The incidence of pleuroperitoneal leak in peritoneal dialysis (PD) is 1.6%, and it occurs in up to 20% of patients who have been using the technique for over a year.1,2 The presence of a communication (congenital or acquired) between the peritoneum and the pleura, associated with an increase in intra-abdominal pressure, can lead to a secondary hydrothorax with dyspnoea and ultrafiltration failure. The first line of treatment consists of peritoneal rest, but chemical pleurodesis can be used in cases of recurrence and depending on the patient's need or desire to remain on PD. We present the case of a 77-year-old woman with a history of hypertension, type 2 diabetes mellitus, obesity and chronic kidney disease secondary to diabetic nephropathy, on continuous ambulatory PD (CAPD) programme, with three daily exchanges per day of 2,000 ml each.
One year after starting on PD, the patient had an episode involving problems with peritoneal drainage and right pleural effusion. Cancer and inflammatory or infectious causes were ruled out by diagnostic thoracentesis, but her pleural fluid was found to have high glucose levels. A likely pleuroperitoneal leak was diagnosed, which resolved spontaneously with peritoneal rest, and the patient remained on PD.
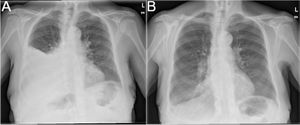
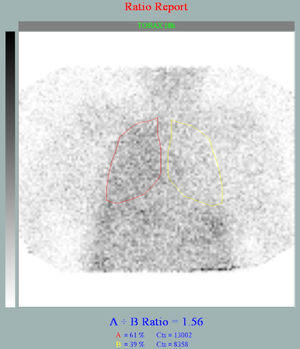
One month later, the patient consulted once again with similar problems, and chest X-ray showed a right pleural effusion (Fig. 1A). Peritoneal scintigraphy showed uptake of the radiotracer in the right hemithorax (Fig. 2), confirming the suspected pleuroperitoneal communication. Given the high risk of recurrence, the patient was offered the option of being transferred to haemodialysis, but she wanted to continue on the PD programme, elective admission was arranged to stop the leak by chemical pleurodesis.
Once in the hospital, a chest tube was inserted and 60 ml of 10% povidone-iodine diluted in 60 ml of 0.9% saline was administered into the patient's pleural cavity. Twenty-four hours after the procedure, she developed a low-grade fever, pleuritic chest pain, increased leucocyte count (to 40,000/μl), neutrophilia (80-90%) and increased C-reactive protein and procalcitonin (to 2.59 ng/ml) in the context of a secondary chemical pleurisy. Consequently, despite the negative results of blood and pleural fluid cultures, the chest tube was removed and the patient was started on treatment with levofloxacin. Over the next few days, the patient began haemodialysis and it was observed a gradual decrease in inflammatory markers and remission of low-grade fever.
Eleven days after the procedure, due to persistence of the right pleural effusion, a second chest tube was inserted, and the same procedure was repeated, as before. This time, the patient did not develop any significant inflammation. However, she did have a self-limiting episode with an atrioventricular junctional rhythm of 50 bpm, without any electrolyte imbalance detected, which remitted spontaneously. She also developed symptoms of pneumatosis intestinalis, which were effectively treated with empirical antibiotic therapy.
Four weeks after admission, having verified resolution of the pleural effusion (Fig. 1B), the chest tube was removed and the patient was discharged from hospital, restarting a CAPD regimen, initially with low volumes per exchange, but later progressing to three exchanges of 2,000 ml in 24 h with glucose and icodextrin. After one year of follow-up, the patient remains on CAPD with no recurrences of the pleuroperitoneal leak, no thyroid dysfunction and no evidence of pleural effusion.
A high success rate has been described with the use of talc as a chemical agent in the pleurodesis of malignant pleural effusion. However, there is growing concern about its safety,3 and there is no robust evidence to recommend its use over other strategies.4 Other methods include the use of povidone-iodine, tetracyclines, bleomycin and instillation of autologous blood.5
Povidone-iodine is a low-cost option, with few side effects and 90% efficacy, which induces a powerful inflammatory response with pleural sclerosis.6–9 However, there is still limited evidence on the management of this complication in PD.5 Gulcan et al.10 are the only authors to report the use of povidone-iodine in PD for chemical pleurodesis in a 67-year-old man, achieving resolution of the hydrothorax three days after the procedure and restarting his CAPD regimen without incident.
In conclusion, pleurodesis with povidone-iodine is a useful technique for the treatment of pleuroperitoneal leak in patients on PD, which limits recurrences and helps patients to continue using PD. In our case, the inflammatory reaction and other adverse effects seen after intrapleural povidone-iodine instillation were self-limiting. It is possible that this patient's many comorbidities contributed to her developing these complications.
FundingThis study has received no specific funding from public, private or non-profit organisations.
Please cite this article as: Guerra-Torres XE, Rodríguez Doyágüez P, Ovejero Merino E, Chávez Guillen AV, Bouarich H, Moreno Barrio F. Pleurodesis química con povidona yodada para el manejo de la fuga peritoneo-pleural en diálisis peritoneal: a propósito de un caso. Nefrologia. 2022;42:213–215.