The efficacy of fluconazole as a prophylactic strategy in patients with chronic kidney disease (CKD) on peritoneal dialysis (PD) with prior antibiotic exposure is controversial in the current literature. This study aimed to compare a strategy of fluconazole prophylaxis versus no-prophylaxis for patients in PD on antibiotics for previous episodes of peritonitis.
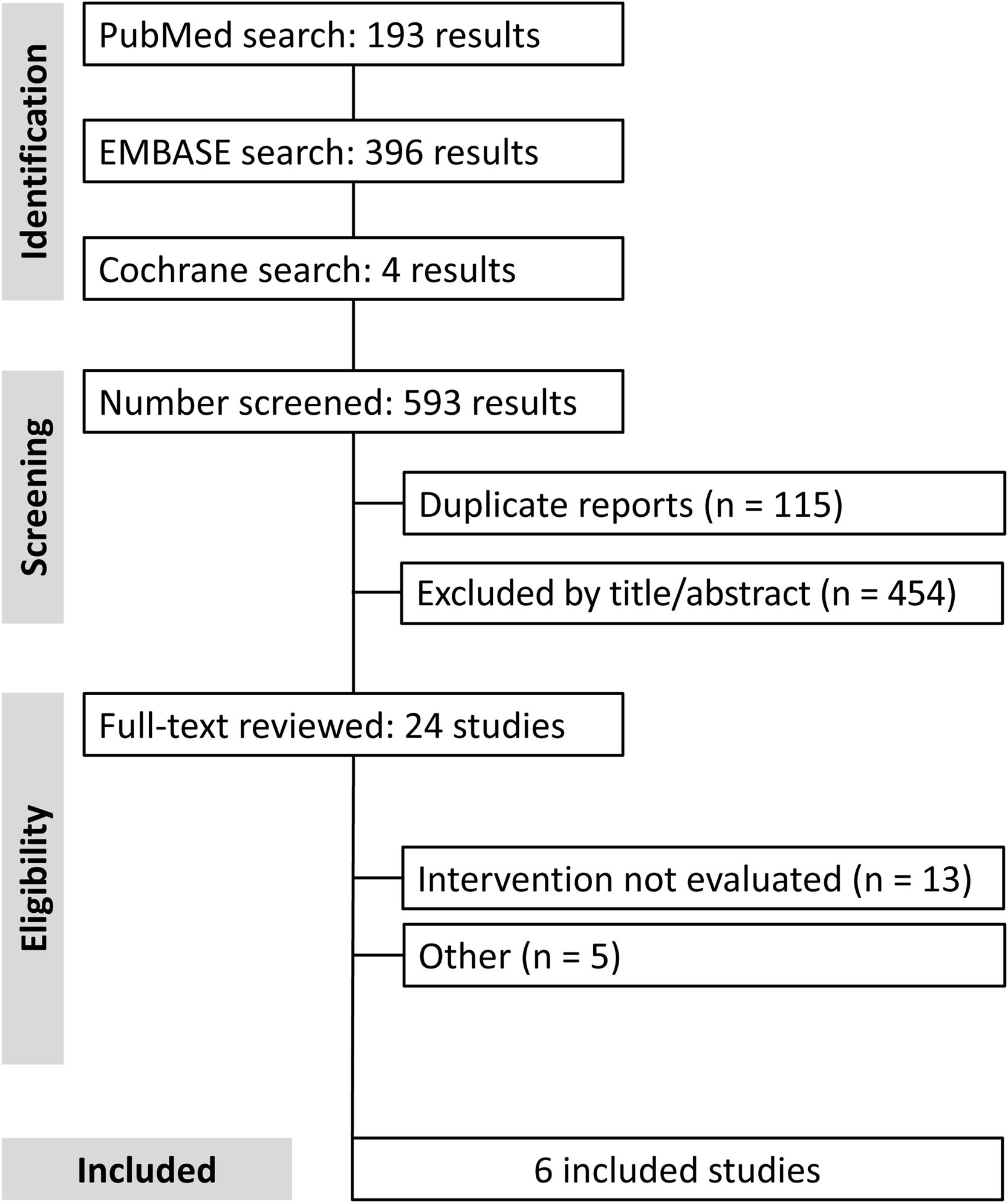
Materials and methodsWe performed a systematic review and meta-analysis of observational studies and randomized controlled trials (RCTs) comparing fluconazole prophylaxis with no prophylaxis for PD-related peritonitis. The search was conducted on PubMed, EMBASE, and Cochrane Central in January 23, 2023. The outcome of interest was the occurrence of fungal peritonitis (FP).
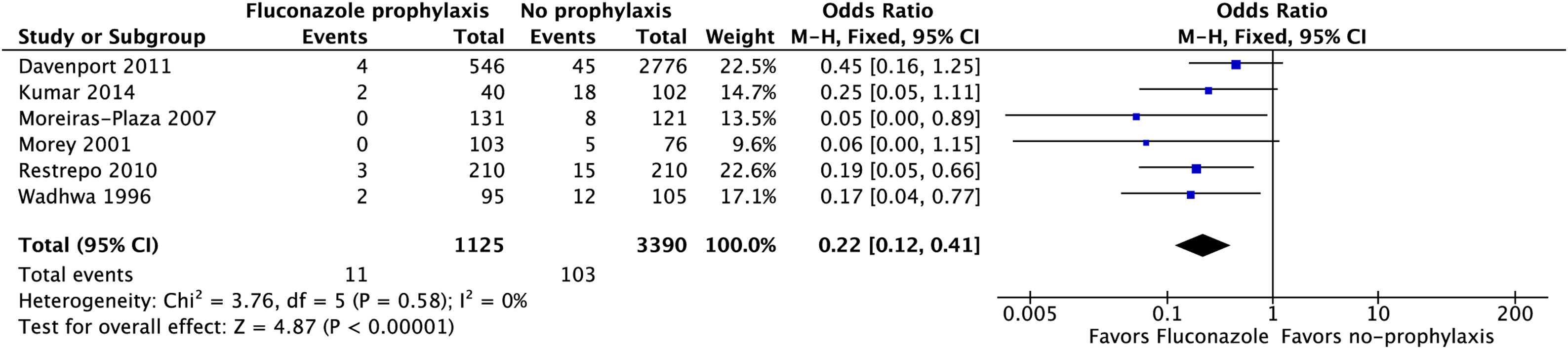
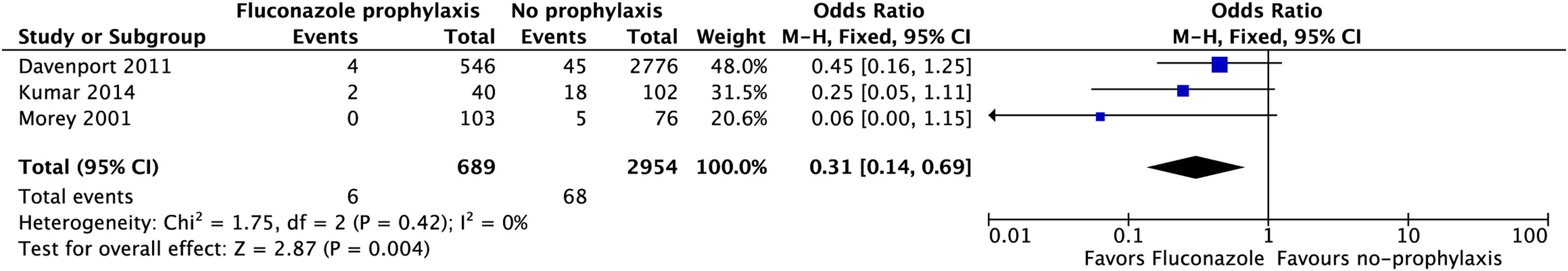
ResultsWe included six studies (1 RCT, 5 observational) with 4515 occurrences of peritonitis, of which 1098 (24.8%) received fluconazole prophylaxis in variable doses, whereas 3417 (75.6%) did not receive prophylaxis during peritonitis episodes. Overall, fluconazole prophylaxis was associated with a lower incidence of FP (OR 0.22; 95% CI 0.12–0.41; p<0.001; I2=0%). Subgroup analysis of studies that administered daily doses of fluconazole also demonstrated a reduced incidence of FP in patients who received antifungal prophylaxis (OR 0.31; CI 0.14–0.69; p=0.004; I2=0%).
ConclusionsIn this meta-analysis of 4515 episodes of PD-related peritonitis, prophylaxis with fluconazole significantly reduced episodes of FP as compared with no antifungal prophylaxis.
La eficacia de fluconazol como estrategia profiláctica en los pacientes con enfermedad renal crónica (ERC) sometidos a diálisis peritoneal (DP) con exposición antibiótica previa es controvertida en la literatura actual. El objetivo de este estudio fue comparar la estrategia de profilaxis con fluconazol frente a no profilaxis para los pacientes de DP con régimen antibiótico por episodios previos de peritonitis.
Materiales y métodosRealizamos una revisión sistemática y metaanálisis de estudios observacionales y ensayos controlados aleatorizados (ECA), comparando la profilaxis con fluconazol y la no profilaxis para la peritonitis relacionada con DP. Dicha búsqueda se realizó en PubMed, EMBASE y Cochrane Central el 23 de enero de 2023. El resultado de interés fue la aparición de peritonitis fúngica (PF).
ResultadosIncluimos seis estudios (1 ECA, 5 observacionales) con 4.515 episodios de peritonitis, de los cuales 1.098 (24,8%) recibieron profilaxis de fluconazol en dosis variables, mientras que 3.417 (75,6%) no recibieron profilaxis durante los episodios de peritonitis. En general, la profilaxis de fluconazol estuvo asociada a una menor incidencia de PF (OR: 0,22; IC 95%: 0,12-0,41; p<0,001; I2=0%). El análisis de subgrupo de los estudios que administraron dosis diarias de fluconazol también demostró una incidencia reducida de PF en los pacientes que recibieron profilaxis antifúngica (OR: 0,31; IC 95%: 0,14-0,69; p=0,004, I2=0%).
ConclusionesEn este metaanálisis de 4.515 episodios de peritonitis relacionada con DP, la profilaxis con fluconazol redujo significativamente los episodios de PF, en comparación con la no profilaxis antifúngica.
Fungal peritonitis (FP) is a catastrophic complication that can occur in patients on peritoneal dialysis (PD). It is associated with a high rate of treatment failure and mortality, and current guidelines recommend immediate catheter removal upon identification of fungi.1 Most cases of FP are preceded by antibiotic exposure,2 which is frequently used in patients on PD for empirical treatment of PD-related episodes of peritonitis, posing a significant risk factor for FP.3
Nowadays, PD-related peritonitis remains one of the most serious complications for PD. Indeed, it is the leading cause of PD technique failure and carries a significant risk of death in this patient population.4 FP represents only about 1–12% of overall cases of peritonitis in patients on dialysis.5–7 However, it is associated with devastating impacts in clinical practice, including catheter removal, migration to hemodialysis, and high mortality rates, ranging from 10 to 36% in the literature,8,9 nearly ten-fold higher as compared with bacterial peritonitis.10
Antifungal prophylaxis for FP has been studied previously using various antimycotic agents, including fluconazole, ketoconazole, and nystatin.11 However, there are conflicting findings in the literature about the efficacy of these therapies in the prevention of FP.12–17 Fluconazole, a member of the triazole class of antifungal medications, inhibits the synthesis of ergosterol, a crucial component of fungal cell membranes.18 It has a broad-spectrum activity against various fungal species, including Candida albicans, the most common cause of FP in PD patients.3 It is well tolerated, with a favorable safety profile, making it a suitable option for prophylaxis in patients on PD.
The 2022 updates from the International Society for Peritoneal Dialysis (ISPD) and the Sociedad Española de Nefrología guideline recommend the use of antifungal prophylaxis to prevent peritonitis in patients on PD who have been exposed to antibiotics. This recommendation is supported by a 1B level of evidence (LOE).1,19 This is based on data from a previous Cochrane meta-analysis that included various strategies for peritonitis prevention. However, the prior meta-analysis included a limited number of studies and pooled different antifungal agents under the same comparison.2 Therefore, we performed a meta-analysis evaluating the efficacy of fluconazole compared with no antifungal prophylaxis during episodes of peritonitis for the reduction of FP.
Materials and methodsEligibility criteriaOnly studies meeting the following eligibility criteria were included in this meta-analysis: (1) randomized controlled trials (RCTs) or nonrandomized studies; (2) comparing fluconazole (intervention group) with no antifungal prophylaxis (control group); (3) in patients on PD; (4) with an episode of peritonitis; and (5) reporting the incidence of FP. We excluded studies with (1) no control group; (2) with antibiotic therapy for non-peritonitis bacterial infections; or (3) with a report on the efficacy of other strategies for prophylaxis of FP, but without a report on fluconazole data.
Search strategy and data extractionWe systematically searched PubMed, EMBASE, and Cochrane Central Register of Controlled Trials in January 20, 2023 with the following search terms: ‘peritoneal dialysis’, ‘fluconazole’ and ‘peritonitis’. A complete electronic search strategy is reported in the Supplementary Appendix. We manually searched the references from all included studies for any additional studies. Two authors (M.G. and F.T.) independently extracted the data following predefined search criteria and quality assessment. This study was registered with the International Prospective Register of Systematic Reviews (PROSPERO) under the number CRD42023394932.
Endpoints and subanalysesThe main outcome of interest was the incidence of fungal peritonitis as defined by the ISPD criteria for FP. Prespecified subanalyses included data restricted to (1) non-RCTs; and (2) studies with daily doses of fluconazole. In addition, a leave-one-out sensitivity analysis was performed to examine the robustness of the results. This was accomplished by systematically removing each study from the analysis and recalculating the results.
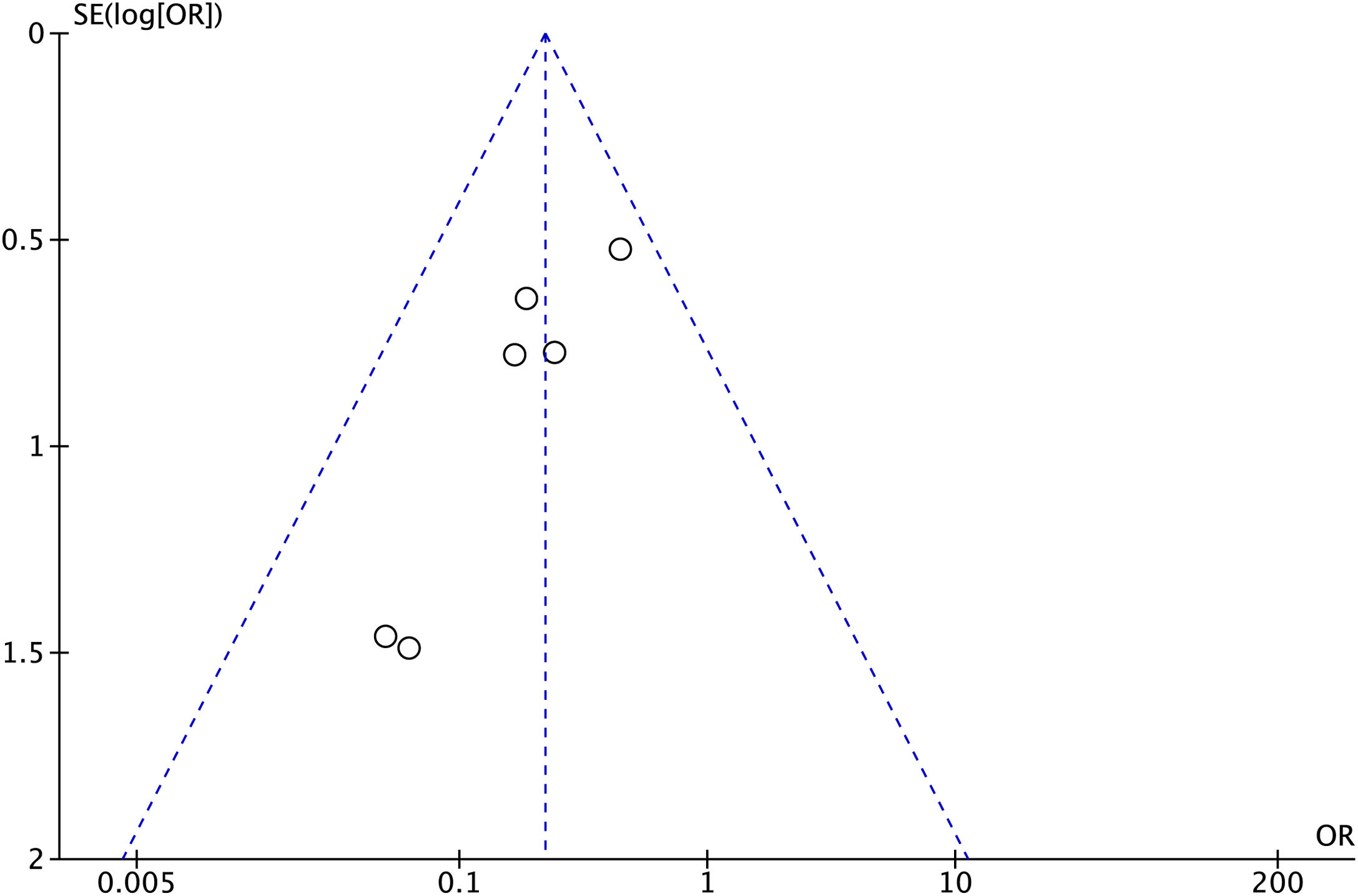
Quality assessmentNon-randomized studies were appraised with the Newcastle–Ottawa Scale (NOS).20 The NOS scores studies on a 0–9 scale based on the quality of patient selection, comparability of groups, and adjudication of outcomes. Quality assessment of the RCT included was performed using the Cochrane Collaboration's tool RoB-2 for assessing risk of bias in randomized trials for quality assessment of individual randomized studies.21 Publication bias was assessed using funnel-plot analysis of point estimates according to study weights.
Statistical analysisThis systematic review and meta-analysis were conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement guidelines.22 Odds-ratios (OR) with 95% confidence intervals were used to compare treatment effects for categorical endpoints. Cochran Q test and I2 statistics were used to assess for heterogeneity; p values below 0.10 and I2 over 25% were considered significant for heterogeneity. We used a fixed-effect model for outcomes with low heterogeneity (I2<25%). Otherwise, a DerSimonian and Laird random-effects model was used. We also performed a sensitivity analysis with the generic inverse variance method using adjusted risk estimates from observational studies, when available. Review Manager 5.4 (Cochrane Centre, The Cochrane Collaboration, Denmark) was used for statistical analysis.
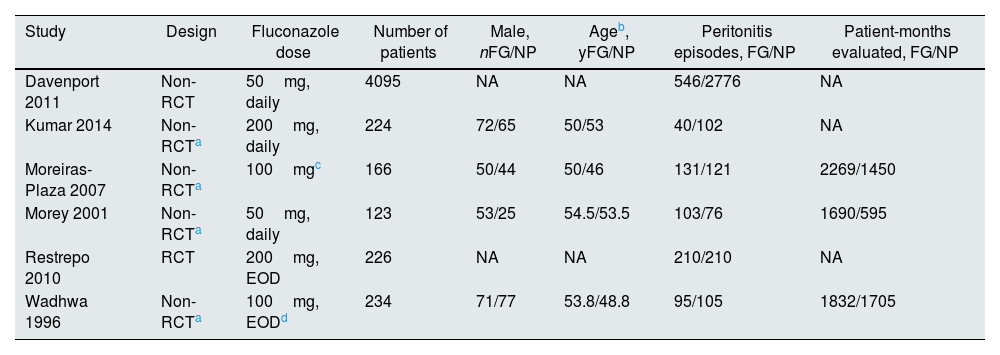
ResultsThe initial search yielded 593 results, as shown in Fig. 1. After removing duplicate records and ineligible studies, we thoroughly reviewed 24 studies. Six studies were ultimately included, comprising 4515 episodes of peritonitis from one RCT23 and five cohort studies.24–28 Among these episodes, 1124 (24.8%) were administered fluconazole prophylaxis, while 3390 (75.1%) did not receive any antifungal prophylaxis. Study characteristics are detailed in Table 1. One study also had an arm with nystatin prophylaxis; however, episodes of peritonitis treated with nystatin were not included in this meta-analysis, as per inclusion/exclusion criteria.26 There was some variability in the duration of prophylaxis, doses, and duration of follow-up, as reported in Table 1.
Baseline characteristics of included studies.
| Study | Design | Fluconazole dose | Number of patients | Male, nFG/NP | Ageb, yFG/NP | Peritonitis episodes, FG/NP | Patient-months evaluated, FG/NP |
|---|---|---|---|---|---|---|---|
| Davenport 2011 | Non-RCT | 50mg, daily | 4095 | NA | NA | 546/2776 | NA |
| Kumar 2014 | Non-RCTa | 200mg, daily | 224 | 72/65 | 50/53 | 40/102 | NA |
| Moreiras-Plaza 2007 | Non-RCTa | 100mgc | 166 | 50/44 | 50/46 | 131/121 | 2269/1450 |
| Morey 2001 | Non-RCTa | 50mg, daily | 123 | 53/25 | 54.5/53.5 | 103/76 | 1690/595 |
| Restrepo 2010 | RCT | 200mg, EOD | 226 | NA | NA | 210/210 | NA |
| Wadhwa 1996 | Non-RCTa | 100mg, EODd | 234 | 71/77 | 53.8/48.8 | 95/105 | 1832/1705 |
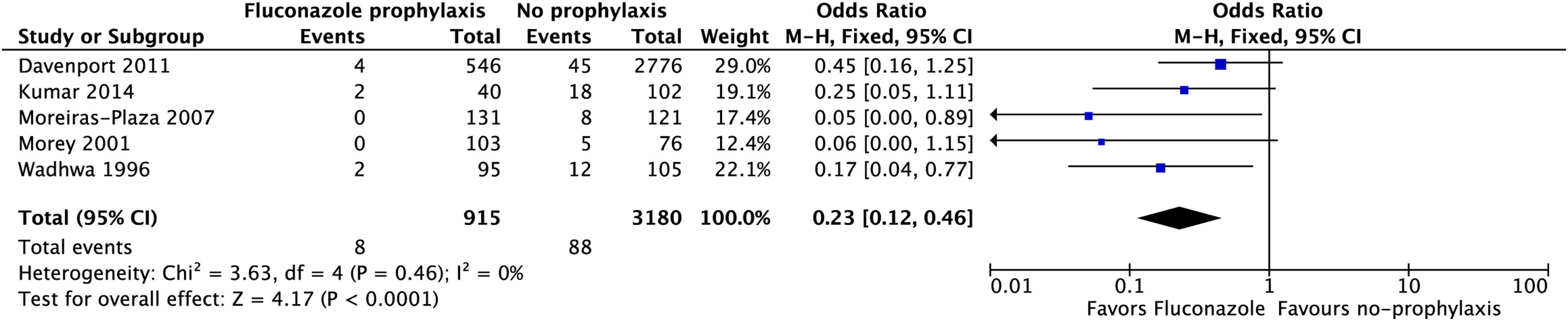
Patients receiving fluconazole had a significantly lower incidence of FP (1.0%) as compared with those who did not receive prophylaxis (3.0%) during an episode of peritonitis with antibiotic exposure (OR 0.22; 95% CI 0.12–0.41; p<0.001; I2=0%; Fig. 2). In a subgroup analysis of studies using daily dose of fluconazole, there was also a significant reduction in the incidence of FP in those who received fluconazole (OR 0.31; 95% CI 0.14–0.69; p=0.004; I2=0%; Fig. 3). In a subanalysis restricted to observational studies, the incidence of FP was also significantly lower in fluconazole-treated individuals (OR 0.23; 95% CI 0.12–0.46; p<0.01; I2=0%; Fig. 4). Leave-one-out sensitivity analyses confirmed the consistency of results after removing each study sequentially and recalculating results. The OR remained statistically significant, ranging from 0.15 to 0.25, when each study was systematically withdrawn from the analysis.
The RCT was appraised using the Cochrane Collaboration's tool RoB-2, and it was considered to have a low risk of bias in all the domains accessed (Table S1). In this study, patients and investigators were unblinded. All five nonrandomized publications achieved ≥7 points in the NOS. A funnel plot analysis of the primary outcome showed a symmetric distribution of studies with similar weights and point estimates that converged toward the pooled treatment effect as weight increased, indicating no evidence of publication bias (Fig. 5).
DiscussionThis systematic review and meta-analysis including 6 studies and 4515 episodes of peritonitis compared the efficacy of fluconazole prophylaxis with no prophylaxis in patients on PD upon antibiotic exposure for treatment of peritonitis. The main findings from the pooled analyses showed that fluconazole significantly reduced the risk of FP to one-third of that in the no prophylaxis group (1% vs. 3%, respectively). Moreover, this finding was robust and remained significant in leave-one-out sensitivity analyses and exploration of subgroups, including data restricted to daily fluconazole dosing and observational studies.
Most FP events are preceded by antibiotic exposure, either for PD-related infections, such as peritonitis, exit-site infection, or tunnel infection, or for other common clinical bacterial infections.29 A previous metanalysis of RCTs showed a significantly lower risk of fungal peritonitis when compared with placebo/no prophylaxis (RR 0.28; 95% CI 0.12–0.63).2 However, that prior meta-analysis included only two RCTs, with different antifungal regimens, specifically nystatin13 or fluconazole.23 Our meta-analysis builds on prior results by showing evidence of benefit from fluconazole specifically in this patient population.
Interestingly, observational studies were not included in the prior meta-analysis.24–28 This is notable because these studies had mixed and conflicting results for this intervention, creating uncertainty in the literature as to the benefit of fluconazole prophylaxis in the prevention of FP in patients with peritonitis. However, our results found a significant reduction in FP with fluconazole therapy even among the subgroup restricted to observational studies. The low heterogeneity (I2=0%) of this analysis indicates that the observational studies were consistent with each other, but likely underpowered to show a statistically significant benefit, which becomes evident in the pooled analysis of these studies (Fig. 4).
The ISPD 2022 expert consensus statement on peritonitis recommends anti-fungal prophylaxis whenever PD patients receive an antibiotic course, regardless of the indication for that antibiotic course (level 1B of evidence).1 This recommendation has no preference for either nystatin or fluconazole, with the latter being recommended at a dose of 200mg every 48h. The 2022 guideline from the Sociedad Española de Nefrología supports the use of fluconazole for prophylactic purposes in this scenario, but it does not provide information on the dosage for its use.19 The PDOPPS cohort conducted a prior study which revealed a noteworthy variance in antifungal prophylaxis utilization across various countries. Routine use of antifungal prophylaxis was observed in Australia and New Zealand, while Japan, Thailand, and the United Kingdom exhibited minimal usage.30 Although the doses and posology of fluconazole varied among the studies included in this meta-analysis, a subgroup of studies that used daily fluconazole also found a significant reduction in the incidence of FP in those who received prophylaxis with fluconazole.24,25,27 After conducting our study, we strongly suggest following the current guidelines and administering antifungal prophylaxis with fluconazole when a patient on peritoneal dialysis is being treated with antibiotics, with the dose of 200mg on alternate days being a well-established scheme for this purpose.
Our study has some limitations. First, most of the included studies were not randomized, which adds risk of bias related to confounding factors. However, the results of observational studies and the RCT were consistent with each other, with a low heterogeneity between studies (I2=0%). Also, sensitivity analyses confirmed consistency of study results after removing each individual study. Second, there was a variation in the dose of fluconazole prescribed by different studies. Third, the absence of patient-level data precluded evaluating additional outcomes, such as need to transition to hemodialysis, hospitalizations, and mortality. Whether fluconazole prophylaxis reduces these endpoints in PD-related peritonitis remains a gap in the literature. Finally, four studies used historical controls for the control group (no prophylaxis). Whether other concomitant interventions were distributed unevenly between patients treated with vs. without fluconazole prophylaxis is unclear.
ConclusionIn this meta-analysis including 4515 episodes of peritonitis in patients on PD, prophylaxis with fluconazole was associated with a significant reduction in the incidence of FP as compared with no antifungal prophylaxis. Given the potential implications of FP, the low cost of fluconazole, and its safety profile, this agent should be considered as standard-of-care in patients with PD-related peritonitis. Future research should evaluate the role of fluconazole prophylaxis in patients on PD who are treated with antibiotic therapy for other, non-peritonitis, bacterial infections.
Funding sourcesThe authors report no funding sources for this manuscript.
Conflict of interestAll authors report no relationships that could be construed as a conflict of interest. All authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
We acknowledge the constant drive of our team to improve patient care at Ana Nery Hospital. We would also reckon the aid of Dr. Rhanderson Cardoso for this manuscript, been a constant inspiration and educator on medical research.