La ateroembolia de colesterol (AEC) es una enfermedad sistémica cuya incidencia ha aumentado en las últimas décadas y que presenta una elevada morbimortalidad. En el momento actual se desconocen cuáles son las alternativas terapéuticas más efectivas en esta entidad. En este artículo presentamos el caso de una paciente diagnosticada de AEC con afectación cutánea, intestinal y renal, que presentó una buena evolución tras el inicio de terapia combinada con esteroides y análogos de las prostaglandinas. A pesar de que no existen estudios concluyentes, sugerimos esta alternativa para el manejo de AEC con afectación orgánica.
Cholesterol atheroembolism (CAE) is a systemic disorder whose incidence has increased in recent decades and that presents high morbidity and mortality. Although several therapeutic alternatives have been reported, there is no consensus about the best treatment for this disease. In this paper we report the case of a patient with CAE with skin, bowel and kidney involvement who presented a good response to combined therapy with steroids and prostaglandin analogues. Although there are no conclusive studies, we recommend this therapeutic alternative in the management of CAE with organic failure.
INTRODUCTION
Cholesterol atheroembolism (CAE) is a disease with a poor prognosis. The pathogenesis of this disease is based on the impact of cholesterol crystals derived from atheromatous plaques in small vessels.1 In recent years, the incidence of CAE has increased as the result of a burgeoning population of individuals that are particularly susceptible to this disease (elderly patients, those with diabetes, hypertension, and dyslipidaemia) in addition to a greater frequency of triggering factors (endovascular procedures, anti-coagulation treatment).2 CAE produces important rates of morbidity and mortality, which increase when the kidneys are also involved. Renal function is recovered following this disease in only 25% of cases.1,2
The management of CAE is a complicated task due to the lack of unified treatment criteria in the medical literature. It does appear that these patients benefit from a strict control of cardiovascular risk factors in order to prevent the development of this disease.3,4 However, there is no agreement regarding the measures to take when the disease has already been triggered. Several articles exist in the medical literature suggesting various treatment regimens, although no definitive results have been shown either to refute or support these recommendations.5
In this article, we present the case of a patient with CAE with peripheral vascular and renal involvement who benefited from combined treatment with steroids and prostaglandin analogues (iloprost).
CASE REPORT
Our patient was a 71-year old female who sought treatment in the nephrology department at our hospital due to an acute deterioration in renal function. The patient’s relevant background included: arterial hypertension (on treatment with enalapril), dyslipidaemia, tobacco use, and grade IIA peripheral vascular disease, with Doppler-ultrasound tests indicative of a significant stenosis in the left femoral artery. Basal renal function was normal.
In December 2012, the patient underwent an arteriography for peripheral vascular disease, which led to a balloon angioplasty of the superficial femoral artery of the left leg, with 2 stents implanted. After 24 hours, the patient was administered Adiro® and low molecular weight heparin (LMWH) and discharged from the hospital. Serum creatinine (Crs) at this moment was 1.26mg/dl.
Ten days later, the patient went to the emergency department due to rectal bleeding with no haemodynamic instability (blood pressure: 127/83mm Hg). Laboratory analysis revealed Hb: 9.8g/dl, 8000 leukocytes/mm3, and 17% eosinophils (1400/mm3). Crs was 4.3mg/dl. During the patient’s stay in the emergency department, treatment with LMWH and enalapril was suspended and volume expansion therapy was started. A colonoscopy was also performed that revealed colonic ulcers indicative of ischaemia. No further rectal bleeding occurred in the following 24 hours, and Crs decreased to 3.42mg/dl. The patient was discharged to her home with a referral to the nephrology department, where she sought further treatment 15 days later.
On her visit to the nephrology department, the patient had a Crs of 4.44mg/dl, acidosis, and hyperkalaemia, which motivated her hospitalisation. Upon evaluation, the patient reported the appearance of painful purple-coloured lesions on the toes and soles of both feet. These lesions appeared 10 days after the endovascular procedure and had worsened with time. A biochemical analysis revealed that the eosinophilia continued, and no improvements could be seen in renal function. A urinary sediment analysis revealed isolated leukocytes with no red blood cells. A dilated fundus examination was normal, and a Doppler-ultrasound showed the kidneys to have normal size and good cortical-medullary differentiation, a non-dilated urinary tract, and an absence of stenoses in the renal arteries.
Given the patient’s history of endovascular manipulation, clinical symptoms, and biochemical parameters, we suspected the presence of CAE with renal involvement (known as atheroembolic renal disease [AERD]). The diagnosis was confirmed with a cutaneous biopsy of the purple lesions on the patient’s feet, in which we observed the intravascular cholesterol crystals typical of this disease.
Given the progressive worsening of renal function (maximum Crs of 5.58mg/dl) and cutaneous lesions, we decided to start treatment with iloprost (2ng/kg/min during 12 hours per day for 14 days), steroids (1mg/kg/day for one week, followed by a decreasing treatment regimen until complete removal after 3 months) and high doses of statins (atorvastatin at 80mg/24h).
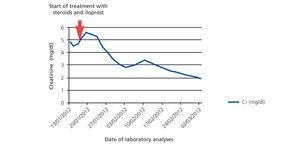
Two days after starting treatment, the patient experienced a progressive improvement in the cutaneous lesions that allowed for reducing the dose of analgesia. This prescription also produced an improvement in renal function, which started one week after starting treatment. Given the good evolution of the patient’s condition, she was discharged to her home one month after hospitalisation. Crs upon discharge was 2.99mg/dl, and 3 months after hospitalisation, Crs was down to 1.9mg/dl (Figure 1).
DISCUSSION
CAE is a systemic disease that produces high rates of morbidity and mortality. It can affect any organ system throughout the body, with the most commonly affected organs being the kidneys, gastrointestinal tract, and the skin. CAE produces a mortality rate after one year that ranges between 30% and 80%, according to studies. When CAE produces renal involvement (AERD), the progression of the disease tends to be quite severe, necessitating dialysis in 40% of cases. Only 25% of these patients eventually recover renal function.3-4 The differential diagnosis of this disease also includes several different entities, such as contrast-induced nephropathy and immunoallergic interstitial nephritis.5
Two different treatment protocols exist for patients with CAE. The first is designed to avoid the reappearance of CAE by controlling cardiovascular risk factors (blood pressure and atheromatous plaques) and avoiding exposure of the patient to factors that could trigger symptoms (anti-coagulants, endovascular interventions). The other type of treatment attempts to reduce the level of ischaemia produced in affected organs in order to improve their functioning. Drugs in this second treatment type include steroids and prostaglandin analogues.6
Several studies have shown that preventative measures reduce the mortality of patients with CAE.2,4 However, the use of specific treatment measures to combat the disease continues to be the subject of much debate.
The pathogenesis of CAE is based on the release of cholesterol crystals from atheromatous plaques that accumulate and obstruct small vessels, producing ischaemic damage in various organs of the body. A histopathological analysis reveals an important inflammatory component in the form of a reaction to the cholesterol crystals as foreign bodies. This inflammatory component also contributes to the vascular obstruction that produces ischaemia.1,2 Through steroid treatment, we attempt to improve the inflammatory component of the embolism by increasing distal blood flow to the vascular obstruction and reducing ischaemic damage. Experimentally, this mechanism has not been demonstrated in vivo. In studies published of cases treated with steroids, arguments have been presented both in favour and against this treatment alternative for improving renal function. For example, in a study involving three Spanish hospitals (Hospital Parc Taulí de Sabadell, Hospital de Ciudad Real and Hospital 12 de octubre),7 which examined 45 cases of CAE, no beneficial effects were observed from steroid use. However, the overall trend in studies published on this disease appears to be improved symptoms of skin and gastrointestinal ischaemia in patients treated with steroids.8-10
Recently, prostaglandin analogues (iloprost) have been added to the treatment arsenal against CAE. These drugs have important vasodilatory and anti-platelet activity, making them ideal for use in various diseases with ischaemic components, with good results.11 Iloprost was first used for the treatment of CAE with cutaneous lesions in 1995. Treatment was effective, with improvements observed in cutaneous lesions and pain.12 Since then, six cases have been published in which iloprost was used to treat CAE.13-15 In all of these, clear improvements were observed in terms of cutaneous lesions and pain, and 50% of the patients also enjoyed an improvement of renal function. In almost all of these cases, combined treatment was administered with iloprost and steroids (Table 1).11-14
Our patient had CAE with important renal, cutaneous, and gastrointestinal involvement. After reviewing the pertinent medical literature, and in light of the poor evolution of the patient’s condition, we decided to apply combined therapy with steroids and iloprost. After starting treatment, we observed clear improvements in the cutaneous lesions and pain, with reduced requirements for analgesic prescriptions. Additionally, renal function, which until this point had suffered progressive deterioration, started to improve 48 hours following the start of treatment. Currently, the patient’s Crs is 1.9mg/dl.
Our case reflects the experiences of other case reports and provides a certain level of optimism for the use of combined therapy with steroids and iloprost.
Combined therapy does not produce a recovery of renal function in all patients, but it does improve extra-renal symptoms, which are often the most important drivers of the prognosis in these patients.4
One very important factor in the response of CAE to treatment is the moment in which treatment is started. Given the pathogenesis of the disease, it is essential to start treatment as soon as possible. If delayed, the affected parenchyma suffers an even greater degree of damage and the probability of recovered function decreases. This parameter has not been evaluated in any studies to date, and may improve the rate of recovery of renal function in these patients.
No studies involving the combined treatment of this condition with steroids and iloprost have described important adverse effects. In all of these, the steroids used were at low doses and for short periods of times.
The aforementioned arguments along with an absence of other treatment alternatives leads us to suggest that combined treatment with steroids and iloprost should be considered for the treatment of patients with CAE and organ damage. This therapy should be started as soon as possible in order to optimise results. This should also be confirmed through the application of prospective and randomised clinical studies.
Conflicts of interest
The authors state that they have no potential conflicts of interest related to the contents of this article.
Figure 1. Evolution of renal function
Table 1. Review of the use of iloprost in cases of cholesterol atheroembolism