To the Editor:
Drug hypersensitivity syndrome or DRESS syndrome is a rare but potentially severe condition characterised by ailing skin, eosinophilia and systemic involvement.1
We present the case of a 74-year-old female, with a medical history of hypertension, atrial fibrillation, right eye glaucoma and basal cell carcinoma of the nose removed. The patient is admitted in the Cardiology department two months prior to moving to our department for the study of syncope. During the hospital stay, the patient reports intense cervical pain accompanied by fever and, in the clinical analysis, elevated acute phase reactants. Magnetic resonance imaging of the cervical spine is carried out. Phlegmons are observed at the inter-vertebral disk C5-C6 with a collection at that level and cervical spondylodiscitis is diagnosed. In the blood cultures we find growing Staphylococcus epidermidis resistant to methicillin. Treatment with intravenous vancomycin and cefepime antibiotics is started. Transoesophageal echocardiography is performed, ruling out the presence of endocarditis and embolic aetiology of spondylodiscitis. Patient evolution is favourable during the first few weeks. Suddenly, towards the end of treatment a erythematous pruritic rash emerges with a 38 ºC fever and a decrease in diuresis until the patient experiences anuria and is moved to our department. Upon her arrival, the patient is conscious, haemodynamically stable and afebrile. She presents generalised maculopapular morbilliform rash as well as data suggestive of fluid overload with bibasilar crackles and lower extremity oedema.
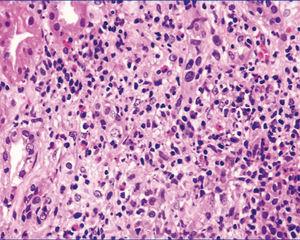
On the clinical analysis leukocytosis is observed with important eosinophilia and acute renal failure with creatinine: 6.1mg/dl, urea: 156mg/dl and vancomycin levels at 36.19µg/ml (normal levels: 5-10µg/ml). Vancomycin is immediately suspended and a catheter is placed the right femoral artery. Haemodialysis session begins. In the immunological study antinuclear antibodies, antineutrophil cytoplasmic antibodies, anti-GBM antibodies and protein electrophoresis were all within the normal range. Sterile blood and urine cultures are collected. Serology is extracted and tested for hepatitis B and C, human immunodeficiency virus, herpes virus, herpes 6, Epstein-Barr virus, Chlamydia and Mycoplasma, all with negative results. Suspecting immunoallergic acute renal failure, corticosteroids treatment is implemented on 3 daily doses of 250mg of methylprednisolone, followed by an intravenous dose of prednisone 1mg/kg. Later on, when the general state of the patient allows it, it is decided to carry out a renal biopsy. The biopsy includes 18 glomeruli, 6 of them with global sclerosis of the glomerular capillary. On the 12 preserved glomeruli, there are no significant intra-capillary lesions. A diffuse moderate tubulointerstitial lesion is detected, with inflammatory infiltrates made up of polymorphs formed by small lymphocytes, plasma cells and abundant eosinophils (Figure 1), and numerous images of tubulitis with lymphocyte infiltrates at the level of the tubular epithelium. On small arteries and small intralobular arteries there were no lesions. All the findings are compatible with the diagnosis of acute tubulointerstitial nephritis with eosinophils suggesting immunoallergic nephritis.
During patient evolution, we implement treatment with clavulanic-amoxicillin due to thrombophlebitis at the peripheral level, a new rash appears, along with increased leukocytosis with intense eosinophilia on the blood test and sudden dyspnea with wheezing related to eosinophilic pneumonitis. An internal consultation with the allergy Department takes place; they discourage the use of both vancomycin and beta-lactams. From the pulmonary point of view, we detect symptomatic improvement on the following 48 hours with some care. During evolution, we also found an increase in glutamic oxaloacetic transaminase (GOT), glutamic pyruvic transaminase (GPT) and γ-glutamyl transferase (GGT). The patient is diagnosed with DRESS syndrome affecting her skin, lung, liver and kidney. Corticosteroids therapy remains in place and a progressive improvement in renal function is evident without the need for a new haemodialysis session. The patient remains in the hospital for 15 days. By the time the patient is dismissed, there is evident improvement of the rash and renal failure is receding. Three months after hospitalization the patient presents 1.34 mg/dl of creatinine and proteinuria comes back negative.
The diagnosis of DRESS syndrome is established by the appearance, after being exposed to a drug, of skin eruptions, haematological alterations as eosinophilia or atypical lymphocytosis and systemic involvement in the form of adenopathies, hepatitis, interstitial neumonitis, carditis or interstitial nephritis. The incidence of the syndrome is estimated as 1 out of every 10 000 individuals exposed to the implicated drugs. The drugs more frequently associated with the syndrome are anti-convulsants but there have been cases involving anti-inflammatory drugs, allopurinol and antibiotics.2 The symptoms appear with a latency period that may vary between 1 and 8 weeks after exposure to drugs. As it has been suggested as an action mechanism, the presence of an allergic hyper sensibility reaction, in which medications act directly as antigens or indirectly as haptens.3 We have also found an association between the reactivation of infection by human herpes 6 virus4 or Epstein-Barr virus and DRESS syndrome. Treatment includes withdrawal from the suspected medication and corticosteroid treatment.5 Mortality varies, depending on the series, between 10% and 30%, and it comes with lung and/or hepatic affectations and sometimes with bacterial ulcer lesions.6
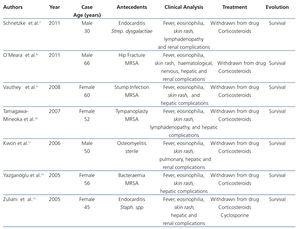
To our knowledge, this is the first case of DRESS syndrome by vancomicyn and beta-lactams, with systemic involvement and a renal biopsy confirming the existence of allergic tubulointerstitial nephritis, with good results after corticosteroids treatment. Table 1 displays cases diagnosed with DRESS syndrome due to vancomycin described in the literature.
Conflicts of interest
The authors have no conflict of interests to declare.
Figure 1. Haematoxylin and Eosin staining
Table 1. DRESS syndrome as an effect of Vancomycin