To the Editor,
It was classically accepted that vancomycin excretion through low permeability membranes during conventional haemodialysis (HD) was negligible (less than 5%). With high permeability membranes this has changed, which has important effects when treating vancomycin overdose. We report a case of acute oliguric renal failure secondary to vancomycin overdose resolved by the use of standard HD with high-permeability membranes.
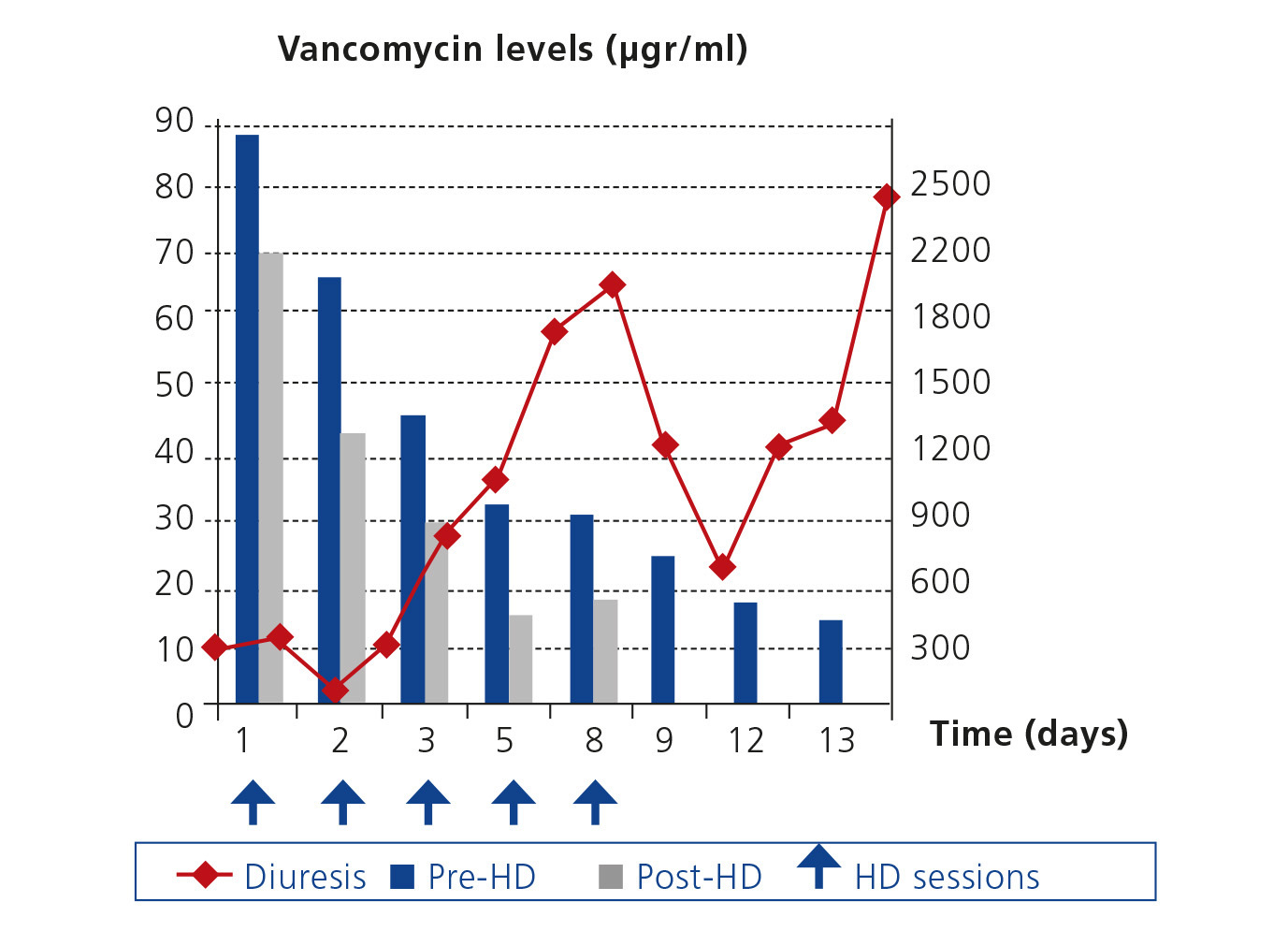
An 83-year-old male with high blood pressure, type 2 diabetes mellitus, who had suffered a myocardial infarction 10 years before and with cognitive impairment due to Alzheimer's disease, was admitted with aspirative pneumonia. He was treated with amlodipine, metformin, aspirin, repaglinide and risperidone. On arrival he was suffering from moderate prerenal kidney failure (plasma creatinine [Cr]: 1.7mg/dl, estimated glomerular filtration rate calculated by the MDRD-4 formula [eGFR]: 40ml/min/1.73m2), which after being corrected stabilized (Cr: 0.95mg/dl, eGFR 80ml/min/1.73m2), with elemental anodyne urine. He was treated with furosemide piperacillin and tazobactam. Due to a poor prognosis, intravenous vancomycin was added on the fifth day at 0.5g/12 hours (13mg/kg/day). Between the tenth and twelfth day urine volume decreased (200-400ml/day) and Cr 6.3mg/dl (eGFR: 9 ml/min/1.73m2) and elemental urine were seen suggestive of acute tubular necrosis (ATN). Doppler Ultrasound: preserved kidney size with no hydronephrosis with preserved intrarenal vasculature. Immunology and viral serology were negative. In 48 hours, Cr rose to 8.4mg/dl (eGFR: 6.5ml/min/1.73m2). General condition worsened, with mild fever disorientation, drowsiness, dysarthria, and slight fever. Vancomycin levels (last dose 48 hours before): 87.7µg/ml. No eosinophilia, eosinophiluria, skin or joint symptoms. The general condition of the patient was not appropriate for renal biopsy and the patient was diagnosed with acute kidney injury network (AKIN) III due to acute tubular necrosis secondary to vancomycin overdose. Acute HD was performed with a high permeability polyamide membrane (poliflux 21 H, Gambro®) 2.1m2 surface, 50 microns thickness and ultrafiltration coefficient (KUF) 85ml/hx mmHg for 4 hours, with a blood flow of 350 ml/min and 800ml/min. Following the session, vancomycin levels went down to 69.9µg/ml, due to an elimination of 20.3% and t½ of 12.6 hours. Two hours later, levels remained stable (65.5µg/ml). After a second session 24 hours later using an on line technique levels were at 41.6mg/ml (percentage of reduction: 40.48% and t½: 6.13 hours). Three sessions of standard HD were performed with reduction percentages between 30-56% (Figure 1). Significant rebound was only seen between the fourth and fifth session, separated by 72 hours. The patient’s general condition gradually improved, fever disappeared and he recovered neurologically. During the following days, urine output increased progressively.
DISCUSSION
Vancomycin has a half-life of 4-6 hours (54-180 hours in terminal renal failure1), 55% protein binding and 1500 Da molecular weight. It is eliminated by glomerular filtration. There are two causes of acute renal failure due to vancomycin acute interstitial nephritis (AIN) and ATN due to direct toxicity on proximal convoluted tubules (PCT)2 due to impurities related to its synthesis ("Mississippi mud"). Most cases present aggravating factors3: concomitant treatment with aminoglycosides or diuretics, treatment during more than 21 days, high APACHE score (Acute Physiology and Chronic Health Evaluation), obesity, trough concentration> 28µg/ml and doses >4g/day. Cuprophane and cellulose triacetate membranes do not eliminate substances with a molecular weight >500Da, so that the decrease in concentration using these membranes is considered negligible. High permeability membranes have increased removal to 50%4,5. The most efficient techniques are thought to be charcoal haemoperfusion, haemodiafiltration and high permeability standard HD, without greater effectivity of any having been clearly demonstrated.
Using biopsy diagnosis, we found 11 cases of acute renal failure: 63% had acute interstitial nephritis (AIN) and 45% acute tubular nephritis (ATN)6-10, and 4 cases that did not undergo biopsy, required high permeability HD or charcoal haemoperfusion. Patient ages ranged from 8 to 79, vancomycin doses from 1-2g/day, 40-60mg/kg/day, during 2-7 days in cases of ATN and 2-30 days in cases of AIN, with trough levels between 45.8 to 420µg/l. 92.8% of ATN cases recovered the baseline GFR despite needing acute HD. In all cases, high permeability membranes were used that achieved reductions of 50-73%.
In our case, the patient required five sessions. In the first, purification efficiency was mild (20.23%); in the second, on line, it was significantly higher (40.48%), and during the others vancomycin concentration reduction ranged from 30-56%. Clinical, neurological and renal function evolution were satisfactory, with recovery of volume of diuresis and GFR in two weeks. In view of this case, we conclude that standard HD with highly permeable membranes is an effective treatment for acute renal failure caused by secondary ATN due to vancomycin overdose.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Figure 1. Evolution of vancomycin levels and diuresis.