To the Editor,
Distal renal tubular acidosis (RTA) is a relatively uncommon tubulopathy that is characterised by hyperchloremic metabolic acidosis, hypokalaemia, elevated urine pH (>5.5), and a negative anion gap. Early diagnosis can facilitate providing adequate treatment, which avoids potentially severe complications. Here we present the case report of a gestating mother (7 weeks) diagnosed with RTA.
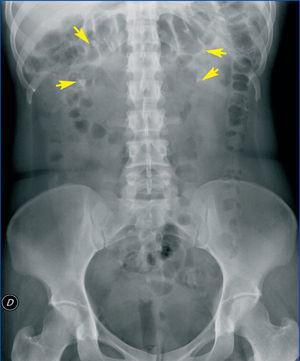
We treated a 28-year old pregnant woman (7 weeks gestation) that sought emergency treatment for intense weakness with vomiting and abdominal pain. She had a history of rhabdomyolysis secondary to severe hypokalaemia of an unknown cause, bilateral nephrocalcinosis, and nephrolithiasis (Figure 1). We reviewed the patient’s previous laboratory results and observed that she had hyperchloremic metabolic acidosis and hypokalaemia with persistently alkaline urine pH with several years’ evolution. Upon arrival in the emergency room, she had: AHT: 103/71mm Hg, HR: 78 systoles, deep abdominal palpation produced pain in the left hypochondria and fossa, with positive left renal percussion.
Blood analysis highlighted a pH of 7.18, bicarbonate at 12.4mmol/L with normal plasma anion gap, PCO2 at 35mm Hg, K+ at 3.3meqL, chlorine at 121 meq/l, creatinine at 0.62mg/dl, calcium at 8.3mg/dl, albumin at 3.3g/dl, and phosphorous at 3.6mg/dl. The urine sample resulted in: urine pH: 8; negative anion gap [Cl (66.2mEq/l) < Na+ (86mEq/l) + K+ (14.17mEq/l)]; diuresis: 3200ml/24h; calciuria: 137.7mg/24h; hypocitraturia (citraturia <102mg/24h), and normal oxaluria. The immunological analysis did not reveal any significant abnormalities.
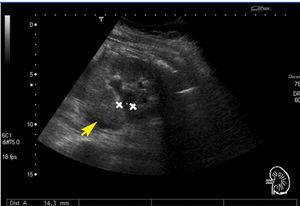
A renal ultrasound revealed grade II-III/IV pelvicalyceal dilatation of the left kidney and fluid collection in the left perirenal space (Figure 2). The patient was gestating with a live foetus. The urology department was advised of the situation, and they placed a left double J ureteral catheter, making passage through a left ureterolithiasis, resulting in the flow of urine with a purulent aspect. We later started treatment with antibiotics and intravenous potassium and bicarbonate, achieving clinical improvement. Based on the clinical symptoms, the previous laboratory analyses, and the current values, the patient was diagnosed with RTA.
RTA is a renal tubulopathy with hereditary aetiology that is idiopathic or secondary to any one of a variety of causes (Table 1). It is diagnosed based on the presence of electrolytic disorders that appear in blood and urine samples through venous gas measurements.
RTA in children tends to be primary or idiopathic. A genetic analysis allows for distinguishing the responsible mutation (over 50 have been described), the most relevant of which are alterations to the genes ATP6V0A4 and ATP6V1B1, this last one related to deafness.1 Early diagnosis can allow for correction of the metabolic acidosis, thus avoiding stunted development and rickets.2
Adult patients require a differential diagnosis in order to rule out associated autoimmune pathologies.3 We asked the patient to undergo a complete examination on several occasions without being able to establish an autoimmune aetiology. Hypercalciuria, hypocitraturia, and abnormally alkaline urine (and less frequently, hyperuricosuria) are situations that predispose the patient to the development of nephrolithiasis and nephrocalcinosis,4 making the patient prone to recurrent urinary infections. Renal function is conserved initially, but without appropriate treatment, patients develop chronic renal failure, AHT, and other complications. There is also a risk of acute renal deterioration with various aetiologies due to urinary infections or acute pyelonephritis, obstructive phenomena, or even rhabdomyolysis secondary to severe hypokalaemia.
Treatment in the initial phase consists of alkalising agents such as bicarbonate or citrate and correction of the hypokalaemia. In cases of RTA related to secondary aetiologies, controlling the responsible pathology aids in correcting the hydroelectrolytic disorders of RTA.5
We conclude that RTA is an uncommon tubulopathy whose early diagnosis avoids severe renal repercussions, although the evolution and prognosis of this condition are both favourable with proper treatment.
Conflicts of interest
The authors have no conflicts of interest to declare.
Table 1. Most common aetiologies in renal tubular acidosis
Figure 1. Simple abdominal x-ray
Figure 2. Left renal ultrasound