. The eGFR at the beginning of the treatment (as mentioned in the methods section, CT is not included) was 8.5 (5)ml/min/1.73m2. Divided according to the type of dialysis and vascular access: peritoneal catheter (n=18) 12 (5)ml/min/1.73m2; internal vascular access (n: 17) 8 (5)ml/min/1.73m2 ; Permanent vascular catheter (n: 11): 9 (3)ml/min/1.73m2, and transient vascular catheter (n: 12): 8 (3)ml/min/1.73m2. The differences were not statistically significant.
Out of 12 patients who start HD with transient vascular catheter, 11 of them had an emergency HD during hospital admission due to heart failure; in the remaining patient the cause is not shown ; 9 of the 12 had received the EP: 7 had chosen HD, one DP, one CT. The profile of these patients who start HD with transient vascular catheter is: Charlson 8 (3), without age 5 (3), age 73 (21) years, and a eGFR at the beginning of HD: 8 (3)ml/min/1, 73m2, baseline GFR 19 (10)ml/min/1.73m2. Period of follow-up in outpatient clinic: 12 months in one patient, and a median of 3 (4) months in the other 11 cases.
Out of the 60 patients, 9 (15 %) changed in relation to the initial choice: 6 changed from PD to HD (one of them during admission because they needed urgent dialysis), 2 patients that chose renal transplantation changed to PD when it was not possible the live donation initially planned and one of the patients who initially preferred CT finally started HD.
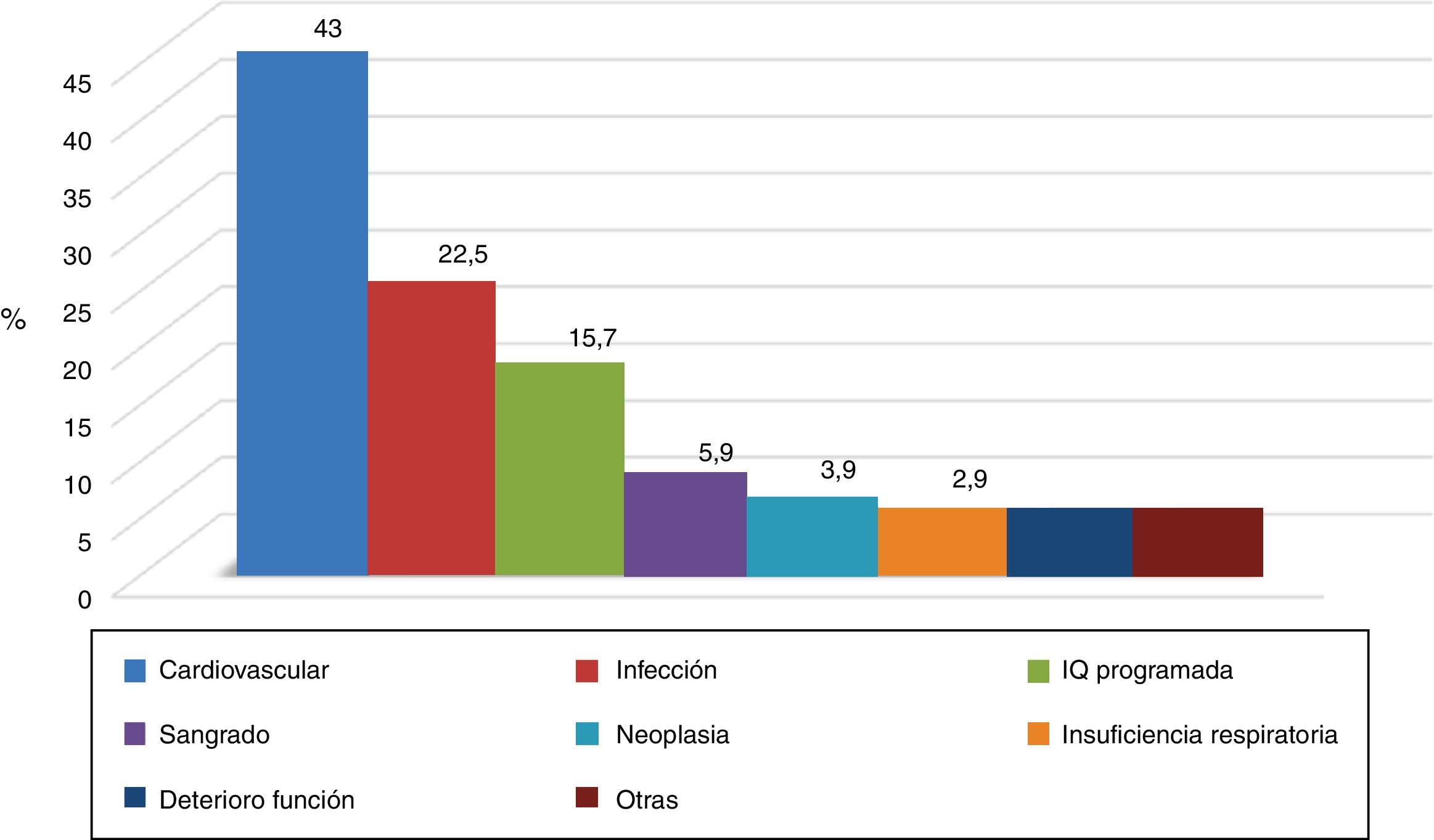
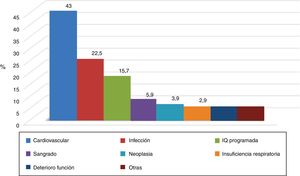
Hospital admissionsDuring the observation period, 104 hospital admissions (data available for 102 episodes) were recorded in 73 patients (23.5 % of the 312 group). The causes of admission are shown in Fig. 2, with the most frequent cardiovascular disease: 44 (43 %), followed by infection: 23 episodes (22.5 %). In 36 of the 102 episodes (35 %) of which we have data, heart failure was recorded in the discharge or death report as a cause of admission or arising throughout it. When analyzing the profile of the patient admitted, we found statistical significance in the variables: Charlson index with age: 7 (3) vs. 8 (3) admitted (p: 0.01), and without age 4 (3) vs. 4 (2) admitted (p: 0.02); no differences in baseline GFR, age, sex or DM.
Mortality6.8 % (23 patients) of the patients died during the follow-up period, time in ACKD outpatient clinic until the death 9 (10) months. In 14 cases the death was in the hospital, in 7 cases at home and in 2 cases this information was not available. The causes could be determined in 18 cases: 7 patients for cardiovascular disease (39 %), 4 patients for cancer (22 %), 3 patients for CKD with CT (1 7 %), 2 patients for infection (11 %), one due to liver disease (5.5 %) and an accidental event in one (5.5 %).
In deceased patients, the age was 80 (10) vs. 71 (17) years (p<0.001), with higher Charlson index with age (9 (4) vs. 7 (3) (p<0.001)) and without age (6 (5) vs. 4 (2) (p: 0.006)). There were no differences in mortality regarding gender and eGFR at the beginning of follow-up or EP. All deceased patients who had received structured information had chosen CT. A 60,9 % of the deceased patients had at least one hospital admission as compared to a 39 % of the non-deceased patients (p<0.001).
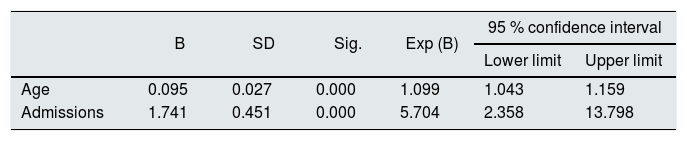
The Cox regression analysis of the predictive variables of death showed that for each additional year of the age in the moment of the first ACKD outpatient clinic visit, the probability of death increases by 1.099 (CI: 1.04 to 1, 16). Likewise, hospital admissions increases the probability of dying 5.7 times (CI: 2.36–13.80) (Table 3).
Cox Regression Analysis : Age.
| B | SD | Sig. | Exp (B) | 95 % confidence interval | ||
|---|---|---|---|---|---|---|
| Lower limit | Upper limit | |||||
| Age | 0.095 | 0.027 | 0.000 | 1.099 | 1.043 | 1.159 |
| Admissions | 1.741 | 0.451 | 0.000 | 5.704 | 2.358 | 13.798 |
Analysis of the variables involved in mortality. Resulting Model. Sex, Charlson index without age and diabetes have been discarded.
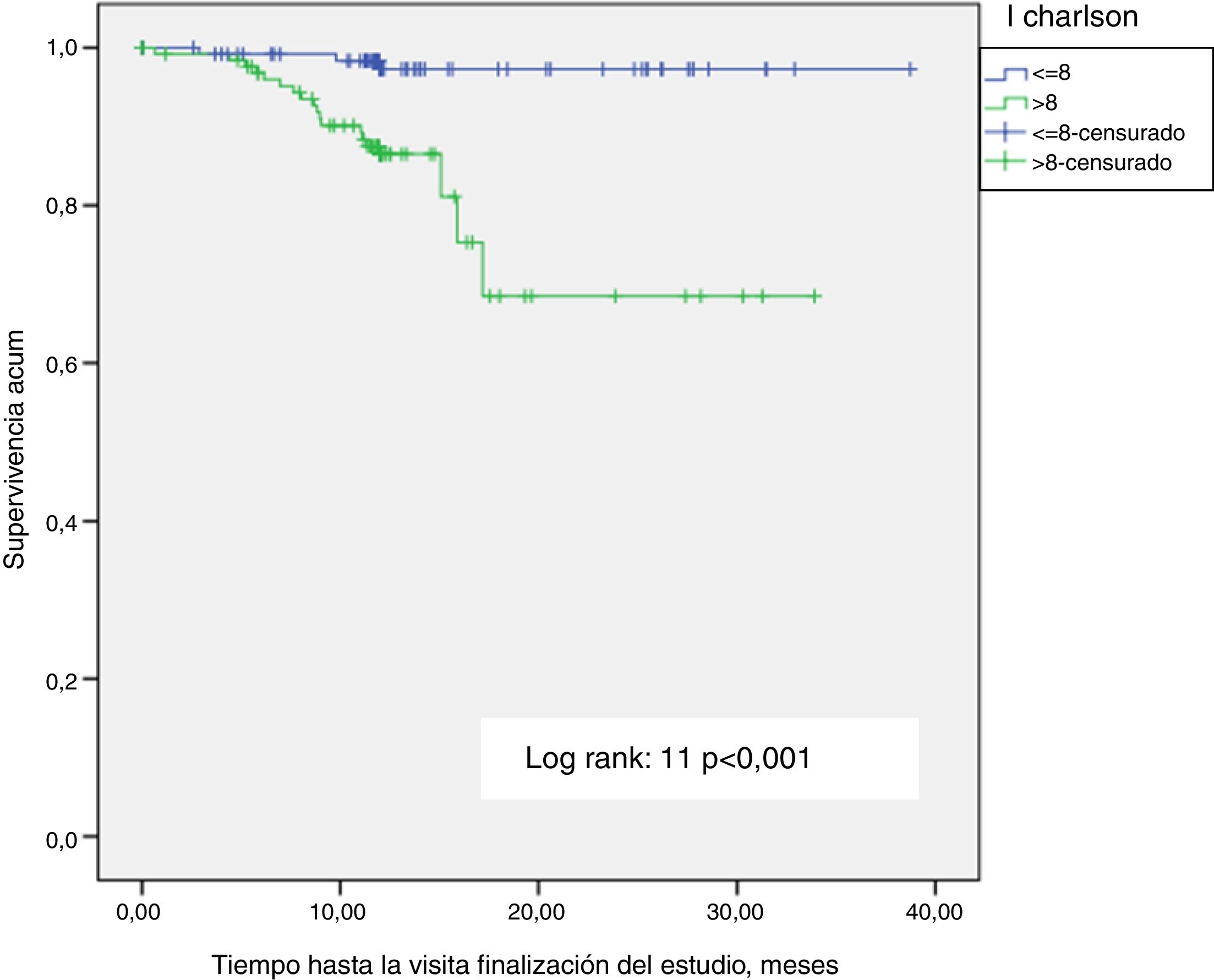
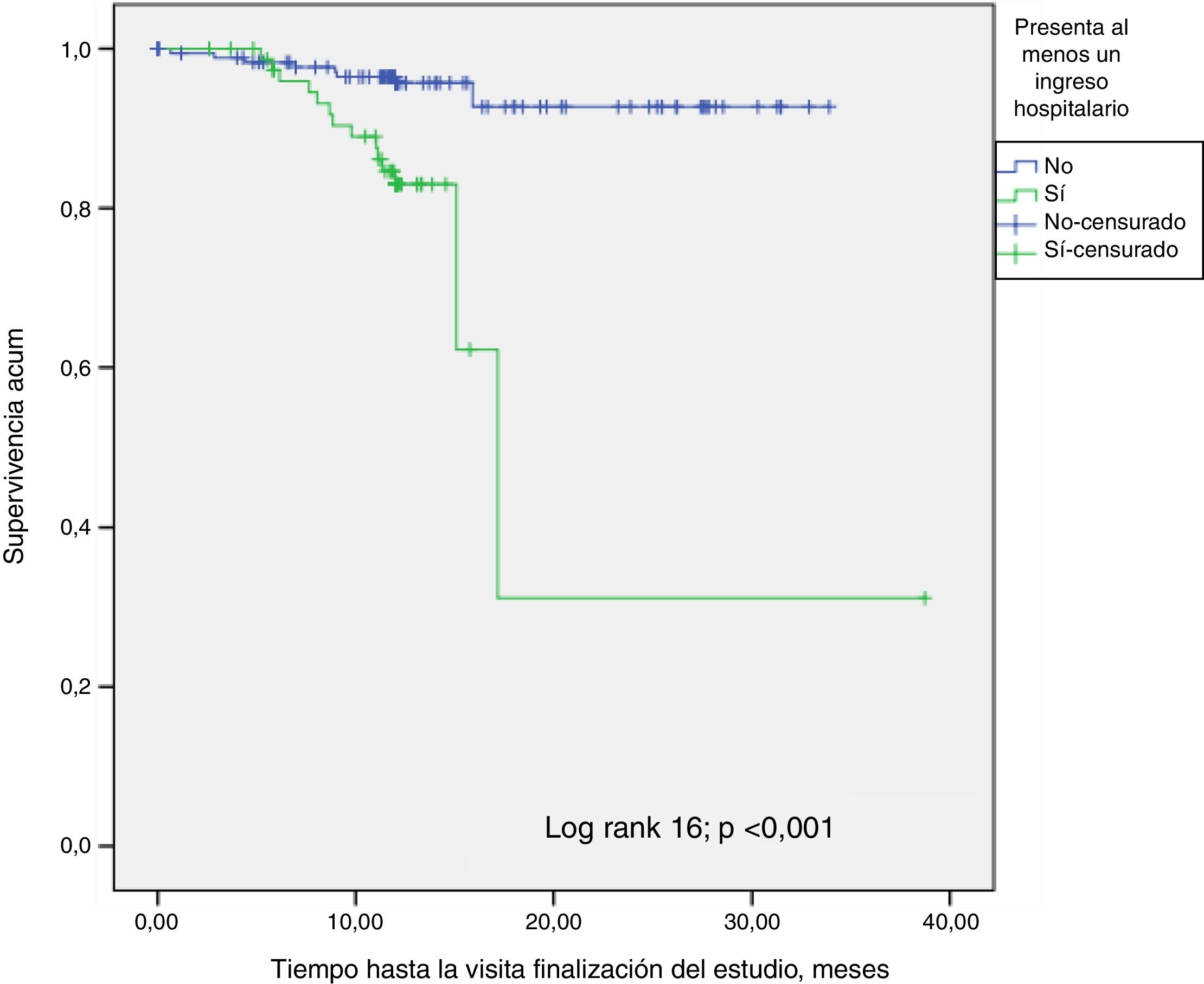
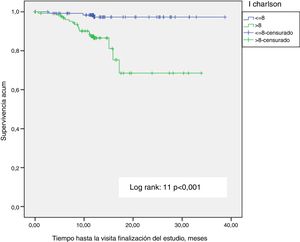
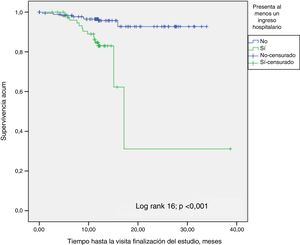
A Kaplan-Meier survival analysis was performed to determine the effect of the Charlson index with age greater or lower than the the median (8) (p<0.001) (Fig. 3). Significance is lost (p=0.1) performing the analysis with the Charlson index without age (4). The influence of hospital admission on survival was also analyzed (Fig. 4); patients who had at least one admission were compared with those without admissions (p<0.001), the results were consistent with the Cox regression analysis. There were no survival differences in diabetic patients.
DiscussionIn the present study, we have observed that the population of patients attended in the ACKD clinics of the participating centers is aged (more than half of the patients are 70 years or older at the beginning of the follow-up) with comorbidities and with a high. Rate of hospital admissions that, together with age, determine mortality. It is also appreciated that a high proportion of patients chose PD and CT after the EP.
The distribution of the different modalities of RRT or CT varies between countries and is often influenced by non-medical factors (economic incentives, availability of resources, bias of the health staff that directs the patient, availability of support structure for CT, etc.). Pre-dialysis education programs, such as the one applied in this study, are based on individualized information sessions explained by trained personnel of the nurses staff to the patient and family, with the support of audiovisual material to take home, with the intention of reducing anxiety and promote the modalities of self-care. For years it has been known that patients receive structured information about RRT different modality options8–10 chose home dialysis more frecuently.
Although the most frequent type of RRT is in center HD, home techniques, such as PD and home HD, technically are equally valid treatment options for the patient's clinical evolution and satisfaction11,12 and are viable or feasible in 80 % of patients with CKD.13 In addition, these techniques are less expensive (not requiring periodic displacements to the dialysis center), which is increasingly important becausethe life expectancy and CKD patients number is increasing.
Our study shows that there is a high proportion of patients who choose PD, both initially at the time of receiving EP (25 %), and when they initiate RRT (30 %). These percentages of the PD as a starting technique are well above percentages of national average and of the regional autonomous communities to which the patients belong, Andalusia and the Canary Islands. According to the dialysis and transplantation report of the 2016 Regional Registries14 the percent of PD patients is: 16.7 % (Spain), 12.6 % (Andalusia) and 20 % (Canary Islands). In a study conducted by Prieto-Velasco et al.8 in our country, using the same education tool, the proportion of patients who chose PD rose to 45 %, a value similar to those who chose HD. This technique of RRT is currently considered the most favorable option of initiate RRT in various studies. In a recent work, performed in Canada with patients on RRT who had received pre-dialysis education, the modality PD shows greater or similar survival than HD at a lower cost of PD.11 Likewise, in a study of the Andalucía Goverment based on the data from the SICATA registry (Regional Autonomous Registry of patients with CKD) (on preparation for publication) describes the more favorable itinerary for the ESRD patient, assuming that patients goes from one type of dialysis to another (preemptive transplant was not considered). The most favorable for patient survival, and at the same time the least expensive, was initiation on PD followed by HD after a period of 3–5 years (coinciding with the loss of residual renal function).15
The profile of the patient who chooses PD compared with the one who chooses HD, is tends to be younger with a high proportion of men, lower number of hospital admissions and less prevalence of DM, however prevalence of DM is the only value that shows statistical significance. This profile would be in accordance with that described in other studies,8,9 in which it seems that younger patients with less morbidity associated with DM choose PD because they are more motivated than HD patients to take care of them self and they want less dependence on schedules and less displacements.
An important aspect of receiving complete information before reaching terminal CKD stage is to allow the patient to contemplate the CT as an option. This has to be weighed and discussed with their relatives and with the healthcare staff. As observed in this study, this option was chosen by 25 % of patients who received EP throughout the follow-up. In the work carried out in Spain and previously referred,8 the proportion of patients choosing CT after receiving EP was much lower (8 %). This difference may be explained by the higher age (67 vs. 71.5) and the high morbidity (not found in the referred study) observed in our study. Although it is difficult to predict which patients will not evolve favorably in dialysis,16 the experience supported by several studies suggests that dialysis does not always entail benefits in patients with high morbidity and, sometimes, it does not extend survival; this was shown in a recent study by our group.17 However, this decision is often difficult, given the absence of generalized criteria and guidelines. Given the importance of individualization in the final decision of the patient and his environment, it seems important to inform with time and in non-pressing circumstances (hospital admission, emergencies, etc.) of this alternative. Despite this, this option is not always contemplated due to various circumstances, depending more on the environment than on the patient. In a recent publication18 the opinion of several nephrologists was analyzed and various factors were identified, such as the lack of infrastructure for the follow-up and treatment of these patients, the economic incentives for dialysis and even the poor preparation of the nephrologist during education of both medical license and specialty training, to deal with patients with issues related to death. In an excellent review of the onset and withdrawal of dialysis,19 it is added that for both the nephrologist and family it may be easier to start dialysis than to propose and follow CT, at times, possibly this may not be the most favorable decision for the patient himself and his quality of life.
A recognized and unresolved problem10 is the best moment and with what eGFR to inform the patient on the various options of RRT or CT. In our study, the median eGFR was 15 (9)ml/min/1.73m2, similar to the study by Prieto-Velasco et al.,8 which seems more reasonable than the 30ml/min/1.73m2, postulated in other studies reasoning that anticipating the situation of stage 5 facilitates the choice of home treatment.20,21 In contrast to the previous approach, it could be argued that a very early decision makes it more likely to be changed, furthermore, given the characteristics of our patients (age and high comorbidity) a large proportion may die before requiring TRS. Thus, in a recent meta-analysis of 28 studies (more than 185,000 patients) with CKD 4–5 that analyzed how traditional risk factors affect the evolution of these patients: They found that cardiovascular events and death were 2 and 4 times more frequent, respectively, than the evolution toended CKD or start on dialysis.22
The comorbidity and age of the patients included in the present study were high, with a high percentage of diabetics, more than 50 %, and more than half of the patients with 70 years or more. As a result, the number of hospital admission was high. In this aspect 2 facts should be highlighted: the high incidence of vascular disease, particularly heart failure, as a cause of admission and the influence of hospital admissions and probably heart failure itself in mortality, to the point of multiplying by almost 6 times the probability of death according to the Cox correlation analysis. A very recent study, which analyzes how to improve the survival of patients with ACKD, emphasizes the high risk and prevalence of heart failure in these patients, especially the heart failure with preserved ejection fraction.23
Another striking fact is the high incidence of patients who initiate HD with transient catheter (12 of the 40 patients, 30%). Except for one of them, they had been followed for less than 3 months in the ACKD clinic and the initiation of HD occurred during admission and in the context of urgent HD. So, this is an unplanned initiation of RRT. This percentage is similar to the average of Andalusia in 2016, 28 %,24 and is lower than in other studies performed in our country that show a 45 %8 and the rate in another countries has been reported to be 5411 and 33 %.25 This should invite us to anticipate the preparation for the initation of RRT in certain patients predisposed to these complications because to avoid the insertion of a transient catheter is important due to its effect on infections and mortality.
The consistency of the study is based on the fact that it is prospective, which favors the veracity and adequacy of the data collected to achieve the objectives, the high number of participants, the uniformity of the information received for the choice of RRT and CT and the scarcity of similar studies. As negative points it could be considered the observation time of one year, with a number of events (patients starting RRT) less than expected and that would have been greater in a longer period of study. Likewise, neither the level of education nor the economic/social status were collected, both important at the time of making a decision regarding the RRT or TC. The absence of protocolized criteria for imparting EP and with what eGFR should not be considered as negative, since it allows to know the clinical practice in a subject that is controversial and is not resolved at the moment.
We can conclude that as can be perceived from the results of this study, that the specialized care of the population of patients with ACKD, of elevated comorbidity, has an important impact on the evolution of the disease and choice of type of RRT. Therefore, the resources available must be facilitated to the demanding population. To corroborate these findings we need studies with longer period of follow-up.
SponsorshipThe study has been promoted and funded by the company Baxter SL.
Conflict of interestsThe authors declare no conflict of interest.
Please cite this article as: Guerrero Riscos MA et al. Estudio ERCA. Características basales, evaluación de la aplicación de la información estructurada para la elección de tratamiento renal sustitutivo y evolución a un año de los pacientes incidentes en la consulta ERCA. Nefrologia. 2019;39:629–637.
Study on Advanced chronic kidney disease (ACKD). Baseline characteristics, evaluation of the application of the structured information for the election of renal replacement therapy and one-year follow-up of incident patients in the ACKD outpatient clinic