Background and objective: Most hypertensive patients do not reach target blood pressure (BP), especially if they are diabetic. The objective of the study is to assess the percentage of tight BP control, defined as BP<130/80mm Hg and identify factors associated with it in diabetic type 2 (DM2) patients treated in nephrology units. Patients and methods: Observational and cross-sectional study; we included 526 patients with DM2 and arterial hypertension (AHT). We collected data on: demographics, anthropometrics, harmful habits, history of cardiovascular disease (CVD), blood pressure, kidney function, glycaemic control, lipid profile, and drug treatment, among others. Results: The mean age (SD) was 66 (10.6) years, 61% were male, 12.8% were smokers, 39.4% had a history of CVD, 72% had hypercholesterolemia, and 44% were obese. Seventeen point five percent of patients had tight BP control (<130/80mm Hg) (95% confidence interval [CI]:14.3-21.0), while 36.9% had BP below 140/85mm Hg. Seventy-one percent of patients were prescribed two or more anti-hypertensive treatments. Several factors are associated with tight BP control not being achieved, and the logistic regression analysis revealed that LDL cholesterol levels were significantly associated (odds ratio [OR] 0.55; 95% CI:0.41-0.75 for one standard deviation increase). Conclusions: Of the DM2 patients that attended the nephrology units, less than 20% achieved a tight BP control. Cholesterol levels seem to be the main factor associated with unsatisfactory BP control within our study population.
Fundamento y objetivo: La mayoría de pacientes hipaertensos no alcanza los objetivos de control de la presión arterial (PA), especialmente si son diabéticos. El objetivo del estudio fue evaluar el porcentaje de control estricto de la PA definida como PA <130/80 mmHg e identificar factores asociados al mismo en pacientes diabéticos tipo 2 (DM2) tratados en unidades de nefrología. Pacientes y método: Estudio observacional y transversal, en el que se incluyeron 526 pacientes con DM2 e hipertensión arterial (HTA). Se recogieron datos demográficos, antropométricos, hábitos tóxicos, antecedentes de enfermedad cardiovascular (ECV), medidas de PA, función renal, control glicémico, perfil lipídico y tratamiento farmacológico, entre otros. Resultados: La edad media (DE) fue de 66 (10,6) años, con un 61% de hombres, un 12,8% de fumadores, un 39,4% con antecedentes de ECV, un 72% con hipercolesterolemia, y 44% con obesidad. El porcentaje de control estricto de la PA (<130/80 mmHg) fue del 17,5% (intervalo de confianza [IC] 95%: 14,3-21,0), mientras que un 36,9% tenían la PA por debajo de 140/85 mmHg. Un 71,1% de pacientes recibía dos o más tratamientos antihipertensivos. Diversos factores se asociaron con falta de control estricto de la PA, de los cuales, tras análisis de regresión logística, destacaban los valores de colesterol LDL (odds ratio [OR] 0,55; IC 95%: 0,41-0,75 para un aumento de 1 DE). Conclusiones: En pacientes con DM2 atendidos en unidades de nefrología, el porcentaje del control estricto de la PA es inferior al 20% en la clínica. Los niveles de colesterol parece el principal factor asociado con el control insuficiente de PA en la población estudiada.
INTRODUCTION
The relationship between arterial hypertension (AHT) and diabetes mellitus type 2 (DM2) is well known. Although the prevalence of AHT in the general population is around 30%, it is between 51% and 93% in DM2 subjects, depending on whether the patient suffers from a related kidney disease.1 In contrast, it is also known that patients with AHT are 2.4 times more likely to develop DM2 than normotensive subjects.2 The cardiovascular risk associated with AHT or DM2 is widely recognised, and it is estimated that in general, 68% of coronary events are due to one of the conditions being present.3 In a classic study, Haffner et al showed that DM2 patients that had not suffered any vascular event had a similar risk to presenting one within 7 years as non-diabetic patients that had already suffered one, be it a coronary, cerebral or peripheral vascular event.4 As such, in practice, DM2 is considered as a coronary equivalent for assessing the risk of future events, as confirmed by longer-term follow-up studies.5 Furthermore, it is understood that AHT + DM2 involves an additional increased risk of vascular complications, as shown in a 28-year follow-up study which reported that men with AHT and DM2 have a 66% higher risk of suffering a stroke or heart attack than men who only have AHT.6
There are several studies that have compared the benefits associated with reducing blood pressure (BP) to prevent cardiovascular events in DM2 patients and non-diabetic patients.7 One of the first studies was the UKPDS38, published in 1998, which revealed that tight BP control in diabetic patients significantly reduced the risk of microvascular complications and stroke during an 8.4-year follow-up.8 More importance has been given to controlling AHT in DM2 patients since the need to maintain BP control throughout patient follow-up was documented by Holman et al.9 These authors conducted a 10-year follow-up of the patients that underwent the UKPDS38 study, observing that the differences in BP between the two groups disappeared 2 years after the study was completed, showing that the benefit of lower risk was lost over time.
Despite these observations, optimal BP control is achieved in less than 30% of AHT patients, even when more than 60% of these patients are prescribed anti-hypertensive treatment.7,10 These optimal control percentages are even lower when examining several risk populations. BP control for DM2 patients (130/85mm Hg in studies) is around 13%, both in primary care11 and hypertension unit.12 Observational studies and clinical trials have proven that poor systolic BP control (SBP) is the main reason for low AHT control percentages.7,13 This is especially relevant for the diabetic population, which usually have a high pulse pressure.14 We are yet to fully understand what causes poor BP control in the hypertensive population. There may in fact be several causes which almost certainly involve patient- (compliance, comorbidities) doctor- (attitude), blood pressure-, and environment- (primary care, hospital) related factors, among others. Furthermore, most studies do not examine all possible aspects that can affect BP control, but only specific aspects.
The main objective of this study is to estimate the prevalence of tight BP control (BP<130/80mm Hg) for patients with AHT and DM2, who attended nephrology units in Spanish hospitals. Secondary objectives are to describe the frequency in which tight control is not achieved due to poor systolic or diastolic blood pressure (DBP) control, or a poor control of both. We also aim to investigate the factors associated with good BP control.
PATIENTS AND METHOD
Study design
We invited 60 nephrologists throughout Spain to participate in our multi-centre, observational, cross-sectional study. We informed them of the objectives and the study justification, and how they could register and participate in the study (via the especially designed web site). We asked doctors to choose the first 10 patients that met the selection criteria (see “Participants”) and visited their unit consecutively, and who agreed to participate in the study. Being a cross-sectional study, the most recent patient data were collected, and we did not perform any type of prospective follow-up. The study was monitored online to ensure that the correct data was included.
Participants
We included patients with AHT15 and DM216 clinically diagnosed in accordance with the current guidelines, at least 18 years old and who had consented to inclusion in writing. We did not include patients who were not physically or mentally capable of giving consent or those who were already participating in other clinical investigations that could interfere with our study. The study was approved by the research ethics committee in the Clínic Hospital, Barcelona.
Recorded variables
We recorded the following data for each of the patients: demographic data were age, sex, body mass index (BMI), waist circumference, mid-upper arm circumference, smoking habit, alcohol use, history of cardiovascular disease (CVD), serum creatinine level, estimated glomerular filtration rate (eGFR), urinary albumin:creatinine ratio (ACRor), total cholesterol, HDL cholesterol and LDL cholesterol, triglycerides, baseline glycaemia, glycated haemoglobin (HbA1c), ambulatory blood pressure monitoring (ABPM) over the past year, self-monitoring of blood pressure at home during the past 6 months, time since diagnosed with AHT, DM and hypercholesterolemia, number of drugs administered for AHT treatment, use of angiotensin-converting enzyme inhibitors (ACEi) and/or angiotensin II receptor blockers (ARB), AHT treatment compliance, adherence to dietary advice for AHT, DM2 or hypercholesterolemia, usual physical exercise, concomitant treatment with psychoactive drugs, non-steroidal anti-inflammatory drugs (NSAID), sympathomimetic drugs, antiplatelet drugs, number of BP measurements, and number of hours since AHT treatment was last taken. Clinical parameters were: hypercholesterolemia, diabetes, cardiovascular disease or clinical BP, and were defined in accordance with guidelines from the European Society of Hypertension and the American Diabetes Association.15,16 BP was measured in accordance with the standard techniques described in the medical literature.15,17 Tight BP control was defined as SBP<130mm Hg and DBP<80mm Hg, in accordance with the AHT guidelines that were valid when the study was being conducted.18 Furthermore, given the recent critical review on the recommendations established,19 we calculated the percentage for a less tight BP control (<140/85mm Hg). Using the serum creatinine level, we estimated the GFR using the MDRD equation, and defined kidney failure as GFR<60ml/min/1.73m2.
We also asked all doctors to complete a detailed questionnaire on their usual medical practice, with special reference to measuring BP, evaluating lifestyle and hygienic/dietary measures, recommendations given to patients and their adherence to them.
Statistical analysis
We used a sample size of 600 patients to ensure that the estimation of the prevalence for good BP control was accurate by ±3.5% (95% confidence interval [CI] of 7% amplitude) supposing that this prevalence were 25%. The study was finished after the three month inclusion period was complete. We had 526 patients and considered that the number was adequate to enable us to make precise estimations. All analyses were performed on eligible patients i.e. those that complied with selection criteria and were able to provide the data needed for examining the main objective. We used the data available, and did not need to use replacement techniques for missing data. The prevalence for good BP control was estimated by calculating the 95% CI, using the normal calculations. Prevalence for successful tight BP control (SBP<130mm Hg and DBP<80mm Hg), for good SBP control and good DBP control was estimated in accordance with the clinical BP measurements.
We performed a logistic regression analysis to identify the factors associated with BP control. Firstly, we analysed the relationship using univariate models. Secondly, we adjusted a multivariate model which included all statistically significant variables (P<.25) in the corresponding univariate model. Then, using this model, we performed a stepwise selection, with entry and exit levels set at 0.05.
We initially considered the following factors: age, sex, BMI, waist circumference, mid-upper arm circumference, smoking habit, alcohol use, history of CVD, serum creatinine level, eGFR, urinary albumin-creatinine ratio (ACRor), total cholesterol, HDL-cholesterol and LDL-cholesterol, triglycerides, baseline glycaemia, glycated haemoglobin (HbA1c), time since diagnosed with AHT, DM and hypercholesterolemia, number of drugs administered for AHT treatment, use of ACEi and/or ARB, AHT treatment compliance, adherence to dietary advice for AHT, DM2 or hypercholesterolemia, usual physical exercise, concomitant treatment with psychoactive drugs, NSAID, sympathomimetic drugs, antiplatelet drugs, number of BP measurements, and number of hours since AHT treatment was last taken. The overall adjustment of the models was considered based on the Hosmer-Lemeshow test, and the (bilateral) significance of the terms using the Wald statistic. All statistical analyses were performed using the SAS® statistical package for Windows (version 9.1).
RESULTS
Patient characteristics
Fifty-five doctors included a total of 526 patients from April until July 2008. Six patients were not considered as eligible as they did not comply with some of the selection criteria. As such, 520 (98.9%) were included in the analysis.
Table 1 summarises the clinical characteristics of patients included in the study. The mean age was over 65 years old and there were more males than females. Mean time between DM2 and AHT diagnosis and inclusion in the study was more than 10 years. Three-hundred and thirty patients (63.4%) had been advised to follow a low-salt diet, 55 (10.5%) a low-fat diet due to dyslipidemia (DLP), and 455 (87.5%) had been given dietary advice for DM2.
Prevalence of good BP control
Tight clinical BP control (<130/80mm Hg) was observed in 91/520 cases (17.5% of the sample; 95% CI:14.3-21.0). Tight clinical SBP control was observed in 110/520 cases (21.2% of the sample; 95% CI:17.7-24.9), and tight DBP control was observed in 281/520 cases (54.0% of the sample; 95% CI: 49.6-58.4).
Table 2 compares the clinical characteristics of the patients with tight BP control and those that did not reach tight BP control.
Experts have recently started to question whether tight BP control is beneficial for DM2 patients, given the lack of clear evidence.19 Although the study objective was to analyse the variables related to lack of tight BP control, we also examined less-tight BP control. Less-tight clinical BP control (<140/85mm Hg) was therefore observed in 180/520 cases, (36.92% of the sample; 95% CI:32.76-41.23). SBP control was observed in 211/520 cases (40.58% of the sample; 95% CI:36.32-44.94), and DBP control was observed in 365/520 cases (70.19% of the sample; 95% CI:66.06-74.1).
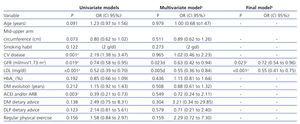
Relationship between tight BP control and predictive factors
Table 3 shows the main results from the logistic regression analysis. This table only includes the variables that had a significance of P<.25 in the univariate models. The following variables showed a statistically significant relationship (P<.05) with BP control (Table 3, univariate models): history of CVD (P<.001), GFR (P=.019), LDL-cholesterol (P<.001), treatment with ACEi and/or ARB (P=.003), and total cholesterol (not shown on the table). Given that the dependent variable was successful tight BP control, OR>1 showed that BP control was more frequent and OR<1 showed that BP control was less frequent. As a result, the OR of the variables mentioned above indicate that history of CVD (OR=2.19) is associated with a more frequent good BP control. On the other hand, GFR values (OR=.74 for one standard deviation increase) or LDL-cholesterol (OR=.52 for one standard deviation increase) and ACEi and/or ARB (OR=.39) are associated with less frequent BP control.
We included all of these variables in a multivariate logistic regression model and achieved a good overall adjustment (Hosmer-Lemeshow c2=9.81; degrees of freedom [df]=8; P=.279). According to the results of this adjustment (Table 3, multivariate model), the GFR and LDL-cholesterol have a statistically significant relationship (P<.05). Using a stepwise selection, LDL-cholesterol and GFR remained statistically significant (P<.001). OR for one standard deviation increase in LDL-cholesterol is 0.55 (0.41-0.75). This implies that when the LDL-cholesterol or GFR are higher, the patient is less likely to control BP. Mean SBP and DBP are higher in patients with LDL>100mg/dl than in patients with LDL<100mg/dl (Student’s t-test, P<.001) (data not shown). Furthermore, no statistically significant differences were found in the SBP and DBP averages for patients with LDL>100mg/dl, considering whether statins were used or not (data not shown). Lastly, 84.8% of patients with history of CVD had GFR values less than 60ml/min/1.73m2, while this occurred for 68.1% of patients that did not have CVD (OR=.38; 95% CI:0.24-0.60).
DISCUSSION
In this study we have checked a sample of patients suffering from AHT and DM2 who were cared for in nephrology units of Spanish hospitals. We found that the percentage of tight BP control (<130/80mm Hg) was 17.5%. In the univariate analysis, various factors are associated with unsuccessful BP control, such as presence of CVD, GFR, treatment with renin-angiotensin-inhibitors, hypercholesterolemia, and concomitant treatment with NSAID. However, in the multivariate analysis, only LDL-cholesterol and GFR were related to poor BP control. The prevalence of good BP control in this study is somewhat higher than that found in previous Spanish studies: in primary care11 and hypertension units,12 (12.2% and 13%, respectively). This is even more important considering that the BP criteria was <130/85mm Hg in these cases. In contrast, a recent study examining compliance of overall DM2 treatment guidelines in nephrology units in Catalonia20 observed a BP control rate of 21.8%. However, their criterion for BP control was ≤30/80mm Hg. When observing the control rate in other countries, we have noted that some observational epidemiological studies found higher BP control rates in diabetic patients. A study conducted in the United States showed that 31.4% had a BP control of <130/80mm Hg.21 In prospective intervention studies on diabetic patients, the SBP control (target <130mm Hg) was not achieved by any of the patients, while the DBP objective (<80mm Hg) was achieved by half of them. Therefore, the percentage of diabetic patients with DBP control <80mm Hg in our study (54%) is similar to those clinical trials. There is little evidence showing that reducing SBP to below 130mm Hg represents a clear benefit for the DM2 patient group. Furthermore, in no clinical trial hypertensive patients with DM2 have reached this SBP level.22 These facts have encouraged the European hypertension guidelines to be reviewed, questioning this target until there is evidence in its favour.19 Until more evidence is made available, general BP control <140/85mm Hg is recommended for all hypertensive patients. The ACCORD study,23 examining more than 4000 patients, showed that a target SBP control <120mm Hg as compared with <140mm Hg did not reduce the rate of fatal and non-fatal cardiovascular events. This outcome has confirmed that the tight BP control levels recommended to date (which are difficult to achieve) are probably unnecessary. More studies are certainly needed to clarify this important clinical matter. The objective of our study was to analyse the factors associated with a tight BP control, in accordance with a recommendation that was in practice at the time the study was designed and performed. However, given that the experts changed their opinion on the matter, we also analysed the less-tight control rate in our sample. As such, 36.9% of patients had a <140/85mm Hg control, while 40% had SBP control and 70% DBP control. These control rates are very close to those of the general hypertensive population,12 suggesting that the poor historic control attributed to DM2 is partly due to therapeutic objectives being too tight and probably unjustified.
The UKPDS38 study established a target BP control of <150/85mm Hg, and observed that 29% of the patients were being treated with three or more anti-hypertensive drugs.8 Our study’s target was <130/80mm Hg and only 35% of patients were treated with three or more drugs, which to some extent suggests that this poor control may be due to undertreatment. Even though in most clinical trials diabetic patients use three or more drugs to reach the BP target, (3.2 drugs according to Bakris et al24) the implementation of intense treatment in clinical practice does not seem to be achieved, according to the results that we present here.
Although the univariate analysis showed a worse control rate for patients treated with ACEi or ARB, we believe that this finding should be interpreted with caution. Firstly, this is because more than 90% of the patients were treated with these drugs. Secondly, we do not know the dosage that was taken, making interpretation difficult. Furthermore, this correlation was not observed in the multivariate model.
The correlation that we have observed between the GFR and BP control is in the opposite direction than was expected. Although this was analysed in a different way, the CLUE study reported a lower BP control (12%) in patients with kidney failure (defined as creatinine >1.4-1.5mg/dl, depending on sex), compared with the general sample (42%).12 In this respect, we must take into consideration that the control limits were tight (<130/80mm Hg) when considering kidney failure. The COPARENAL study,25 which is the most important study that has been conducted in Spain on BP control of kidney failure patients, showed a (<130/80mm Hg) BP control rate of only 17%. However, no difference was shown between serum creatinine and creatinine clearance between groups with and without optimal BP control. In our study, although we observed a statistically significant correlation with GFR, we believe that the difference of 7ml/min has little clinical importance to be able to consider it the cause of good or bad control. In our sample, there was a correlation between the GFR <60ml/min and cardiovascular disease. However, the correlation between GFR and BP control was no longer significant when we examined each CVD category. We could also believe that patients with lower GFR (as well as those that have more serious cardiovascular disease) could cause the doctor to pay more attention to improving BP control, although this is merely speculative. Meanwhile, a correlation between poor BP control and the proteinuria level was found in the COPARENAL study. We did not find this correlation in our study, partly because the proteinuria level in our patients was low (ACR median: 36mg/g, mean: 200mg/g). This was probably because were more patients with nephrosclerosis than with diabetic nephropathy, and they were undergoing anti-hypertensive treatment.
Furthermore, results from the multivariate logistic regression analysis show and that independent BP control was lower when LDL-cholesterol values were higher. This correlation matches with that observed in other studies on BP control in Spain: such as the one conducted in a primary care setting (PRESCAP)26 or in the COPARENAL study, mentioned above.25 The correlation between dyslipidemia and AHT is well known. Hypercholesterolemia is related to endothelial dysfunction, both in human and animal models27 and it seems that a deficiency of the nitric oxide vasodilator,28 which is involved in its mechanism, is partly produced by the oxidative effect of atherogenic lipoproteins.29 The mean LDL-cholesterol values for patients in our study were above 110mg/dl (Table 1), being higher than the figure recommended in current dyslipidemia guidelines for DM2 patients.16 However, it matches the figure found by other authors in a recent analysis of overall DM2 treatment guide compliance,20 in which only 39% of patients achieved the LDL-cholesterol target (<100mg/dl).
One limitation of our study was that we were not able to assess the doctor’s attitude when their patient did not achieve BP control, given that it was a single cross-sectional study. Another limitation found in observational and cross-sectional studies is that convenience samples are used, although this is not greatly relevant to our study as our results are similar to those found in other studies on BP control.
In summary, tight AHT control for patients with DM2 who attended nephrology units is low, while the less-tight control is similar to the general hypertensive population. Among the factors analysed, the LDL-cholesterol and GFR have an impact on the degree of BP control. Likewise, despite the vast range of drugs available, data suggest that they are underused in these patients, given that the percentage of patients treated with three or more drugs was relatively low despite poor BP control. This warns us that we need to emphasise on the number of drug used to improve BP control in diabetic patients. Similarly, the percentage of patients treated with statins may seem inappropriate, which would indicate that doctors are placing less emphasis on controlling lipids, as well as the BP. We therefore believe that understanding the factors that influence BP control could help when implementing strategies for fulfilling tight therapeutic targets in this risk population.
ACKNOWLEDGEMENTS
This study has been financed by an unconditional grant from Laboratorios Menarini, S.A.
Table 1. Clinical characteristics of patients studied
Table 2. Clinical characteristics of the patients in accordance with degree of blood pressure control
Table 3. Variables that affect good control of blood pressure according to the logistic regression analysis