El manejo del anciano diabético con enfermedad renal crónica presenta peculiaridades que afectan tanto al control metabólico como a las medidas terapéuticas. Los objetivos de control glucémico han de individualizarse en función de la expectativa de vida, la afectación de la función renal, los riesgos de hipoglucemia y la comorbilidad. La metformina puede emplearse en monoterapia o asociada a otros antidiabéticos orales, pero debe suspenderse cuando el filtrado glomerular sea inferior a 30 ml/min. La gliclazida y la glipizida son sulfonilureas que no requieren ajuste de dosis en la enfermedad renal crónica, pero deben evitarse en los casos de enfermedad renal avanzada por el riesgo de hipoglucemia. De las meglitinidas, solo la repaglinida es recomendable en estos pacientes. Los inhibidores de las α-glucosidasas deben evitarse en pacientes con filtrado glomerular inferior a 25 ml/min o en diálisis. La pioglitazona no precisa ajuste de dosis, pero presenta efectos adversos potencialmente desfavorables en esta población. Los inhibidores de la dipeptidil peptidasa-4 son eficaces y bien tolerados. De ellos, la linagliptina no precisa ajuste de dosis. Los agonistas de los receptores del péptido similar al glucagón tipo 1 y los inhibidores del cotransportador sodio-glucosa tipo 2 no se recomiendan en ancianos con enfermedad renal avanzada. Finalmente la insulinoterapia, especialmente empleando los nuevos análogos de insulina, permite un manejo adecuado de la hiperglucemia de estos pacientes con diversas pautas terapéuticas que deben ser individualizadas para evitar la hipoglucemia.
Management of diabetic elderly patients with chronic kidney disease involves specific characteristics that affect both metabolic control and therapeutic measures. Blood glucose control targets should be individualised based on life expectancy, renal function, hypoglycaemia risk and comorbidity. Metformin may be used alone or in combination with other oral anti-diabetic drugs but must be discontinued when the glomerular filtration rate is less than 30mL/min. Gliclazide and glipizide are sulfonylureas that do not require dose adjustment in chronic kidney disease but they should be avoided in cases of advanced kidney disease because of the risk of hypoglycaemia. Repaglinide is the only meglitinide recommended in these patients. Alpha-glucosidase inhibitors must be avoided in patients with a glomerular filtration rate of less than 25mL/min or those undergoing dialysis. Pioglitazone does not require dose adjustment but it has potentially adverse effects in this population. Dipeptidyl peptidase-4 inhibitors are effective and well tolerated. Of the latter, linagliptin does not require dose adjustment. Glucagon-like peptide-1 receptor agonists and sodium-glucose cotransporter 2 inhibitors are not recommended in elderly patients with advanced kidney disease. Lastly, insulin therapy, particularly using the new insulin analogues, allows adequate management of hyperglycaemia in these patients, with different therapeutic regimens that must be individualised in order to avoid hypoglycaemia.
INTRODUCTION
Ageing is accompanied by changes in renal function. Furthermore, carbohydrate metabolism disorders are also very prevalent in the elderly population1,2. The prevalence of diabetes mellitus (DM) clearly increases with age3.
Chronic kidney disease (CKD) is a common complication of DM, with the latter being the main cause of ESRD, which requires renal replacement therapy4,5. Increased life expectancy and a higher DM incidence lead to an increase in the number of elderly diabetic individuals with CKD.
Treating DM in elderly patients is more complicated and there are more limitations than in the adult population, due to a higher risk of hypoglycaemia and its serious consequences6-11. Renal function in the elderly may be compromised, not only due to old age, but also due to the coexistence of DM. Likewise, CKD also limits treatment options in DM.
KIDNEY DISEASE IN THE ELDERLY
Ageing is a natural and inevitable biological process that affects all organs. As part of this process, In kidneys of healthy elderly people, a series of changes occurs that affect both (Table 1). The main functional changes are a decrease in the glomerular filtration rate (GFR) and in effective renal plasma flow. In fact, GFR decreases from a maximum value of around 140ml/min/1.73m2 in the third decade of life at a rate of approximately 8ml/min per decade12. Lastly, very old healthy individuals (>85 years), despite having an age-associated decreased GFR (~50 ml/min), have different characteristics from CKD patients: 1) they do not have anaemia, since proximal tubule function is preserved in healthy elderly individuals 2) urea, calcium, phosphorus and magnesium levels are normal and 3) systematic urine analysis is normal, without the presence of haematuria or proteinuria13.
With the introduction of the K/DOQI (Kidney Disease Outcomes Quality Initiative)14 guidelines, the classification of CKD is now based on the GFR grade and signs of renal damage (haematuria, proteinuria), and CKD is classified in 5 stages. However, its weak point is that it considers CKD individuals to be any patient with a GFR <60ml/min or ≥60ml/min with signs of renal damage, without taking into account either the influence of age or the existence of other laboratory abnormalities associated with the presence of kidney disease.
The new 2012 KDIGO (Kidney Disease: Improving Global Outcomes)15 guidelines maintain the definition of CKD based on the presence, for more than 3 months, of renal damage markers along with a decrease in the GFR and they add a risk stratification based on the degree of urinary albumin elimination: A1 <30mg/24h (normal-slight), A2, 30-300mg/24h (moderate), A3 >300mg/24h (severe). These guidelines continue to be valid for the whole population, including the elderly population and, therefore, healthy elderly individuals with a moderately reduced GFR, for example, between 45 and 60ml/min, may still erroneously be classified as having kidney disease16. Therefore, the most adequate definition of CKD in an elderly patient may be considered to be the presence of a GFR <60ml/min maintained over time, along with signs that are characteristic of kidney disease.
The combination of demographic factors, an ageing population, an increased DM incidence and more flexible criteria for starting renal replacement therapy result in a higher proportion of diabetic elderly patients with ESRD17.
DIABETES MELLITUS IN ELDERLY PATIENTS
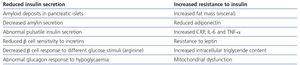
Carbohydrate metabolism disorders are also common in the elderly population (Table 2). Both the secretion of insulin and its peripheral action may be compromised as age increases1,2.
DM prevalence increases in elderly individuals. In our country, carbohydrate metabolism disorders are more common in the 61-75 year old age group, where overall diabetes prevalence (known and unknown) is 42.4% and 29.8% in males and females, respectively18.
The elderly population is not homogeneous. Different factors such as age, their functional and cognitive situation, comorbidity and life expectancy must always be borne in mind whenever we refer to this population group. In clinical practice, we distinguish between four elderly patient groups according to the functional and cognitive situation and the condition of their health: healthy elderly individual, unhealthy elderly individual, frail elderly individual and geriatric patient19.
Elderly diabetic patients may suffer from incidental diabetes (diabetes diagnosed ≥65 years) or prevalent longstanding diabetes (diagnosed in adulthood). Incidental diabetes is generally associated with better blood glucose control, a lower likelihood of insulin treatment and a lower presence of retinopathy than prevalent diabetes. However, there are not usually differences between the two forms in the presence of cardiovascular disease or peripheral neuropathy3.
In the elderly, diabetes is accompanied by certain specific characteristics that must be borne in mind, such as comorbidity, cardiovascular risk factors, frailty, limited life expectancy, unintentional weight loss, changes in body composition, polypharmacy with the possibility of enhancing drug interactions, high risk of hypoglycaemia and difficulty in recognising it, social isolation, functional and dependency situations, the socioeconomic situation, the family environment, geriatric syndromes, as well as desire and therapeutic preferences6-11.
Elderly individuals with diabetes may have both micro and macrovascular chronic complications from diabetes, which further hinders therapeutic management8,10. Likewise, acute complications, such as a hyperosmolar hyperglycaemic state and severe hypoglycaemia, are more prevalent and dangerous in elderly individuals ≥75 years of age9.
Despite the high number of elderly patients with diabetes, few clinical trials have been carried out specifically in this population or consensuses especially designed for them7,9,10. To date, there have been no long-term randomised studies that show the benefits of intensive blood glucose control in the elderly population. As such, the benefits obtained with intensive blood glucose control in the adult population have often been extrapolated.
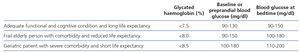
The therapeutic targets in elderly individuals with diabetes depend on various factors including the patient’s functional condition, their cognitive state, their life expectancy, the duration of diabetes and a history of cardiovascular disease and of severe hypoglycaemia. In line with the 2013 American Diabetes Association’s recommendations11, elderly patients with diabetes who have an adequate functional and cognitive state with a long life expectancy, allowing them to obtain the benefits of long-term intensive diabetes treatment, may be treated with similar therapeutic targets to those that are pursued in young adults with diabetes, while always avoiding the development of hypoglycaemia (Table 3).
DIABETES IN ELDERLY PATIENTS WITH KIDNEY DISEASE
Diabetes is the main cause of CKD in developed countries. Furthermore, in individuals with diabetes, CKD significantly increases cardiovascular morbidity and mortality and it is the main reason for renal replacement therapy. Given the high prevalence of CKD and DM in the elderly population, it is not surprising that the percentage of elderly individuals with both disorders is also high. CKD prevalence according to K/DOQI14 criteria in individuals (mean age, 67.9±13 years) with type 2 DM controlled in Primary Care in our country was 34.6%20.
Currently, there are no randomised studies specifically designed for elderly patients with CKD and DM, and as such, we must apply the conclusions obtained in the adult population (Table 4). The benefit of controlling blood glucose in elderly patients with DM and CKD would be greater in those recently diagnosed with DM, younger patients, those with a greater life expectancy, those with less renal function involvement and those with fewer comorbidities. By contrast, this benefit would be lower in frail elderly individuals with many comorbidities, a high risk of hypoglycaemia and of falling, and a reduced life expectancy or geriatric patients. As such, blood glucose control targets should be adapted to the type of elderly individual with kidney disease, at all times avoiding the acute complications (hypoglycaemia and hyperosmolar hyperglycaemic state or ketoacidosis) of DM.
The therapeutic strategy for DM in elderly CKD patients must be individualised in accordance with the blood glucose control target previously established and agreed with these patients, their family members and/or carers. The Primary Care doctor should assess kidney disease progression in elderly patients to decide whether or not to refer them to the Nephrology specialist. Furthermore, other cardiovascular risk factors (high blood pressure, hyperlipidaemia, CKD, etc.) should be addressed in a comprehensive and individualised manner, in line with the recommendations of the main clinical guidelines9,21,22.
ORAL DRUGS
Pharmacotherapy of hyperglycaemia in elderly patients with DM and CKD should be individualised using drugs associated with the lowest possible risk of hypoglycaemia, for which it is necessary to decrease the dose of some or avoid others23-26. Treatment with oral anti-diabetic drugs in the initial stages (stages 1 and 2) of CKD is relatively safe. However, in advanced stages (stages 4 and 5) commonly observed in the elderly population, the risk of hypoglycaemia increases.
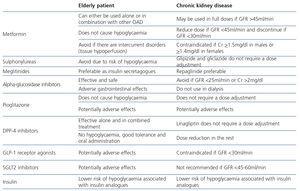
Metformin is the first line drug and the drug of choice in the treatment of type 2 DM. It acts through different mechanisms, such as inhibiting glucose production in the liver, increasing the use of insulin-mediated glucose by peripheral tissues and reducing circulating free fatty acids, which decreases gluconeogenesis. This drug does not cause hypoglycaemia by itself and it achieves a significant reduction in A1c of around 1.5%. Its use is the basis of treatment not only in adults but also in elderly individuals with type 2 DM. Observational studies have demonstrated that metformin is associated with a more favourable prognosis in the elderly population, including for mortality. One of its main limitations is that it is mainly eliminated via the kidneys and, therefore, it is accumulated in the case of renal failure, with the resulting risk of lactic acidosis. This is particularly important in elderly individuals, since ~20% of the latter have a GFR <60ml/min27. For this reason, it is recommended to reduce the drug dose if the GFR is <45ml/min and discontinue it if the GFR is <30ml/min28. Other common special situations in elderly CKD patients that may lead to lactic acidosis are those that involve tissue hypoperfusion, such as dehydration (vomiting and/or diarrhoea), acute cardiorespiratory failure, acute intercurrent disorders and the use of iodinated x-ray contrast media.
Different studies have shown a high percentage of CKD patients treated with metformin without an increased risk of hospitalisation or death. Recently, a multicentre observational study carried out on Italians that analysed age, renal dysfunction, cardiovascular disease and pharmacological treatment of type 2 DM showed that in real life conditions, the percentage of elderly patients (≥74 years) with DM and (stages 3 and 4) CKD treated with metformin was 39.3% and 14.3%, respectively. Metformin use was independently associated with a lower prevalence of cardiovascular disease, regardless of age and the degree of renal function29.
Insulin secretagogues, sulfonylureas (SU) and meglitinides (repaglinide and nateglinide) are drugs that stimulate endogenous insulin secretion by pancreatic β cells. Glipizide and gliclazide, two second-generation SU, are recommended in patients with advanced CKD, kidney transplants or those on dialysis, since they do not require dose adjustment because they are metabolised to inactive compounds24. However, since SU are potent hypoglycaemic agents, their use in the elderly should be restricted due to their high capacity to produce severe and prolonged hypoglycaemia. This complication is more common in cases of a reduced GFR, due to their long half-life and the elimination via the kidneys either of the unchanged drug or its active metabolites, and as such, their use does not seem advisable in elderly diabetic patients with CKD.
Meglitinides are short-acting insulin secretagogues that act preferentially on postprandial hyperglycaemia. Their shorter half-life compared to SU reduces the risk of hypoglycaemia, especially in elderly patients with an irregular intake pattern. Both meglitinides are metabolised in the liver, but, as with some SU, nateglinide metabolites are active and are eliminated via the kidneys, stherefore, only repaglinide use is reduced GFR. Repaglinide has proven to be safe and effective in elderly diabetic individuals with varying stages of CKD (≤20 GFR ≤80ml/min)30. In patients with advanced stages of CKD, a dose reduction is recommended in accordance with blood glucose levels.
Intestinal alpha-glucosidase inhibitors such as acarbose and miglitol reduce the postprandial glucose peak on delaying the conversion of complex carbohydrates to monosaccharides in the intestines. These drugs are potentially beneficial in elderly diabetic individuals both alone and as combined treatment, including with insulin. Miglitol is absorbed in the intestines and is not metabolised, but rather eliminated unchanged in urine; however, acarbose is metabolised in the gastrointestinal mucosa, its absorption is low and its elimination via the kidneys is <2%23. Its use is advised against in advanced stages of CKD (GFR <25ml/min or serum creatinine >2mg/dl), and in dialysis23,25.
Pioglitazone is a glitazone that increases peripheral sensitivity to insulin through activation of the peroxisome proliferator-activated receptor gamma and it improves the lipid profile by activating receptors that regulate the expression of genes involved in glucose and lipid metabolism, respectively. Pioglitazone has the advantage of not causing hypoglycaemia and being potentially beneficial in secondary prevention due to its anti-inflammatory and anti-atherogenic effects. Given its essentially hepatic metabolism, pioglitazone can be used in CKD23,25,31. However, the slightly increased risk of bladder cancer, macular oedema, bone loss and risk of fracture and heart failure, conditions associated with both pioglitazone and age, would limit its use in elderly individuals with and without CKD.
Dipeptidyl peptidase-4 (DPP-4) inhibitors or gliptins (sitagliptin, vildagliptin, saxagliptin and linagliptin) inhibit DPP-4, an enzyme that deactivates different gastrointestinal hormones called incretins, such as the glucose-dependent insulinotropic peptide and glucagon-like peptide-1 (GLP-1). Inhibition of this enzyme extends the half-life of these incretins, prolonging their biological action, including the stimulation of endogenous insulin secretion and the reduction of glucose-dependent postprandial glucagon secretion, thus contributing to improving blood glucose control. These drugs are an attractive therapeutic option in the elderly, as they are not associated with hypoglycaemia, they have good tolerance, no significant drug interactions and they may be administered orally32. There has been little experience with these drugs in elderly diabetic patients (≥75 years). Data have been obtained with vildagliptin, which has proven to be an effective and safe drug in this population33. A study has recently been published that has shown that adding linagliptin to other oral anti-diabetic drugs in elderly diabetic patients (age >70 years) is effective as a hypoglycaemic drug and has a similar safety profile to the placebo34. Different studies have demonstrated the efficacy and safety of these drugs in CKD35. Linagliptin, due to its metabolism in the liver, is the only gliptin that does not require a dose adjustment in CKD36; however, the other gliptins require a dose reduction as the GFR decreases37. Vildagliptin use (50mg/day) in elderly diabetic patients (age ≥75 years) with moderate to severe CKD (mean estimated GFR ~35ml/min/1.73m2) was effective, safe and well-tolerated, compared with the placebo38.
OTHER DRUGS
GLP-1 agonists are human GLP-1 analogues (liraglutide) or analogues of exendin-4 (exenatide and lixisenatide), a natural peptide isolated from the saliva of the Gila monster (Heloderma suspectum), whose amino acid chain overlaps (53%) with that of the human GLP-1, which allows it to activate its receptors. These drugs are much more resistant to DPP-4 than endogenous incretin, which prolongs their biological activity. As with DPP-4 inhibitors, they increase glucose-dependent insulin secretion by β cells, they inhibit glugacon secretion, which slows down hepatic gluconeogenesis, but they also slow down stomach emptying, which delays circulation of glucose from intake, they increase the sensation of thirst and reduce intake39. These drugs have a greater hypoglycaemic effect than DPP-4 inhibitors and, furthermore, they are accompanied by weight loss40. Their disadvantages are intolerance, with frequent nausea and vomiting, the need for them to be administered parenterally and their high cost. Although they have been considered an attractive therapeutic option in elderly diabetic patients41, reduced appetite and gastrointestinal discomfort may be disadvantages in this population, particularly in fragile elderly individuals with kidney function involvement. These drugs are also contraindicated in cases of advanced CKD (GFR <30ml/min).
Sodium-glucose cotransporter 2 (SGLT2) inhibitors (canagliflozin and dapagliflozin) are a new class of oral anti-diabetic drugs that, as well as improving glygated haemoglobin without causing hypoglycaemia, reduce body weight and systolic blood pressure42. These drugs reduce glucose reabsorption in the proximal convoluted tubule, increasing glycosuria. They are not recommended in CKD (GFR <45-60ml/min). Their disadvantages include their relationship with genital and urinary infections, volume depletion and a higher incidence of bladder and breast cancer associated with dapagliflozin42. Both the mechanism of action and undesirable effects make these drugs unattractive for use in elderly diabetic patients with CKD.
INSULIN THERAPY
Insulin is the most potent and effective form of hypoglycaemic treatment, and it is therefore associated with an increased risk of hypoglycaemia. This is particularly significant in the elderly population, because hypoglycaemia can have serious clinical consequences. The current availability of long-acting insulin analogues such as insulin glargine (one daily dose) or insulin detemir (one or two daily doses), and some more recently introduced forms such as insulin degludec, allows the use of a basal insulin, either alone or in combination with oral anti-diabetic drugs, which facilitates blood glucose control with a lower risk of hypoglycaemia than with NPH insulin. In insulin-dependent elderly diabetic individuals, the use of basal-bolus therapy with short-acting insulin analogues such as insulin aspart, insulin lispro or insulin glulisine reduces the risk of hypoglycaemia compared with regular insulin43.
The kidney is the main organ responsible for exogenous insulin metabolism, and as such, its metabolism is impaired in CKD patients. This causes insulin requirements to decrease as the GFR decreases. In this regard, it is recommended to reduce the insulin dose by 25% or 50% whenever the GFR is 10-50ml/min and <10ml/min, respectively44. Although intensive insulin therapy (two or more doses of insulin) is associated with a better diabetic nephropathy prognosis, it also increases the frequency of hypoglycaemic events compared with basal insulin therapy. A lower hypoglycaemia rate associated with short-acting insulin analogues compared with that of regular human insulin, along with their greater administration flexibility, makes these insulin analogues attractive drugs in the management of insulin-dependent diabetes in elderly individuals with CKD45.
KEY CONCEPTS
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Age-related structural and functional changes in the kidney (46-50)
Table 2. Age-related carbohydrate metabolism disorders (1,2)
Table 3. Blood glucose control targets in the elderly in accordance with functional and cognitive condition and life expectancy (9,11)
Table 4. Therapeutic considerations in the pharmacological treatment of diabetes in the elderly and in chronic kidney disease