To the Editor:
The formation of pseudoaneurysms in prosthetic vascular accesses is a common event that is associated with fatigue of the prosthetic material secondary to repeated punctures and stenosis-occlusive damage in the venous drainage.1
Treatment is indicated when the pseudoaneurysm undergoes rapid growth, exceeds 2 times the diameter of the prosthesis, produces pain or a threat to cutaneous viability, or in cases of rupture.1
Traditionally, the treatment of this complication has been surgical; however, in recent years, several working groups have incorporated endovascular treatment using the placement of covered stents to exclude this type of lesion.2,3 Thrombin is not widely used as an embolising agent during the treatment of these lesions, with only a few reports of cases in which this type of treatment has been associated with a stent graft.4,5
Case report
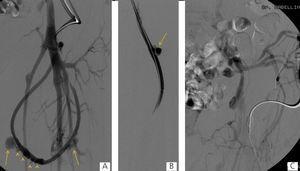
Here we present the case of a 46-year-old patient with chronic renal failure, on trimestral haemodialysis for 23 years secondary to obstructive uropathy, with a left femoral loop (21 months of use) with occluded iliac venous drainage that produced oedema in the leg and three pseudoaneurysms in the therapeutic range. One of these was actively bleeding. The three pseudoaneurysms and occlusion of the left primitive iliac vein were treated using endovascular methods under local anaesthesia. The actively bleeding pseudoaneurysm was excluded with a covered stent, and the other two were percutaneously embolised using balloon-assisted thrombin injections in order to avoid thrombosis in the prosthesis. The iliac venous axis was recanalised and treated with angioplasty balloons; in the final angiographic controls, we observed no pseudoaneurysms, with patency of the prosthesis, iliac venous drainage, no signs of collateral circulation, and without having produced any complications.
Discussion
Deterioration of the prosthetic material secondary to repeated punctures and stenosis-occlusive lesions in drainage veins represents one of the most common causes of pseudoaneurysms.1 In our case, the prosthetic material was worn down, in addition to a stenosis/occlusive lesion of the venous drainage and bleeding of one of the pseudoaneurysms, with oedema in the leg.
Traditionally, pseudoaneurysms were treated with open surgery; this procedure consisted of replacing the damaged segment of the graft, and if this were impossible, the vascular access was abandoned and another was created. Our patient had exhausted all options of vascular access, for which we decided to preserve the existing one.
Since the first publication by Sapoval in 1996, several cases have been reported in which aneurysms and pseudoaneurysms of vascular accesses were treated using an endovascular approach by placing a stent graft, with a success rate of as high as 100% according to some studies.2,3
The use of thrombin as an embolising agent has been widely studied in the treatment of femoral pseudoaneurysms, and this technique currently constitutes the standard practice for treating uncomplicated pseudoaneurysms. In the treatment of pseudoaneurysmal lesions of vascular accesses, we only have case reports of its isolated use4 or in association with a stent graft.5 Even so, we have not found any reference in the medical literature to the treatment of 3 pseudoaneurysms in the same patient using different techniques, in addition to revascularisation of the venous drainage system of a femoral loop.
Although the treatment of a vascular access with these characteristics may be the subject of debate, we believe that this was the best option in our case, since this was a patient with no other options for a vascular access.
Currently, endovascular treatment offers various alternatives for the treatment of this type of lesion, and so must be considered prior to programming surgery or abandoning the vascular access.
Conflicts of interest
The authors have no conflicts of interest to declare
Figure 1. Fistulographies
Figure 2. Stent, fluoroscopic images, and fistulography