A 12-hour training program was delivered to the professionals of a nephrology department. Contents of the course were about difficult communication skills in health care interactions. Counselling was the relational methodology instructed. The objective was to assess changes in attitudes in relation with bioethics principles and knowledge. Variables were measured before and after the training program. Sample was composed by 76 professionals (57% nurses, 26% auxiliary nurses y 17% nephrologists) for knowledge and 27 professionals for variable attitudes. Considering the total sample, results show changes in implication with bioethics principles (p <0.05) and knowledge (p <0.001). There are differences related to the kind of profession. Nurses benefit more from the training program attending in the variable knowledge (p <0.001).
Los profesionales sanitarios del servicio de nefrología de un hospital de tercer nivel recibieron entrenamiento en comunicación terapéutica mediante un curso de 12 horas centrado en el instrumento terapéutico conocido como counselling. El objetivo fue evaluar cambios en actitudes en relación con los principios bioéticos y en conocimientos sobre comunicación y gestión emocional. Las variables evaluadas se midieron antes y después de la implantación del curso. La muestra estaba formada por 76 profesionales (un 57% profesionales de enfermería, un 26% auxiliares y un 17% médicos especialistas en nefrología) para la variable conocimientos y por 27 profesionales para la variable de actitudes. Considerando la muestra total, en los resultados se observan cambios en implicación con los principios bioéticos (p <0,05) y conocimientos (p <0,001). Se observan diferencias en función de la profesión y son los profesionales de enfermería quienes más se benefician del curso en el área de conocimientos (p <0,001).
INTRODUCTION
Health professionals that attend to patients with renal diseases frequently find themselves in situations of very high stress derived from the uncertainty associated with caring for patients with progressive chronic diseases.1 Several different studies have shown that patients on haemodialysis suffer from very high rates of depression,2-6 which can influence the level of compliance with treatment plans and relationships with health professionals.7-9 Authors such as Cukor, Cohen, Peterson, and Kimmel10 consider the renal patient as a paradigm of chronic patients from a psychological perspective. These are complex patients, with multiple associated comorbidities and, as such, the psychological need for adaptation both to the disease itself and to the treatment methods that imply a high impact on quality of life.11,12 To suffer from a renal disease usually implies a serious challenge to a person’s emotional balance, since the patient must deal with multiple issues and threats throughout the diagnosis and treatment periods. A poor state of health creates a personal crisis in which the patient suffers from very intense emotional reactions and requires specific resources in order to recover overall balance. Inevitably, all this affects the interactions between patients and health professionals.
Although proper use of medical and biological technology and procedures is of great importance, they are insufficient if we are to offer an effective and efficient response to the personal crisis this causes the patient and his/her family.13 As Chochinov stated,14health care focused on maintaining patient dignity, improving communication and developing an emotional approach, has a significant influence on the patient’s experience. This framework can be applied in clinical practice as well as in the training of multidisciplinary teams, paramedics, and medical students of all specialties.
Difficult communication in situations of high emotional intensity and a lack of professional resources have a major impact on the quality of health care provided.15,16 The medical literature indicates that the communicative relationship between a nephrologist and the patient should promote a joint decision-making process.17-19 In many occasions, these patients must make very difficult decisions, such as starting a chronic dialysis programme, halting a treatment plan, or composing an advance health care directive.20-22 In all of these cases, the attending doctor and nursing staff can aid in resolving conflicts, offering information tailored to the patient’s needs, and establishing the patient’s general expectations and expected quality of life so that all decisions are made voluntarily and using all available information. For this communication process to be effective, health care staff must have, in addition to good communication skills, training in the attitudes and value systems necessary to create an environment of trust and understanding that facilitates decision-making.23
The training of health professionals in communication skills is necessary for both directly and indirectly improving the quality of life of renal patients and facilitating compliance with treatment plans and the process of adapting to the disease.24-27 It also provides a fundamental source of support to doctors and nurses, as improving the level of care given to the patients and their families usually aids in preventing work-related stress.28-30
Within the nephrology department at an acute care hospital, in which the workload can be high and hectic, patients may experience even more intense levels of suffering caused by their conditions and may react to health care professionals with aggressiveness or be excessively demanding.31-33 Proper training in communication skills and techniques for handling strong emotions aids in minimising the impacts associated with health care.
Generally, health care professionals have not properly developed these skills in chronic patient care due to the lack of training and general ignorance regarding the need for this type of training.34 Most assume (erroneously) that good intentions are sufficient to guarantee proper communication. Hospital infrastructure, workload, and a procedure-focused health system can all decrease the quality of health care due to a shortage of good communication skills and emotional competency.35 Counselling training is not a normal component of medical education, but studies have shown that this model of communication, and treatment technique, facilitates patient adaptation to the disease and reduces the level of conflict and emotional stress, both in patients and health care workers.36,37
Clinical work in a specialised hospital implies the need for continuous interaction, and thus, communication among health professionals. Obviously, we cannot expect to observe significant changes in their communication process if training and interaction processes are not included as an independent variable. Health care is provided under a chain of command, and this chain is only as strong as its weakest link. As such, to not take into consideration the professional development of certain components of this chain, such as nursing assistants, puts the work of the entire team in jeopardy. Certain concepts and tools, such as how to manage patient aggressiveness as an adaptive emotional reaction to hospitalisation, must be taught universally, since they affect the objectives and decisions made by all health professionals. A team that does not receive common training in fundamental areas (communication and values) will only achieve partial objectives (such as increasing dialysis doses), but not integrated objectives regarding the biological and psychosocial well being of the patients and their families. A lack of a formal environment for mutual understanding and communication can cause differences in language, concepts, and perspectives from other disciplines and co-workers may seem inefficient, ineffective, or even completely opposed to the common task that brings them together.
Another fundamental aspect that must be considered is that proper communication regarding treatment does not come naturally. We all have acquired attitudes and abilities in our processes of personal and professional growth; even so, we are not always conscious that some learned behaviours create a negative atmosphere for communication, especially because hospital employees find it difficult to give constructive criticism about their own or other professionals’ style of communication. We need platforms for mutual understanding in which an environment is created to facilitate the detection and amelioration of the automated communication patterns that we are not always aware of.
Keeping in mind all of the aforementioned variables, the administration of the nephrology department at our hospital facilitated and promoted the development of a training course for doctors, nurses, and other hospital staff with the objective of improving attitudes, abilities, and understanding within the context of communication among health care professionals and patients.
The hypothesis of our study is that a formal training course in communication directed towards the entire multidisciplinary work team (doctors and nursing staff) within a single department will produce changes in both attitudes and knowledge (considered as dependent variables).
MATERIAL AND METHODS
Study subjects
Our study involved a pretest-posttest design with no control group. The initial sample was composed of a total of 76 health professionals from the nephrology department at a tertiary hospital. The study subjects accepted the proposal of receiving training in difficult communication and decision-making within the framework of continued education established by the hospital. The study sample represented 86% of the department employees, and the reasons for abstaining from the study of the other 14% were unknown. Of the participants, 57% were nurses (43), 26% were nursing assistants (20), and 17% were nephrologists (13). By category, the study subjects represented 93% of nurses, 95% of nursing assistants, and 61% of specialist doctors. By age, 38% of study subjects were between 25 and 35 years old, 37% were between 36 and 50 years old, 22% were older than 50, and 3% were younger than 25. We were also interested in the amount of experience (how many years) that each participant had with this type of chronic patient: 50% had more than 10 years of experience in working with renal patients, 16% had between 6 and 10 years experience, 26% had between 1 and 5 years experience, and 8% had less than one year of experience. A large majority of the study group (89.5%) were women. Finally, we would like to point out that the directors of the nursing staff along with the head of department actively promoted this training course and participated in it.
Tools
We evaluated the participants using a questionnaire that was put together ad hoc on the following areas (the number in parentheses expresses the Cronbach’s alpha coefficient for the pretest evaluation):
1. Attitudes regarding the four basic bioethical principles (nonmaleficence, justice, respect for autonomy, and beneficence):
a) Importance of the bioethical principles in hospital work (α=.76): made up of four items with a Likert scale ranging between 1 (unimportant) and 10 (extremely important).
b) Personal compliance with the bioethical principles in my daily work (α=.89): made up of four items with a Likert scale ranging between 1 (no compliance) and 10 (total compliance).
2. Knowledge (α=.85): made up of 15 items with four possible responses each, and no penalty given for wrong answers. This section was composed of two categories (difficult communication and managing emotions).
Building the questionnaire:
The creation of the initial version of the questionnaire was supported by a basic literature review regarding the training of health professionals in communication skills. Through this review of previous publications, we identified two relevant areas of evaluation for the study: attitudes (importance of bioethical principles and compliance with them) and knowledge (both in difficult communication and managing emotions). We developed 23 possible items for assessing these two areas. In order to evaluate the validity of the content and face validity of each item, comprehension by the participant, and the relevance of each item for Counselling training, we sent the questionnaire to a group of expert faculty members (n=10) along with a standardised evaluation form. The standardised evaluation facilitated the assessment of the comprehension and relevance of each point. We established criteria for revising or eliminating each item based on the percentage of agreement between judges (the expert faculty) in the evaluation of the comprehension and relevance of each item. If inter-judge accordance was 80% or higher, the item was kept in the survey. If the value was below 50%, it was eliminated from the questionnaire. If the value was between 50% and 80%, the item was scrutinised and revised using the observations and suggestions provided by the reviewers. None of the items were eliminated from the initial list. We took into consideration the observations and suggestions provided by the judges when revising the form and producing the final document.
Course content
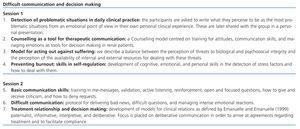
The course content considered various health care situations (chronic/acute, exacerbations, terminal-stage patients, etc.) that present themselves to health professionals and their patients in a hospital department that treats a wide range of complex cases. This content is summarised in Table 1.
The course was focused on using Counselling as a therapeutic tool. A good communication model is needed that facilitates the patient-health care professional relationship and the decision-making process in order to produce effective clinical practice in nephrology. This is especially important when facing scenarios as severe as starting renal replacement therapy or halting it. Counselling is a therapeutic tool that has proven to be very useful in health care.38,39 It consists of an interactive and relational process that develops between the patient and his/her caregivers that facilitates psychological adaptation to the disease, avoids adverse emotional states, promotes self-regulation by the health care professional, and motivates to pursue a change for the better.40
Procedure
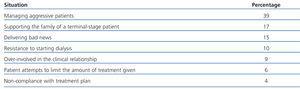
A 12-hour interdisciplinary course was organised on 5 separate occasions during 2007. The course was divided into two sessions that were held on two consecutive days during mornings or afternoons. The hospital department for continued training collaborated directly with the design and execution of the course. We also procured that all hospital staff were released for training sessions without having to make up for missed time. This was done in such a manner as to include the greatest possible number of participants without causing notable losses in productivity. At the start of each course, we asked all participants to list their three most feared situations, or those that produced the greatest amount of difficulty from an emotional standpoint. The main situations that were identified by the study group are listed in Table 2 (there was no need to categorise them).
The course was taught by a team of four hospital psychologists with experience in Counselling training for health professionals. Each course was led by a subgroup of two psychologists. The maximum number of participants was 20 per course. We used a methodology of active participation to support interactive learning and to act out most of the difficult situations identified using role-playing. This teaching method allows for the students to identify key aspects of communication, such as attitudes, skills, and value systems. Using these shared observations, we provided key techniques for managing personal relationships that were revisited in a role-playing context in order to observe student assimilation of the techniques. The different scenarios that were worked through included all the situations that may occur in nephrology (hospital/home dialysis, outpatient/hospitalised patients). All study subjects that participated in the different courses were evaluated using the ad hoc questionnaire before and after the training course.
Statistical analysis
We used SPSS software for Windows (version 17.0) for all statistical analyses. We produced descriptive statistics of sample and point scores from the before and after studies. We tested the reliability of the data using the Cronbach’s alpha coefficient for analysing the internal consistency of the questionnaire areas described in the “tools” section. We used non-parametric tests (Wilcoxon’s test) to compare the before and after scores in attitudes and knowledge in the overall study group and by type of profession (doctors, nurses, and nursing assistants). We used the Spearman’s correlation coefficient to analyse the differences in scores for “importance of bioethical principles,” and “compliance with bioethical principles” between surveys taken before and after the training course.
RESULTS
Sample characteristics
As we mentioned in the “study subjects” section, the total sample size was 76 health professionals from the nephrology department in a tertiary hospital. All participants filled out the knowledge questionnaire, but only 27 (18 nurses, five nursing assistants, and four doctors) did so for the attitudes questionnaire in both pre- and post-training course surveys. For this reason, n is greater for knowledge than for the other variables evaluated.
Training course results
Comparison of means from pre- and post-training surveys
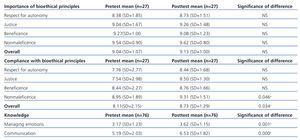
1. Importance of bioethical principles. There were no differences observed in the importance given to bioethical principles, with very high mean values in before and after surveys.
2. Compliance with the bioethical principles. We observed significant differences in the global score (P=.034) and the nonmaleficence category (P=.046), with higher values produced in the post-training survey, but no differences were observed for respect for autonomy, justice, and beneficence.
3. Knowledge. All differences between the two surveys (managing emotions and difficult communication) were statistically significant (P<.001)with higher scores obtained after the training course. This indicates that attending the training course produces significant positive effects in acquiring knowledge.
The statistical results from comparing means are summarised in Table 3.
Correlations between importance of and compliance with the bioethical principles in health care practice
We observed significant direct correlations between all study variables, indicating that when the four primary bioethical principles (nonmaleficence, justice, respect for autonomy, and beneficence) and the values that they imply are given importance, health professionals also tend to comply with them. This trend was observed in both the pre- and post- training surveys.
The results for data correlations are summarised in Table 4.
Programme results by type of health profession
Taking into consideration that each profession is based on a distinct set of abilities and skills that are specialised for the work activity to be carried out, we set out to compare the effects of the training programme (pretest-posttest) by type of profession. We used non-parametric tests (Wilcoxon’s test) for this analysis. When dividing the study sample into professional categories, we observed statistically significant differences between the two surveys in nurses. The variables in which we observed these differences were acquired knowledge (P<.001) and difficult communication (P<.001). We observed no significant differences in attitudes related to the bioethical principles.
DISCUSSION
The most important findings of this study were:
1. The majority of health care professionals surveyed had a high level of familiarity with the importance of bioethical principles. The more they knew, the more they complied with them.
2. Participation in an interdisciplinary training course in Counselling and emotional support improved the compliance with the bioethical principles, especially in the nonmaleficence category.
3. The group of nurses was the only one that significantly improved in the managing emotions and difficult communication categories.
Our study group was relatively young (88% of participants were younger than 50 years), but with extensive experience in caring for renal patients: 50% of the sample indicated over 10 years of experience. As we have described earlier in greater detail,41 a high level of quality in nephrology health care requires the development of an interdisciplinary and experienced team to properly attend to the physical and emotional needs of their patients. One way to attend to the multi-dimensional nature of renal patients is by promoting training courses in communication skills and managing emotions.
The health care professionals evaluated in our study indicated that the most difficult situations that they face in normal clinical practice are those that have to do with communication with patients (for example, dealing with an aggressive patient, resistance to dialysis, etc.) and the family (for example, giving support to the family of a terminal-stage patient). In previous studies42 carried out with similar study subjects, the most feared situations were communicating with patients (51.7%) and their families (39.3%).
We observed significant differences in all areas of acquired knowledge when evaluating all of the professions in the sample group. This is in line with some teaching experiences43 involving groups of doctors and nurses or students which have come to the conclusion that mixed training in communication dealing with certain emotional reactions provides the participants with increased knowledge of daily clinical practice.
With regard to the attitudes of the participants, we did not observe changes in the importance of bioethical principles (the rate was very high from the beginning and remained so after the training course), but survey results did significantly improve in the section on the compliance with these principles (both in the global score and in the nonmaleficence section). This makes sense since one of the principle components of the course is the development of moral responsibility in the face of suffering, which is reflected in the nonmaleficence principle. A conceptual understanding of these values does not necessarily conduce to complying with them; however, in this study, it appears that an initially high conceptual value given to bioethical principles, which did not change after the training course, provides a foundation for the development of personal compliance with them through participation in the training course. To this end, the atmosphere created in the training course was not one of indifference, but rather of a dynamic, but direct, approach of how these values are incorporated into everyday clinical practice. Thus the training was not simply about giving information, but also upholding values. In other words, seeing the connection between the common clinical situations and the basic values previously mentioned can increase the interest in applying them in the clinical setting (for example, if as a nephrologist, I am conscious of the fact that by effectively managing the visits time I am working towards the principle of justice, I will put more energy towards this pursuit). The ability to see everyday situations in terms of personal values can increase the personal compliance with these values and improve treatment results.
By breaking up the results of our study into different professions, we observe that nurses obtained the greatest benefit from this type of training course in comparison to doctors and nursing assistants. Probably, one of the most important factors involved in this disparity is the smaller sample size in the other two groups, especially in the attitudes section, in which an important part of the sample was lost, since not all participants filled out the questionnaire completely. This is probably due to the fact that the evaluation form did not consist of one single document, and several participants believed that they had finished the survey after completing only the section on knowledge. However, over 90% of the nursing staff and 61% of doctors participated in the training course. These differences may have been due to the lower level of interest held by nephrologists in these matters, or simply due to the higher workload of hospital doctors, making free time for further training very scarce. Several studies have analysed the same differences found in our study variables among the different types of health professions. One study from Norway that was performed in nursing homes concluded that, when making health decisions at the end of a patient’s life, doctors tended to guide themselves more by the principles of beneficence and nonmaleficence, whereas nurses did so following the principle of respect for autonomy, even in patients with communication problems and dementia.44 Another study involving 1910 health professionals from 14 public hospitals in Hong Kong showed that different sectors of health services (doctors and nurses) and previous experience in the clinical setting were independent variables for predicting the perception of ethical dilemmas with terminal-stage patients and difficult communication, among others.45 In intensive care units and with trauma patients, nurses and doctors have also professed different perceptions regarding whether to apply life support techniques (such as cardiopulmonary resuscitation).46-48 Most studies have concluded that nurse practitioners believe that cardiopulmonary resuscitation is a procedure that causes ethical dilemmas and anxiety if there is no consensus in the medical team about the prognosis of the patient. However, both doctors and nurses coincide that including the patient’s family in making decisions with a high emotional impact is very important.49
Traditionally, this type of training course was designed to provide nurses with resources and tools for handling emotional situations.50 Our study results support the validity of providing training in communication skills and handling emotions, as other authors have shown51 or sought52 in order to face the complex situations that arise in clinical practice.
In spite of producing interesting results, this study did have certain limitations. Methodologically, the lack of some type of follow-up or control group made it difficult to extract conclusions regarding the stability of the changes produced by the training course, or to attribute causality of the results observed to the programme alone. We also lost an important section of the sample in some parts of the questionnaire, which has limited the power of the statistical methods used to analyse the data. We would also like to incorporate into the next version of the training course another independent variable: level of satisfaction with teamwork. We believe that a secondary benefit derived from this type of interdisciplinary course is improved personal relations amongst the hospital staff.
This type of continued training is a good stimulus for the different approaches to providing health care to renal patients and their families. Studies such as ours are needed in order to continue revealing to the nephrological community the importance of a biopsychosocial decision-making approach to the disease and the possible suffering of the patient.53-55 To conclude, it is important to point out the relevance of working on value systems based on modern bioethical principles within the training given in personal relations to health care workers that treat renal patients and share in making complicated life decisions.
Table 1. Content of the Counselling course for the nephrology department
Table 2. Difficult situations faced by health professionals in daily practice
Table 3. Comparison of before and after mean values for the variables regarding importance of bioethical principles, compliance with the bioethical principles, and knowledge
Table 4. Correlation between the importance and compliance with the bioethical principles (n=27)