Dear Editor,
Cat scratch disease (CSD) is an infectious disease that usually presents as a self-limiting illness characterized by regional lymphadenopathy, fever and constitutional symptoms in association with a cat scratch or bite.1-4 In most cases, Bartonella henselae is the etiologic agent and cats are important reservoirs.2-5
We report a case of CSD in a 38-year-old Caucasian female recipient of a deceased kidney transplant since 2006 due to chronic renal failure of unknown etiology. Her maintenance immunosuppressive treatment was mycophenolate mofetil and cyclosporine. She was also medicated with calcium carbonate, vitamin D, atenolol, folic acid, fluoxetine, omeprazole, ferrous sulfate.
Six years post transplantation the patient was admitted to the hospital with a 4-week history of asthenia, low fever, loss of weight and multiple painful cervical ganglions. There was no previous history of tuberculosis. She had close contact at home with cats. On physical examination, the patient had a temperature of 37,3ºC, pulse rate of 84/min, blood pressure of 134/88mmHg, respiratory rate of 16/min and pulse oximetry of 100% in ambient air. She had multiple bilateral painful ganglions only in cervical region (node size ≤4cm). There was no rash. Examination of the lungs, heart and abdomen revealed no abnormalities including hepatosplenomegaly. The graft was painless. Laboratory tests revealed a white blood cell count 11,81×10^3/L (neutrophils 65,8%, lymphocytes 23,6%, monocytes 10%, eosinophils 0,1%), normochromic-normocytic anemia (Hgb 9,6g/dL); creatinine 1,2mg/dL (basal value), blood urea nitrogen 39mg/dL; protein C reactive 143mg/L; LDH, SGOT, SGPT, total bilirubin and alkaline phosphate without alterations. Ultrasound cervical ecography demonstrated multiple ganglion formations.
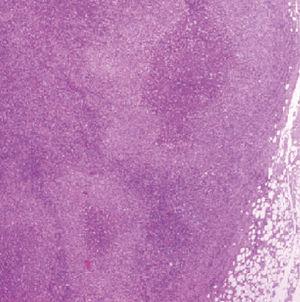
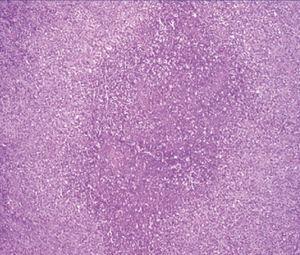
She was observed on admission by an otorhinolaryngologist who prescribed metronidazole plus amoxicillin and clavulanate for a nasopharynx´s infection. Serologies for Epstein-Barr virus, herpes virus, cytomegalovirus, toxoplasmosis, brucella, leishmania, and HIV infection were negative. Blood culture was sterile. Chest and abdominal CT scan without changes. Quantiferon test for tuberculosis was indeterminate. Peripheral blood cytometry and cytometry of ganglion did not showed immunophenotypic alterations compatible with lymphoma. An ganglion biopsy was performed and histological examination revealed reactive lymphadenitis with central necrosis (Ziehl neelsen was negative) alterations compatible with CSD (Figure 1 and Figure 2). She stopped the initial antibiotherapy on the 6th of internment (without improvement of complains) and began azithromycin 500mg on day one, followed by 250mg for four days. There has been a good clinic improvement with involution of ganglion swelling and resolution of the pain and fever. One month later the patient was asymptomatic, without any signs of recurrence.
This case report intends to illustrate that the investigation of an immunocompromised kidney transplant patient presenting with lymphadenopathy may constitute a challenge given the wide differential diagnosis possible. The presence of enlarged lymph nodes in those patients should lead to post-transplant lymphoproliferative disorders (PTLD) as a first hypothesis; however more benign and unsuspected causes must be the cause.
The risk of PTLD is associated with the degree of immunosupression, time post transplant and the presence of Epstein-Barr virus.6-9 Their incidence is approximately 30 to 50 times greater than in the general population and comprises a wide histological spectrum from hyperplastic appearing lesions, non-Hodgkin lymphoma or multiple myeloma histology.6,8
Regional lymphadenopathy is the hallmark of CSD in association with mild constitutional symptoms and a previous history of cat scratch or bite.1-3 In our case the investigation was wide and extensive once this disease can mimic the more common PTLD disease or others infectious causes.2-4 In addition to serological tests a lymph node biopsy was performed to exclude lymphoma or other malignant causes. It has been proposed that at least three of four criteria must be present to establish the diagnosis of CSD: a) cat or flea contact; b) negative serology for other causes of adenopathy or sterile pus aspirated from a node or a positive Bartonella PCR assay or liver or spleen lesions on CT scan; c) positive serology for Bartonella henselae (EIA or IFA≥1:64); d) biopsy showing granulomatous inflammation consistent with CSD or a positive Warthin-Starry silver stain.2,3,10 The diagnosis of CSD in our patient was based on the presence of a cat contact history, negative serology for other causes and a ganglion biopsy compatible with CSD (Figure 1 and Figure 2). Serologic methods for detection of Bartonella henselae were not available in our hospital and it was not possible to isolate this agent by culture. The treatment of this entity is recommended in immunocompromised patients due to high risk for disseminated and recurrent CSD.2,3
Although CSD had rarely been reported in kidney transplant patients it should be considered in the differential diagnosis of patients with lymphadenopathy and a history of cat exposure.5 The absence of easy complementary tests, the difficulty in isolating the bacteria and the need of tissue biopsy makes a difficult diagnosis.
Conflict of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Figure 1. Ganglion biopsy Focus of necrosis, some surrounded by granulomatous inflammation in cortical region (H&E, original magnification x40).
Figure 2. Ganglion biopsy Focus of stellate aspect necrosis with epithelioid macrophages in the periphery (H&E, original magnification x100).