The use of medications concerns to patients and healthcare professionals, and there may be errors with significant clinical repercussions.1 There are factors that contributes to these errors: pluripathology, polymedication, healthcare system fragmentation (with multiple prescribing physicians and absence of a single health record), as well as a lack of knowledge of the treatment by the patient and/or the family or caregivers. Several processes have been proposed to decrease these medication errors, including medication reconciliation (creating a precise list of medication that compiles all the drugs that the patient is taking), treatment review (evaluating the list for suitability, effectiveness, safety and convenience in conjunction with the patient's state of health) and personalised therapeutic management (confirming adherence, knowledge of drugs and list of medication “in the wallet”). Conciliation of the treatment should be done by a multidisciplinary group (physicians, nurses and pharmacists), in all patients, including all medications, covering all healthcare processes (in-hospital and as outpatient). Since this is a costly process, priority has been given to patients with chronic disease, polymedicated and with multiple pathologies, generally in healthcare transition and for groups of drugs more commonly involved in adverse reactions (with preference given to drugs that should be reconciled within 4h of admission, drugs that should be reconciled within 24h of admission, drugs with a narrow therapeutic index, drugs with multiple interactions and drugs wit high-risk).2,3 Given that patients in dialysis are at a high risk, we conducted a study to determine which drugs were prescribed on our unit, as well as medication adherence and knowledge on the part of the patients and/or caregivers as a starting point for reconciliation.4–7
We conducted a prospective, observational study on a cohort of patients in peritoneal dialysis from February to May 2015. The following variables were collected: age, sex, time in dialysis, comorbid conditions (diabetes mellitus, cardiovascular disease and hypertension), number of drugs, number of pills per day, type of medication (drugs that required reconciliation within 4h of hospital admission, drugs that required reconciliation within 24h of hospital admission, drugs with a narrow therapeutic index, drugs with multiple interactions and high-risk drugs) and number of prescribing physicians. Adherence was calculated using the Morisky-Green questionnaire,8 and knowledge was calculated using the knowledge and abilities assessment scale (adaptation of 2 scales, DRUGS and MedTake).9 Statistical analysis was performed with the SPSS® version 15.0 software programme.
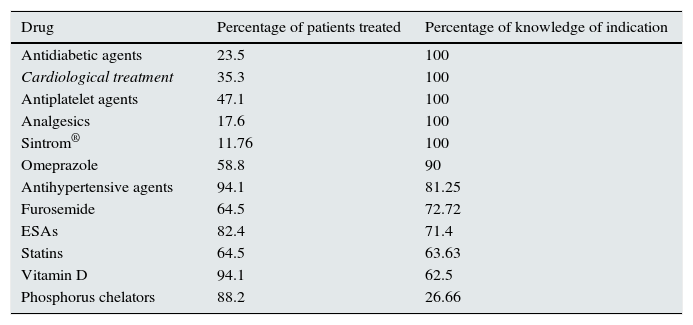
The 17 patients enrolled, including 4 women (23.8%), had a mean age of 65.29 years (47–86), a mean time in dialysis of 38.7 months (3–93) and the following comorbidity: diabetes mellitus, 23.5%; cardiovascular disease, 23.5%; and hypertension, 100%. The number of prescribing physicians in the last 24 months was 8 (6–11). Medication-related data: number of drugs, 12.59 (9–17); number of pills, 13.59 (8–27); drugs that required reconciliation within 4h of admission, 13 (76.5%); drugs that required reconciliation within 24h of admission, 17 (100%), drugs with multiple interactions, 16 (94.2%); drugs with a narrow therapeutic index, 3 (17.6%); high-risk drugs, 17 (100%). Five patients (29.4%) required help with completion of forms. Adherence was 76.6%, and overall lack knowledge about the therapeutic indication was 52.94%. Table 1 shows knowledge according to therapeutic group.
Knowledge according to therapeutic group (knowledge and abilities assessment scale adapted from DRUGS and MedTake).
| Drug | Percentage of patients treated | Percentage of knowledge of indication |
|---|---|---|
| Antidiabetic agents | 23.5 | 100 |
| Cardiological treatment | 35.3 | 100 |
| Antiplatelet agents | 47.1 | 100 |
| Analgesics | 17.6 | 100 |
| Sintrom® | 11.76 | 100 |
| Omeprazole | 58.8 | 90 |
| Antihypertensive agents | 94.1 | 81.25 |
| Furosemide | 64.5 | 72.72 |
| ESAs | 82.4 | 71.4 |
| Statins | 64.5 | 63.63 |
| Vitamin D | 94.1 | 62.5 |
| Phosphorus chelators | 88.2 | 26.66 |
Our patients had a high risk of having problems related to medication: multiple drugs, large number of pills per day and high number of prescribing physicians. The majority of patients received drugs that required reconciliation within 4h of admission with multiple interactions or high-risk medicines. They showed a good level of adherence (76.6%), with a broad knowledge of cardiological medication (antiplatelet agents, antiarrhythmic agents and anticoagulants), antihypertensive agents, gastroprotective agents, antidiabetic agents and analgesics, and poor knowledge of treatments related to complications of kidney disease and dialysis (phophate binding and erythropoiesis-stimulating agents [ESAs]).
C. Everett Koop, stated: “Drugs don’t work in patients who don’t take them”. Therefore, it is advisable to generate a list showing all the medicines that the patient is taking and how he or she takes them and ensure that he or she is receiving medication in appropriate, effective and safe manner for his or her clinical situation, taking into account the indication for each drug and the convenience of taking it (the patients enrolled in our study had poor knowledge of drugs, especially drugs related to their kidney disease). The dialysis centre should be the “centre for health” and information on medication, given that no physician knows the patient better than the dialysis team. Errors should be detected at regular intervals (3–4 months) or in each transition (visit to other specialists, change in medication or hospital admission), the patient should receive a printed copy of the reconciled medication list and, until there is a comprehensive electronic system, the patient should be advised to carry in his or her wallet the reconciled medication list so that it is always available, for any healthcare personnel in any health field.
Please cite this article as: González López A, Nava Rebollo Á, Andrés Martín B, Herrera Gómez F, Santana Zapatero H, Diego Martín J, et al. Grado de adherencia y conocimiento previo a la conciliación terapéutica en pacientes en diálisis peritoneal. Nefrología. 2016;36:459–460.