The presence of persistently high urinary concentrations of protein or albumin is considered a sign of kidney damage. Nowadays, the diagnosis of chronic kidney disease (CKD) is based on the presence of signs of kidney damage together with the estimation of the glomerular filtration rate. The presence of either proteinuria or albuminuria identifies a group of patients with a higher risk of progression of CKD and higher cardiovascular risk. Treatment with angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers decreases both the progression of CKD and the incidence of cardiovascular events and death in patients with CKD and proteinuria. Thus, proteinuria is currently considered a therapeutic target by itself.
Despite the importance of detecting and monitoring proteinuria in the diagnosis and follow-up of CKD, there is no consensus among the clinical practice guidelines published by different scientific societies on the diagnostic cut-off levels, on different sampling procedures, on the units used in laboratory reports or just on whether it should be defined in terms of albuminuria or proteinuria.
The goal of this document, created with the agreement of the Spanish Society of Clinical Biochemistry and Molecular Pathology (SEQC, representing its Spanish acronym) and the Spanish Society of Nephrology (S.E.N.), is to recommend appropriate guidelines to medical and laboratory physicians for detecting and monitoring proteinuria as a marker of CKD in adults and children. These recommendations are the result of searching, evaluating and summarising current scientific evidence published in the last few years.
La presencia de concentraciones elevadas de proteína o albúmina en orina, de modo persistente, es un signo de lesión renal y constituye, junto con la estimación del filtrado glomerular, la base sobre la que se sustenta el diagnóstico de la enfermedad renal crónica (ERC). Su presencia identifica a un grupo de pacientes con un riesgo superior de progresión de la enfermedad renal y con mayor morbilidad cardiovascular. El tratamiento con inhibidores de la enzima de conversión de la angiotensina o antagonistas del receptor de la angiotensina, en individuos con ERC y proteinuria, ha demostrado que disminuye tanto la progresión de la enfermedad renal como la incidencia de eventos cardiovasculares y muerte, por lo que la disminución del valor de la proteinuria es considerado un objetivo terapéutico.
Pese a la importancia de la detección y monitorización de la proteinuria en el diagnóstico y seguimiento de la ERC, no existe consenso entre las guías de práctica clínica publicadas por distintas Sociedades científicas sobre cuáles son los valores que indican su presencia, si ésta debe ser definida en términos de albúmina o de proteína, el espécimen más adecuado para su medida o el tipo de unidades en que deben ser expresados los resultados.
La finalidad de este documento, elaborado con el consenso de la Sociedad Española de Bioquímica Clínica y Patología Molecular (SEQC) y la Sociedad Española de Nefrología (S.E.N.), es proporcionar recomendaciones, a los facultativos clínicos y de laboratorio, para la detección y monitorización de la proteinuria como marcador de la presencia de ERC en adultos y en niños. Las recomendaciones son el resultado de la búsqueda, evaluación y síntesis de la evidencia científica publicada sobre el tema en los últimos años.
INTRODUCTION
Different epidemiological studies have shown that chronic kidney disease (CKD) has a high prevalence.1-4 The number of patients with advanced CKD requiring renal replacement therapy has increased in the last few years as a result of an aging population and the fact that older patients and patients with associated conditions are now included on dialysis. Furthermore, the incidence and prevalence of CKD due to glomerulonephritis or type 1 diabetes mellitus (DM) has stabilised and today, atherosclerosis, type 2 DM or hypertension are now the main causes of CKD; these are conditions that may affect kidney function silently. This is why CKD is detected at an advanced stage. Diagnosing the disease early is important to prevent kidney function from deteriorating as well as cardiovascular complications responsible for the high morbidity and mortality of these patients compared to individuals with similar clinical symptoms but without CKD.5
Different studies promoted by the Spanish Society of Nephrology (S.E.N.) report that CKD has a prevalence of around 9.16% in the population of over-18s.6 It also reaches values of 21% in patients attended by primary care physicians.7 The data from the registers of CKD stage 5 patients on renal replacement therapy (haemodialysis, peritoneal dialysis or kidney transplantation) show an incidence and prevalence of 129 and 1039 patients per million inhabitants/year, respectively.8
The Spanish registry of children with chronic kidney disease (REPIR II, abbreviation in Spanish), which includes pre-dialysis patients diagnosed with CKD stage 2-5, shows an incidence and prevalence rate of 8.6 and 71.0 cases per million inhabitants/year, according to the data from 2008.9 The most frequent causes of CKD in children are obstructive uropathy secondary to congenital defects, glomerulonephritis and hypertension.10
The presence of persistently high urinary concentrations of protein or albumin is a sign of kidney damage. Diagnosis of CKD is based on the presence of signs of kidney damage together with the estimation of the glomerular filtration rate (GFR).11 The presence of high urinary concentrations of protein or albumin shows a higher risk of kidney disease progression12-18 and a higher cardiovascular morbidity19,20; furthermore, this risk is linear and continuous, even for concentrations within the reference range.21 Treatment with angiotensin-converting enzyme inhibitors (ACEI) or angiotensin-receptor blockers (ARB) in patients with CKD and proteinuria has been shown to reduce the progression of kidney disease as well as the incidence of cardiovascular events and death. Reducing the level of proteinuria is therefore a therapeutic target by itself.22-30
Despite the importance of detecting and monitoring proteinuria in the diagnosis and follow-up of CKD, there is no consensus between the clinical practice guidelines published on the cut-off values, whether it should be defined in terms of albuminuria or proteinuria, the most appropriate sampling procedure, or how useful reagent strips are as an initial screening method.
OBJECTIVE AND SCOPE
The objective of this document is to provide recommendations for detecting and monitoring proteinuria as a CKD marker in adults and children. The recommendations are different for each group due to the differences in prevalence and the type of disease responsible for the CKD in each group.
METHODOLOGY USED TO PREPARE THE DOCUMENT
The recommendations in this document are the results of searching, evaluating and summarising current scientific evidence on the assessment of proteinuria in the diagnosis and follow-up of CKD. The information has been collected principally from clinical practice guidelines published in recent years.
The level of evidence or strength of the recommendations has not been included in this document, as it is impossible to exchange the grading systems used by each scientific society. The guidelines consulted as well as their evidence-grading systems are described at the end of the document (Appendix).
CURRENT DIAGNOSIS CRITERIA AND CLASSIFICATION OF CHRONIC KIDNEY DISEASE
The National Kidney Foundation (NKF)-Kidney Disease Outcomes Quality Initiative (K/DOQI) defines the following diagnosis criteria in its guidelines on the evaluation, classification and staging of CKD11:
1. GFR under 60ml/min/1.73m2 during a time period greater than or equal to three months.
2. The presence of kidney damage, with or without a decrease in the GFR, during a time period greater than or equal to three months. The concept of kidney damage refers to structural or functional abnormalities of the kidney manifested directly by histological disorders in the kidney biopsy, or indirectly, from the presence of albuminuria, proteinuria, urine sediment abnormalities or imaging techniques.
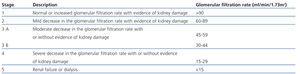
The combination of both diagnostic criteria is the basis for CKD classification in 5 stages (Table 1). In stages 1 and 2, the presence of kidney damage on its own is used to diagnose CKD.
This definition and classification into stages has been accepted by the large majority of scientific societies, including the S.E.N.31 and the international initiative Kidney Disease: Improving Global Outcomes.32 In recent years, changes have been proposed to this classification such as: a) adding the letter “T”, “D” or “p” to identify patients with kidney transplants, on dialysis and with proteinuria, respectively33-35; b) the subdivision of stage 3 CKD into 3A (GFR 45-59ml/min/1.73m2) and 3B (30-44ml/min/1.73m2)32,34,36.37; c) the elimination of stages 1 and 238 or combining these into one stage,39 given that there is no optimum measurement of kidney function in this range of GFR; d) the need for additional evidence of kidney damage for GFR values over 30 or 45ml/min/1.73m2 as a prerequisite for diagnosing CKD40,41; e) decreasing the cut-off point from 60 to 45ml/min/1.73m2 for stage 3 CKD42; or f) introducing GFR reference values depending on age and sex.11,39,40,42 Some of these considerations have been included in guidelines published after the KDOQI (Table 2).
DEFINITIONS
Proteinuria
Under normal conditions, a healthy individual eliminates between 40-80mg of protein/day through urine, about 10-15mg of this is albumin and the rest is made up of Tamm-Horsfall protein43 and small amounts of low-molecular-weight proteins.
In this document, the term proteinuria is used to indicate the presence of concentrations of urine above the reference range. However, there is not a universal cut-off point that defines this range, as this depends on the type of sample used for the measurement (24-hour or random urine sample), the way the results are expressed (in terms of concentration or excretion) or the population being assessed (adults or children) (Table 3).
When a random urine sample is used, the results must be expressed as the ratio between the urinary concentration of protein and creatinine (Pr/Cr).
Albuminuria
In healthy individuals the excretion of albumin in urine is below 30mg/day.11,34,44,45 In this document the term albuminuria refers to the presence of an albumin excretion above this value. When a random urine sample is used, the results must be expressed as the ratio between the urinary concentration of albumin and creatinine (ACR) and the cut-off points that have the highest international consensus are >2.5mg/mmol or >17mg/g (men) and >3.5mg/mmol or >25mg/g (women). However, some societies recommend using only one criterion. These values were obtained from individuals with insulin-dependant diabetes46,47 and have been applied to the rest of the population.48
The values that define microalbuminuria and macroalbuminuria vary depending on the clinical guidelines consulted (Table 4). Both terms, despite being widely used, can give rise to confusion and should therefore be abandoned.49
Under normal conditions the concentration of albumin represents only a small part of the concentration of protein in urine. As the concentration of protein increases so does the proportion of albumin. This ranges between 5% and 70% for Pr/Cr values <2.5 and >90mg/mmol, respectively.50,51 Due to the varying relationship between both measurements, it is not advisable to use conversion factors from ACR to Pr/Cr and viceversa.11
TYPES OF PROTEINURIA
Increased urinary concentrations of protein may be a result of different aetiopathogenic mechanisms,52 and each of them is associated with a type of proteinuria with specific quantitative and qualitative characteristics.
Albumin is the most abundant protein in urine in CKD due to DM, glomerular disease or ATH, which are the main causes of CKD in adults. This is due to an abnormal filtration process, whether structural damage or an alteration in the electrical charges of the glomerular basement membrane.
The presence of low-molecular-weight proteins in urine (β2-microglobulin, α1-microglobulin, retinol-binding protein, etc.) shows the existence of tubulo-interstitial disease. This type of proteinuria is due to an impaired renal tubular reabsorption as a result of congenital structural or functional defects, which are the most frequent causes of CKD in children.
Another type of proteinuria that must be mentioned is orthostatic or postural proteinuria, which only appears when the patient is in the supine position and disappears in the upright position. This mainly affects children and teenagers and tends to disappear when they reach adulthood. Its value is normally below 1g/m2/day and is caused by glomerular haemodynamic abnormalities.53,54
METHODOLOGICAL CONSIDERATIONS IN THE ASSESSMENT OF PROTEINURIA
Pre-analytical conditions
Patients
The presence of fever, stressful situations or performing intense physical exercise55 may cause proteinuria to rise temporarily. This usually reverts back to normal levels after a few days, once the triggering factor disappears. Urinary tract infections or menstruation can result in false positives. For this reason, it is recommended to avoid collecting a urine sample to assess proteinuria in these circumstances.
Sampling procedure
As proteins are removed at a varying rate throughout the day, as a result of factors such as level of hydration, physical activity or protein intake, the 24-hour urine sample has been considered as the reference sample for measuring proteinuria. However, problems associated with collecting a 24-hour urine sample have led researchers to look for alternatives such as first morning urine or random urine samples, expressing the results in terms of concentration or even urinary concentration of creatinine in order to remove the variations depending on the level of hydration. The biological variability must be known to be able to decide which type of sampling procedure is the most appropriate for screening and monitoring proteinuria and assessing the clinical significance of a change.
The studies that have assessed the suitability of Pr/Cr in random urine samples as an alternative to protein excretion in 24-hour urine samples56-60 agree that there is good correlation and agreement between both values, even between samples from individuals with different levels of kidney function impairment61,62 and for a wide range of proteinuria values.63,64 However, correlation as well as agreement worsen when proteinuria is in the nephrotic range (>3.5g/1.73m2/day).64,65 When Pr/Cr is expressed in mg/mg, the quantitative value obtained is approximately the same as that obtained for an excretion of protein expressed in g/day. If Pr/Cr is expressed in mg/mmol, the excretion in 24-hour urine is approximately 10 times this value, considering an average creatinine excretion of 10mmol/day.36
Likewise, the studies that have assessed which is the most appropriate type of sampling procedure for measuring albumin in urine (first morning urine or random urine sample as an alternative to the 24-hour urine sample) and the best way to express the results (urinary concentration of albumin compared to ACR) have found greater agreement with first morning urine compared to second or random urine sample.66,67 They also found a lower intraindividual variability for this type of sample when expressed as ACR. As a consequence, first morning urine is considered the most appropriate sample for screening and monitoring albuminuria. The results should be expressed as ACR (mg/mmol, mg/g) rather than as a concentration value (mg/L).
Conservation
The urine sample remains stable for 7 days at 2-8ºC.49,68 If it has to be frozen, it must be done at a temperature of ≤-70ºC. Lower values, especially at -20ºC, cause the albumin concentration to drop. This especially affects urine samples with albumin values below 300 mg/L.69-72 The sample must be thawed at room temperature and homogenised before measuring it, to dissolve the precipitates that may have formed as well as any albumin absorbed by the container. It is not well understood what effect freezing and thawing has on different molecular forms.
Before freezing and analysing the sample, the urine must be visually inspected to check for the presence of precipitates. These must be eliminated by centrifugation.
If for some reason a 24-hour urine sample is needed, the urine must be kept refrigerated. It is not necessary to add any type of preservative.
Methods for assessing proteinuria
Screening methods
Reagent strips for protein screening
This is a strip of paper impregnated with tetrabromophenol blue buffered at pH 3.0, and68 its colour changes when it comes in contact with the proteins of the sample. The intensity of the colour varies according to the concentration of protein. The result is interpreted by visually comparing the colour obtained with a chromatic scale, and it is translated into values that oscillate from negative to a “+” scale, according to the different concentration values. The scale varies depending on the manufacturer of the strips. Using automated readers reduces the possibility of error and the interpersonal variability when interpreting the results.73 Proteinuria is considered to exist when the colour changes by “1+” or higher. For the majority of manufacturers this corresponds to a concentration of between 150 and 300mg/L.68 The reagent strips are especially sensitive to proteins with a negative charge, such as albumin, and less sensitive to globulins and low-molecular-weight proteins. The most significant limitations of these measuring systems are: inability to detect concentrations below 300 mg/L, false negatives in diluted urine and false positives in concentrated or alkaline urine, and in the presence of haematuria and coloured components such as bilirubin and drugs (ciprofloxacin, quinine and chloroquine).74
Different studies have compared how precise the diagnosis with reagent strips is against the protein measurement in a 24-hour urine sample in populations with a high prevalence of proteinuria.75-77 The results showed a sensibility and specificity which varied depending on the concentration of protein used as the cut-off point. For this reason, most of the clinical practice guidelines advise against using it as a screening test to detect proteinuria34,35,45 and those that do include it, recommend that a positive result should be confirmed with a quantitative measurement.11,78
In recent years, some manufacturers have incorporated an area in their reagent strips which measures creatinine and expresses the protein to creatinine ratio semi-quantitatively. The results can be read visually or by automated devices. Although the initial results have shown it to be effective in monitoring patients with CKD,79 more studies are needed to evaluate its diagnostic value.
Reagent strips for albumin screening
The semi-quantitative measurement of albumin by reagent strips is based on immunological or non-immunological methods that use a strip of paper coated with a tetrabromo-sulfonephthalein derivative.68 They are able to detect small concentrations of albumin (30-40mg/L). There are also test strips on the market with two reaction areas, one saturated with a high affinity and specificity dye (tetrabromo-sulfonephthalein) for albumin and another area to measure creatinine (based on the peroxidase-like activity of a copper-creatinine complex). These strips provide semi-quantitative estimates of the albumin-creatinine ratio in three categories: <3.4mg/mmol, 3.4-33.9mg/mmol and >33.9mg/mmol. These devices have been recently evaluated with results that show a good diagnostic accuracy in the general population as well as in patients with CKD of various origins.80,81
The studies performed to find out the diagnostic accuracy of the specific strips for detecting albumin at concentrations above 30mg/g creatinine have found that they have a low sensibility (from 37% to 83%) and a high specificity (from 93% to 98%). The positive and negative predictive value varies depending on the concentration used to define albuminuria.34
Quantitative methods
Quantitative methods for measuring protein
There are some significant difficulties when measuring protein in urine due to the variability in the make-up and proportion of the different types of protein, as well as the high concentrations of non-protein substances that may interfere with the measurement.
The most used methods are turbidimetric methods (based on the binding of proteins to substances such as trichloroacetic acid or benzethonium chloride) and dye binding methods (Ponceau-S, Coomassie brilliant blue and pyrogallol red-molybdate). Both of the methods have different analytical sensitivity and specificity for the different types of proteins. They strongly react with albumin.82-84
There is currently no measurement procedure or reference material to determine the urinary concentration of protein. This means that there is a lot of variability between the results obtained in different laboratories. This variation has an effect, especially at low concentrations, and decreases at higher concentrations due in part to the higher relative concentration of albumin that they have.
The data from the external quality control programme (FPCQLC) of the Spanish Society of Clinical Biochemistry and Molecular Pathology (SEQC) for 2009 show that turbidimetric methods that use benzethonium chloride (48.5% of laboratories) and pyrogallol red-dye binding (44.9% of laboratories) are the most used methods for measuring protein. The coefficients of variation range between 7.7% and 10.5% (turbidimetric methods) and from 4.5% to 7.7% (pyrogallol red-dye binding) for a concentration range between 0.31 and 1.07g/l.85
Quantitative methods for measuring albumin
The most common methods for measuring albumin levels in urine are the turbidimetric or nephelometric immunoassays with detection limits between 2 and 10mg/L. The antibodies used can be monoclonal or polyclonal with different sensitivities for detecting anomalous albumin or fragments of albumin present in urine. Methods based on high performance liquid chromatography (HPLC) have appeared in recent years. These methods have higher values than immunoassays as they detect non-immunoreactive albumin.
Several external quality control programmes have shown that there are differences in the results obtained by different laboratories and in the units used to express the results.86 This is because there is no reference laboratory test; no international reference material and due to the presence of different molecular forms of albumin both in the urine sample and the calibrators (fragmented molecules, glycosylated molecules and dimeric forms), the presence of degraded albumin or non-antibody-reactive albumin; non-specific binding of albumin to the tubes used to collect the sample, as well as polymerisation and fragmentation that occurs during storage and the freeze/thaw process.87
Most of the manufacturers of products for in vitro diagnosis state that the value assigned to their calibrators is traceable to the certified reference material ERM®-DA470k/IFCC (previously called CRM 470), which is distributed by the Institute for Reference Materials and Measurements of the European Commission. This material, with an albumin concentration of 37.2g/l, is the same as the one used for serum albumin calibration. There are differences between the manufacturers in the protocols for preparing the calibrators, the solvent used, the dilution factor, the plasma or urine matrix, etc. Recently, the Japanese Society of Clinical Chemistry has developed a candidate for a reference material devised from monomeric human albumin with over 97.5% HPLC purity in a buffered and lyophilised aqueous matrix. The Japanese Committee for Clinical Laboratory Standards is currently evaluating it.88 Furthermore, researchers from the Mayo Clinic are working on a method based on liquid chromatography-isotope dilution mass spectrometry (LC-IDMS)89 as a possible reference method candidate.
Specific immunoassays for determining albumin provide a better albumin measurement compared to the protein measurement in laboratory tests. The data for 2009 from the FPCQLC of the SEQC shows that 87.8% of registered laboratories determined albumin in urine using turbidimetric methods compared to 12.1% that used nephelometric methods. The coefficients of variation oscillate between 5.4% and 10.0% (turbidimetric methods) and 6.8% and 15.5% (nephelometric methods) for a concentration range between 260 and 970mg/L.85
FUTURE LINES OF RESEARCH
There was a conference in 2007 organised by the Laboratory Working Group of the National Kidney Disease Education Program (NKDEP) and the International Federation of Clinical Chemistry and Laboratory Medicine (IFCC). The objectives of this conference was to highlight the problems associated with measuring albuminuria and to organise working groups in order to formulate recommendations that could be included in clinical practice guidelines.49 The group of experts believed that the following aspects had to be further investigated in order to standardise the measurement of albumin and how the results are expressed:
1. Pre-analytical requirements regarding the container used to collect the sample; the need to carry out further investigation into biological variability in order to decide when to obtain the sample or the influence of blood, seminal fluid and other physiological contaminants in urine.
2. Clarify the definition of the mesurand and research the molecular forms of albumin in freshly voided urine sample and the level of degradation of albumin depending on the storage conditions.
3. Develop a reference measurement procedure as well as urine albumin and creatinine primary and secondary reference materials with standardised and certified commutability by the Joint Committee for Traceability in Laboratory Medicine (JCTLM).
4. Determine the most appropriate measurement procedure, considering the variation in urinary composition.
5. Define the total acceptable error clinical requirements for measurement procedures, as well as the materials to be used in Quality Control Programmes that allow the different methods to be compared.
6. Assess whether different decision thresholds are needed depending on the sampling procedure, anthropometric characteristics (age, sex or ethnicity) and different population groups (general population or high-risk groups such as DM, hypertension or cardiovascular disease [CVD]).
7. Research on the usefulness of age- and sex-specific equations to convert ACR to an albumin excretion/day value for which a single reference limit may be appropriate.
KEY ASPECTS ON THE EVALUATION OF PROTEINURIA IN CLINICAL PRACTICE GUIDELINES
Different scientific societies have prepared guidelines that include recommendations for evaluating proteinuria in CKD patients. The most important aspects are summarised in Table 5. They are displayed below according to the year of publication.
Target population
All the guidelines agree on the fact that screening for proteinuria must be carried out on individuals with high risk of CKD: DM, hypertension, CVD, GFR below 60ml/min/1.73m2, multi-systemic diseases with possible kidney impairment, over 60 years old, past family history of CKD, or specific ethnic groups with a high prevalence of CKD. There are guidelines with recommendations for specific population groups such as those by the American Diabetes Association (ADA)90 or the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.91
Use of reagent strips for proteinuria detection
Only the KDOQI11 and Welsh Renal NSF78 guidelines state that the use of reagent strips as acceptable for screening for proteinuria. They propose that any result “≥1+” should be confirmed using a quantitative measurement (Pr/Cr or ACR) within the following 3 months. The other guides advise against its use due to its low sensibility and specificity even though there is evidence that a strip test value of “≥1+” can be used to identify patients with a high risk of end-stage CKD and CVD.35
Sampling procedure
All the guidelines agree that the most appropriate sample is the 24-hour urine specimen; although collection problems make its use difficult in clinical practice. For that reason, they recommend using a urine sample, preferably first-morning urine; although a random urine sample is also acceptable.
Biological measurement that must be determined (protein or albumin)
There is general consensus between the guidelines that determining Pr/Cr or ACR in a random urine sample must replace measuring protein or albumin in 24-hour urine. Furthermore, all the guidelines agree that analysing protein in urine is not sufficiently sensitive to identify the presence of incipient diabetic nephropathy. They suggest determining albumin expressed as ACR once a year. In other circumstance, the guidelines vary on recommending using ACR or Pr/Cr. Thus, KDOQI, KDIGO, ADA, NICE, JNC-7 and SEN-semFYC recommend using ACR while PARADE (children), CARI, SIGN, UK Guidelines, Welsh Renal NSF and CSN recommend using Pr/Cr.
Cut-off values
Table 5 shows reference ranges and values considered as pathological by each of the guidelines.
Units used to express the results
The PARADE (children), KDOQI, JNC-7, CARI, KDIGO, ADA and SEN-semFYC guidelines recommend using conventional units (mg/g), the rest of the guidelines suggest using International System of Units (mg/mmol).
Recommendations for children
Only the KDOQI, Welsh Renal NSF, PARADE (children) and CARI guidelines include children-specific recommendations. All the guidelines agree that Pr/Cr must be used to detect and monitor proteinuria in children, except in children with postpuberal onset of DM with more than 5 years of duration. In these cases, the use of ACR is recommended in the same way as in adults.
They recommend this because of the low prevalence of CKD due to DM or hypertension in children compared to diseases linked to urinary tract abnormalities or congenital tubular disorders, which are characterised by the elimination of low-molecular-weight proteins.
RECOMMENDATIONS
Assessment of proteinuria and/or albuminuria
1. The presence of high urinary concentrations of protein or albumin on two or more occasions during a period of 3 or more months is a sign of kidney damage. The diagnosis of CKD is based on signs of kidney damage and the GFR.
2. The estimation of the glomerular filtration rate should be measured together with urinary concentration of protein and/or albumin in individuals at risk of developing CKD.
3. The detection and monitoring of protein and/or albumin in urine must be based on a quantitative measurement.
4. When detecting, staging and monitoring CKD, the presence of proteinuria must be assessed:
a. In adults proteinuria must be assessed by measuring the albumin-creatinine ratio in a urine sample.
Albuminuria is a more sensitive marker than proteinuria in CKD due to DM, hypertension or glomerular disease, which are responsible for most of CKD cases in adults.
If a laboratory decides to use the protein-creatinine ratio as an initial quantitative test, they should also measure the albumin-creatinine ratio if the result is within the reference range.
b. In children without DM, proteinuria must be assessed using the protein-creatinine ratio in a urine sample.
There is a much lower prevalence of CKD due to DM or hypertension in children than in adults; however, there is a high prevalence of CKD due to urinary tract defects or congenital tubular disorders that may cause non-glomerular proteinuria.
c. In children with post-pubescent onset of DM with more than 5 years of duration, the albumin-creatinine ratio must be measured in a urine sample. In other circumstances, the same recommendation for children without DM must be followed.
5. “Clinically significant proteinuria” should be considered:
a. In individuals without DM: protein excretion >0.5g/day, protein-creatinine ratio in a urine sample >50mg/mmol or albumin-creatinine ratio in a urine sample >30mg/mmol.
b. In individuals with DM: albumin-creatinine ratio in a urine sample >2.5mg/mmol or 17mg/g (men) and >3.5mg/mmol or >25mg/g (women).
This recommendation is based on the criteria established by the NICE guidelines. These criteria are an indication to start ACEI or ARB treatment.
6. It is possible to monitor individuals with CKD and clinically significant proteinuria using the protein-creatinine ratio.
7. Given that the proportion of albumin in urine with regard to the concentration of protein varies, the use of conversion factors from creatinine-albumin ratio to protein-creatinine ratio and vice versa is not recommended.
Sampling procedure
8. It is not necessary to collect a 24-hour urine sample to detect and monitor proteinuria and/or albuminuria.
9. First-morning urine is the most appropriate sample for detecting and monitoring proteinuria and/or albuminuria. It is the sample with the lowest biological variability and has the best correlation with protein and/or albumin excretion in 24-hour urine. The presence of orthostatic proteinuria can also be excluded with this sample. If this is not available, a random sample is acceptable.
10. The most appropriate sample to assess proteinuria and/or albuminuria is freshly voided urine. If the samples are not processed on the same day as they are taken, they should be stored for up to 7 days at temperatures between 2 ºC and 8 ºC. If the samples have to be frozen, this should be done at temperatures ≤-70ºC and they should be thawed at room temperature. Any cloudiness should be removed by centrifugation
Clinical laboratory reports
11. The urinary concentration of protein or albumin must always be compared against the concentration of creatinine to reduce the effect that hydration may have on the results.
12. The results can be expressed in mg/g or mg/mmol depending on the type of units used in each laboratory, although the use of International System of Units is recommended (mg/mmol).
13. The terms microalbuminuria and macroalbuminuria should no longer be used and should be replaced by albuminuria.
Members of the SEQC Commissions
Kidney function: J. Ballarín Castán*, P. Bermejo López-Muñiz, J. Bover Sanjuán*, A. Cases Amenós*, M.J. Díez de los Ríos Carrasco, S. Gràcia García, J.A. Jiménez García, C. Macías Blanco, R. Martínez López, R. Montañés Bermúdez (President), G. Ruiz Martín, L.J. Morales García, J. Ruiz Altarejos, S. Sanz Hernández, S. Ventura Pedret.
*Associate members.
Proteins: C. Bermudo Guitarte, M.C. Cárdenas Fernández, M. Cortés Rius, M. Fernández García, M. García Montes*, C. Martínez-Brú (President), D. Pérez Surribas, T. Rodríguez González, C. Valdecabres Ortiz, J.A. Viedma Contreras, E. Zapico Muñiz.
Members of the S.E.N. who collaborated in the revision of the document: R. Alcázar Arroyo, J.L. Górriz Teruel, F. Rivera Hernández.
Table 1. Classification of chronic kidney disease stages according to the KDOQI guidelines of the National Kidney Foundation (2002)
Table 2. Classification chronic kidney disease stages according to the UK Renal Association (2007), NICE (2008) and SIGN (2008) guidelines
Table 3. Values used to define proteinuria according to the different scientific societies
Table 4. Values used to define albuminuria according to the different scientific societies
Table 5. Summary of the guidelines
Guidelines consulted while preparing this document