Dear Editor,
Cryptosporidium parvum is an intracellular protozoan that can produce gastroenteritis in humans. In immunodepressed patients the infection can be severe and lead to persistent diarrhoea and endanger life. There is limited experience with the treatment of this infection in solid organ recipients. We describe the importance of diagnosis and early treatment in a case of severe cryptosporidiosis in a kidney transplant recipient. To optimise the patient’s immunological status and resolve the infection it is necessary to apply antibiotic treatment, together with the reduction of immunosuppression.
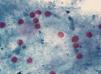
We present the case of a 78 year old woman with chronic kidney disease, secondary to chronic interstitial nephropathy on haemodialysis since February 2003. She received a kidney transplant from a deceased donor in December 2003 with a basal CRP of 2 mg/dl. The patient was being treated with steroids, mofetil mycophenolate and tacrolimus. Steroids were discontinued 3 months post-transplant. In June 2008 the patient was admitted with watery diarrhoea without any pathological substance that had a 7 day evolution, without fever, vomiting or abdominal pain. The patient also had haemodynamic instability and a blood pressure of 80/50 mmHg, her diuresis rhythm decreased and renal failure deteriorated to CRP and plasma urea levels of 4.3 and 177 mg/dl, respectively. As diarrhoea persisted in spite of absolute diet and saline therapy, treatment with metronidazol and ciprofloxacin was initiated. The detection of adenovirus and rotavirus antigens in faeces, and the culture and cytotoxicity in direct faeces samples to Clostridium difficile were negative. In the analysis of fresh faeces no parasites were observed. Antigen tests and quantitative PCR for cytomegalovirus (CMV) were negative. Finally, and in view of the poor evolution of the patient, modified Kinyoun stain (Figure 1) was used and Cryptosporidium oocysts were seen in the faeces. Treatment, therefore, began with paramomycin and azithromycinuntil for a period of 14 days. Subsequently nitazoxanide was administered for 6 days and the doses of mofetil mycophenolate and tacrolimus were reduced. After these measures were taken, diarrhoea disappeared and kidney function recovered to basaline levels and 17 months later the patient was still asymptomatic.
Acute diarrhoea is a significant complication in solid organ transplant recipients (SOTR). The differential diagnosis of acute diarrhoea in these cases is difficult, since both microorganisms and immunosuppressive medication can be involved, especially mofetil mycofenolate.1
Our patient maintained a stable kidney function for 5 years after transplant with double immunosuppressive therapy. Drug levels remained stable, therefore it was ruled out that the diarrhoea could be secondary to immunosuppressive therapy. Suspected diagnosis was microorganisms; the usual ones were quickly ruled out, including Clostridium difficile2 and CMV.
Cryptosporidium parvum is an intracellular protozoan that causes gastrointestinal disease worldwide, since it is an intestinal parasite of domestic and wild animals. This infection is more common in developing countries. The parasite is initially transmitted by the faecal-oral route, and in epidemics it has been associated with contaminated municipal water, person-to-person transmission and even animal-to-person transmission.3
Clinical symptoms of cryptosporidiosis depend on the host’s immunological status. In immunocompetent subjects it causes self-limited diarrhoea, but in immunodepressed patients the infection can be prolonged and life-threatening, since there is no specific antiparasite drug.4,5 In addition to intestinal involvement, in immunosuppressed patients, cases have been described with respiratory system, gallbladder and sclerosing cholangitis involvement.6
Microbiological diagnosis depends on the observation of the parasite in the faeces using a microscope and a modified Ziehl-Neelsen stain or modified Kinyoun stain that reveal the presence of 4-6 micron red oocysts. Several samples of faeces collected on subsequent days must be examined since oocyst shedding is intermittent.7
The cornerstone of treatment in immunodepressed patients is correction of electrolyte and acid base balance disorders.4 This infection can be treated with nitazoxanide, paromomycin and azithromycin. However, clinical response is variable and the intestinal protozoan can be difficult to eradicate. It would seem that in a SOTR reduction of immunosuppression, together with antimicrobial treatment, can improve immunological status and achieve infection resolution.8
This case is interesting due to the importance of suspecting this infection in any immunodepressed patient who develops diarrhoea when no other cause is found.
Figure 1. Modified Kinyoun stain