To the Editor,
A 75 year-old male came to the emergency department due to epigastralgia of five days of evolution. Two weeks before, he had received non-steroidal anti-inflammatory drugs (NSAIDs), due to a trauma of his right wrist, which he had to suspend due to the digestive symptoms described above.
As personal history of significance, he had undergone a radical prostatectomy for a tumour and suffered sphenoid sinus aspergillosis in October 2011.
- Physical examination: blood pressure 195/77mmHg; no other relevant findings.
- Laboratory tests showed: creatinine: 5.38mg/dL, urea: 116mg/dL, amylase: 113IU/L, sodium: 136mEq/L, potassium: 4.7mEq/L, normal blood count.
- Urine analysis: leukocyturia.
- Complement: C3: 39 (85-180), C4: <1.4 (10-40).
- Immunoglobulins: IgG: 2460 (680-1530), IgG4: 72 (9-104), IgM: 36 (40-240), IgA: 127 (70-400).
- Antinuclear antibodies, anti-DNA antibodies, ANCA, anti-RO antibodies, anti-La antibodies: negative.
- Cryoglobulins: negative.
- Angiotensin-converting enzyme: 30 (8-50).
- Hepatitis B, Hepatitis C, and human immunodeficiency virus serology: negative.
- Protein in 24-hour urine: 0.5 grams.
- Blood immunoelectrophoresis: normal.
- Urine immunoelectrophoresis: light precipitation band in kappa light-chain.
- Bone marrow: normal.
- Upper digestive endoscopy and colonoscopy were normal.
- Abdominal ultrasound, chest and abdomen X-ray: nothing of note.
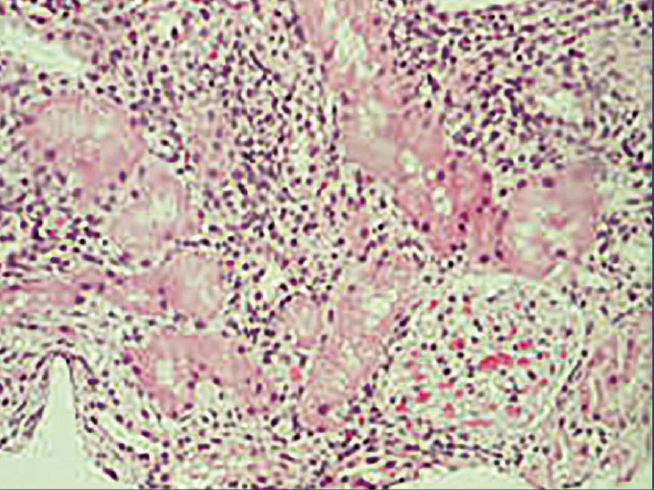
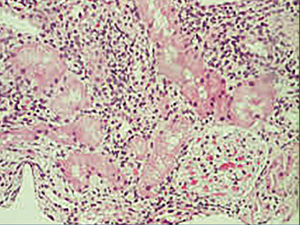
Initially, it was interpreted as tubulointerstitial nephritis (TIN) related to NSAIDs. Finding low complement values expanded our differential diagnosis and included suspected lupus nephritis, mixed cryoglobulinaemia, post-infectious and membranoproliferative glomerulonephritis. So we performed a renal biopsy (Figures 1 and 2): renal cylinder with six glomeruli without significant alterations. Inflammatory interstitial lymphocyte infiltrate with few plasma cells. On direct immunofluorescence, a granular deposit of immunoglobulin G and C3 is seen in the tubular baseline membrane and in Bowman's capsule of some glomeruli.
This finding led us to consider a differential diagnosis with systemic lupus erythematosus (SLE), Sjogren, TIN related to Ig4 and idiopathic TIN.
This last term covers three separate entities: TINU (tubulointerstitial nephritis and uveitis), nephritis due to baseline membrane antibodies and low complement TIN. SLE is ruled out due to the absence of antibodies and negative symptoms, Sjogren's syndrome is also ruled out since there is no xerostomia or xerophthalmia, and antibodies are negative.
IgG4-related TIN, name proposed by Saeki et al, is included in a recently described syndrome known as IgG4-related autoimmune disease of unknown origin. It is characterised by elevated plasma IgG4 associated with lymphocyte and plasma cell infiltrates of any organ with a predominance of IgG4-positive plasma cells. In the kidney, TIN is the most characteristic finding with low complement in a high percentage of cases.
We ruled out this entity as IgG4 levels were not high and no other organ was involved.
The patient was diagnosed with low complement TIN. It is a rare entity of unknown pathogenesis. There are several hypotheses regarding the formation of in situ or preformed circulating immune-complex deposits. This disorder usually affects males with a mean age at presentation of 66 years. The most common clinical presentation is renal failure with low complement.
Treatment experience is limited and consists mainly of steroids associated or not with other immunosuppressive drugs.
Mean duration of treatment is 3-12 months. In some cases of recurrence or treatment failure other drugs used are: cyclophosphamide, mycophenolate mofetil and tacrolimus.
In the case of our patient, we used prednisone at a dose of 1mg/kg/day, gradually tapered off, with excellent tolerance and partial response in renal function. In the last review, after four months of treatment, the patient had creatinine values of 2.7mg/dL and normal C3 and C4 values: 6.
We conclude that low-complement TIN should be included in the differential diagnosis of any renal failure with low complement without failing to consider IgG4-related disease.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Figure 2. Interstitial infiltrate with healthy glomeruli
Figure 1. Deposits of IgG and C3 in the baseline membranes of the tubules and in Bowman's capsule with intact glomeruli