Peritoneal dialysis is a type of renal replacement therapy that uses the physical and chemical properties of the peritoneal membrane to perform ultrafiltration and clearance processes.1–3 One complication of this procedure is peritonitis,4,5 which is diagnosed with the presence of at least two out of the three following criteria: a leukocyte count higher than 100mm−3, a corresponding clinical picture and microorganisms on a Gram stain.4,5
The International Society for Peritoneal Dialysis recommends management with first-generation cephalosporins for Gram-positive microorganisms and third-generation cephalosporins for Gram-negative microorganisms.6
It also recommends starting treatment with third-generation cephalosporins (ceftazidime) and first-generation cephalosporins (cefalotin) by the intraperitoneal route, with permeation doses of one gram and maintenance doses of 250mg every 6h; however, the response is uncertain.7
Against this background, the aim of this study was to compare the efficacy of the permeation regime and the maintenance regime in patients with peritonitis due to dialysis.
A cohort study was conducted in patients with end-stage renal disease and peritonitis. The exposure group included patients treated with a permeation regimen (one gram of ceftazidime/cefalotin q 24h); the unexposed group included patients with a maintenance regimen (one gram initially and 250mg of ceftazidime/cefalotin q 6h thereafter).
Patients with a diagnosis made by cell count were included; patients with refractory peritonitis, recurrent peritonitis or cephalosporin allergy were excluded.
The sample (31 per group) was calculated using a percentage formula for 2 populations, assuming that the efficacy of ceftazidime/cefalotin was 60% in the permeation group and 35% in the maintenance group.
Their sociodemographic characteristics, concomitant diseases, modality of dialysis, time on peritoneal dialysis and time of progression of chronic kidney disease were studied.
Therapeutic efficacy was established through cell counts, using 99 cells per field as a cut-off point, evaluated at 24, 48, 72 and 96h.
Analysis included percentages, averages, standard deviations, Student's t-test for independent populations and the chi-squared test.
Age and gender were similar in the permeation group and the maintenance group: 48.06±17.79 years and 55.07±12.64 years (p=0.84); male gender with 65.6% and 62.1%, respectively (p=0.77). In these groups the prevalence of hypertension (p=1.00), diabetes mellitus (p=0.62) and drug immunosuppression (p=0.35) were similar.
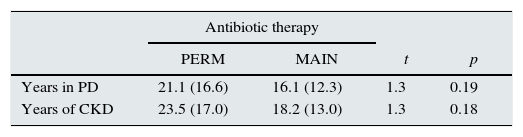
In both groups there was a predominance of continuous ambulatory peritoneal dialysis (59.4% and 69.0%, respectively; p=0.51). Time in dialysis (p=0.19) and time of progression of chronic kidney disease (p=0.18) were similar in the groups (Table 1).
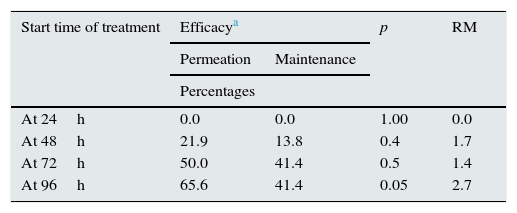
Seventy two hours after initiation of therapy, efficacy was 50.0% in the permeation group and 41.4% in the maintenance group; however, they were not statistically different (p=0.50). At 96h, a statistical difference was found: in the permeation modality 65.6% showed efficacy and in the maintenance modality 41.4% showed efficacy (p=0.05) (Table 2).
Efficacy of permeation and maintenance by start time of treatment in peritonitis.
| Start time of treatment | Efficacya | p | RM | |
|---|---|---|---|---|
| Permeation | Maintenance | |||
| Percentages | ||||
| At 24h | 0.0 | 0.0 | 1.00 | 0.0 |
| At 48h | 21.9 | 13.8 | 0.4 | 1.7 |
| At 72h | 50.0 | 41.4 | 0.5 | 1.4 |
| At 96h | 65.6 | 41.4 | 0.05 | 2.7 |
In the management of bacterial peritonitis associated with dialysis, the antimicrobial regimens and dosage regimens proposed in clinical practice guidelines have shown to produce ineffective results, hence the importance of this study analysing the prolonged stay of the antibiotic in the abdominal cavity and the decrease in the manipulation of the peritoneal cavity.8
It was ensured that the 2 groups were statistically similar with respect to disease history, type of dialysis, time of progression of chronic kidney disease and time in dialysis as these were significant benchmarks that made comparison between the different management regimens more reliable.
Similarly, the same antibiotic was used in the 2 groups as this made it possible to be certain that what was being compared was the number of drug administrations (one administration vs 4 administrations). The pathophysiological substrate was the drug's cumulative capacity in the peritoneum and its half-life, as well as the peritoneum's lower exposure to the introduction of microorganisms in each drug administration. To date, this matter has not received enough attention.8,9
Cephalosporins are first-line antibiotics in the treatment of peritonitis in dialysis: as they are administered by the intraperitoneal route, they penetrate the tissue wall and achieve a half-life of 48–72h. However, it will be necessary to clarify whether the efficacy achieved in the permeation regimen is due to the fact of exposing the peritoneum to a high dose of antibiotic, or to the fact of decreasing the events that penetrate the peritoneal cavity and therefore the potential for keeping from introducing germs into the cavity.6
In conclusion, the permeation regimen has a greater efficacy than the maintenance regimen in the management of peritonitis secondary to peritoneal dialysis.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Carranza-Torres JM, Vargas-Daza ER, Villarreal-Ríos E, Galicia-Rodríguez L, Martínez-González L. Eficacia del esquema de impregnación vs. esquema de mantenimiento con ceftazidima/cefalotina en pacientes con peritonitis por diálisis. Nefrologia. 2016;36:448–450.