Hepatitis B virus (HBV) reactivation in kidney transplant recipients (KTR) involves important morbidity and mortality. Despite being more common in patients who are HBsAg-positive, it may occur in patients with clinically resolved infection (HBsAg-negative and anti-HBc-positive), in whom the presence of the protective anti-HB antibody is thought to decrease the risk of reactivation. Data regarding reactivation rates in this population are scarce.
ObjectiveTo retrospectively evaluate the risk of HBV reactivation in KTR with previously resolved infection.
Material and methodsRetrospective cohort study including patients who underwent a kidney transplant between January 1994 and December 2014 with resolved HBV infection at the time of transplantation (anti-HBc seropositivity without detectable HBsAg, with or without anti-HB-positive antibodies and normal liver enzymes).
ResultsOut of 966 patients, 95 patients with evidence of resolved HBV infection were analyzed, of which 86 had a titer of anti-HBs >10mIU/ml. Mean follow-up time was 93 months; 12 patients had lost anti-HBs. Two patients showed evidence of reactivation. Risk factors associated with loss of anti-HBs were elderly age (>60) and occurrence of acute graft rejection (p<0.05).
ConclusionThe risk of HBV reactivation in KTR with previously resolved infection is not negligible at 2%. Elderly age and acute rejection were associated with loss of anti-HBs, and these patients may benefit from closer monitoring of HBV DNA levels. Routine serology and/or HBV viral load monitoring in HBsAg-negative, anti-HBc-positive patients is recommended and should be emphasized in these patients.
La reactivación del virus de la hepatitis B (VHB) en receptores de trasplante renal (RTR) supone una importante morbilidad y mortalidad. A pesar de ser más frecuente en pacientes con HBsAg positivo, puede suceder en pacientes con infección clínicamente resuelta (HBsAg-negativo y anti-HBc-positivo). En estos casos, la presencia del anticuerpo protector anti-HBs parece disminuir el riesgo de reactivación. Existen escasos datos relativos a las tasas de reactivación en esta población.
ObjetivosEvaluación retrospectiva del riesgo de reactivación del VHB en RTR con infección previa resuelta.
Material y métodosEstudio de cohorte retrospectivo, incluyendo RTR entre enero de 1994 y diciembre de 2014, con infección VHB resuelta en el momento del trasplante (anti-HBc seropositivo, HBsAg indetectable, con o sin anticuerpo anti-HBs e enzimas hepáticas normales).
ResultadosDe un total de 966, 95 pacientes con evidencia de infección VHB resuelta fueron analizados; 86 tenían un título de anti-HBs>10mIU/ml. El tiempo medio de seguimiento fue de 93 meses, 12 pacientes habían perdido anti-HBs. Dos pacientes tuvieron evidencia de reactivación. Los factores de riesgo asociados a la pérdida de anti-HBs fueron la edad avanzada (>60) y la evidencia de rechazo agudo del injerto (p<0,05).
ConclusiónEl riesgo de reactivación del VHB en RTR con infección previamente resuelta (2%) no es despreciable. La edad avanzada y el rechazo agudo están asociados a la pérdida de anti-HBs, y estos pacientes podrían beneficiarse de una vigilancia de los niveles de DNA del VHB. Las serologías de rutina y/o la monitorización de la carga viral en pacientes HBsAg-negativo, anti-HBc-positivo está recomendado y debería ser enfatizado en estos pacientes.
Hepatitis B virus (HBV) infection has decreased in frequency in kidney transplant recipients (KTR) due to the reinforcement of vaccination policies in the Chronic Kidney Disease (CKD) population and increased precautions to prevent transmission of the HBV among dialysis patients.1 Reactivation of HBV infection in KTR is associated with important morbidity and mortality.2 Immunosuppressive (IS) drugs used to prevent graft rejection blunt B and T cell functions and that permits HBV replication and viral protein expression on the surface of the infected hepatocytes.3 Reactivation is more frequent in patients who are HBsAg-positive, but it can also occur in patients with resolved HBV infection (HBsAg-negative and anti-HBc-positive), since the virus can still replicate within the hepatocytes.4,5 Data are scarce and conflicting regarding the risk of HBV reactivation in this subset of patients. Reported rates of reactivation are variable; while some authors claim that the risk is negligible regardless of anti-HBs status,6 others have published rates ranging from 1 to 6.5%.7,8 It has been suggested that in these patients the presence of anti-HBs antibodies may provide protection against HBV reactivation8–10 but there are too few data about the proportion of renal transplant patients with resolved HBV infection and with positive anti-HBs titers that lose immunity during follow-up.11 Thus, it remains unclear regarding what kind of monitoring is needed and whether these patients would benefit from antiviral prophylaxis during the post-transplant period.
In this study we aim to retrospectively evaluate the risk of HBV reactivation in KTR with previously resolved infection in a Portuguese Kidney Transplant Centre.
Material and methodsStudy populationWe designed a retrospective cohort study enrolling all consecutive patients who underwent a kidney transplant at our center in the period between January 1994 and December 2014 who had serological evidence of resolved HBV infection at the time of transplantation. Patients were followed until September 30th, 2015.
Resolved HBV infection was defined as seropositivity for anti-HBc without detectable HBsAg, and normal liver enzymes (ALT, AST), with or without anti-HBs positive titers.
Cutoff for positive anti-HBs was defined as >10mIU/ml and loss of immunity was defined by fall of anti-HBs to levels bellow 10mIU/ml and reactivation was defined according to current guidelines by a viral load >2000IU/ml.12
Exclusion criteria were: no information regarding viral status at the time of transplant, if they had a positive HBsAg, primary non-functioning allograft, and allograft survival less than 30 days.
Acute rejection (BPAR) was defined by biopsy-proven histological changes compatible with either cellular or antibody-mediated rejection according to the latest Banff classification update available at the time of diagnosis.
Analyzed dataData were collected from the patients’ medical records. Demographic data included age, sex, time on dialysis, cause of CKD and number of previous transplants.
Data regarding HBV serological status, IS regimen, use of antiviral prophylaxis, and occurrence of acute rejection were collected.
In the evaluation of kidney transplant candidates and upon admission for renal transplant, liver enzymes (ALT, AST) and routine HBV serological markers were obtained from all transplant candidates. Our transplant center did not test HBV viral load in KTR with resolved HBV infection, and post-transplant serological HBV testing did not follow a systematic protocol, thus, the frequency of monitoring was left at the discretion of the attending Nephrologist. All patients’ post-transplant serological markers were recorded during the follow-up monitoring; the date of reactivation or the date of the last serological testing, whichever came first, was considered the end of follow-up. The follow-up appointments were scheduled according to our Institution's protocol but could be adjusted by the Nephrologist according to the patient's clinical status. Serological markers were obtained using hemi luminescent methods (Prism HBsAg® and Prism HBcore®, Abbott; Architect Anti-HBs®, Abbott), and HBV DNA was obtained using multiplex nucleic acid test, COBAS® TaqScreen MPX Test, version 2.0, Roche.
Statistical analysisDescriptive statistics were recorded as median and interquartile range (IQR) intervals. Univariate analysis was performed using Cox regression analysis; covariates with p<0.1 were tested in a gender-adjusted multivariate model. Cox multiple regression analysis using the forward conditional method was performed to assess independent risk factors for loss of anti-HBs, and significance was considered if p<0.05. Statistical analysis was performed using IBM SPSS version 23 (IBM Corp. Released 2016. Armonk, NY: IBM Corp).
ResultsPatient dataFrom the 1151 kidney transplant recipients performed during the study period the following were excluded: 137 without record of HBV serological status, 7 HBsAg-positive patients, 28 with primary graft failure and 13 patients with graft survival <30 days. From the remaining 966 patients, 867 were anti-HBc negative and the remaining 99 patients had evidence of resolved infection at the time of surgery.
Four of the 99 patients had no information regarding post-transplant serological data and thus were excluded from the analysis. Of the remaining ninety-five patients, nine had anti-HBs <10mIU/ml.
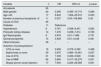
Baseline characteristics of the study population are shown in Table 1.
Baseline characteristics of the study population. Values are medians and interquartil ranges unless indicated otherwise.
| Patient characteristics | N | Value |
|---|---|---|
| Recipient age (years) | 95 | 50 [42–59] |
| Recipient sex, n (%) | 95 | |
| Male | 33 (34.6) | |
| Female | 62 (65.3) | |
| Cause of chronic kidney disease, n (%) | 95 | |
| Glomerulonehpritis | 15 (15.8) | |
| Polycystic kidney disease | 14 (14.8) | |
| Diabetic nephropathy | 11 (11.6) | |
| Nephroangiosclerosis | 8 (8.4) | |
| IgA nephropathy | 8 (8.4) | |
| Other | 10 (10.5) | |
| Unknown | 29 (30.5) | |
| Graft rank, n (%) | 95 | |
| First transplantation | 84 (88.4) | |
| Retransplantation | 11 (11.6) | |
| Donor type, n (%) | 95 | |
| Deceased | 93 (97.9) | |
| Living | 2 (2.1) | |
| Time on dialysis (months) | 95 | 38.5 [23.8–83.3] |
| Type of dialysis, n (%) | 95 | |
| Hemodialysis | 86 (90.5) | |
| Peritoneal dialysis | 9 (9.5) | |
Patients were followed at our Outpatient Clinic for a median time of 93 months (IQR=58–146). Follow-up time did not differ significantly between patients who lost anti-HBs compared to those who did not (median follow-up time 68 vs 73 months, p=0.789). In patients who lost anti-HBs compared to those who did not 5 and 10 year patient survival rates were 93.9% and 89.9%, while 5 and 10 year allograft survival rates were 95.95% and 90.9%, respectively. During the study period, 13 patients died with a functioning allograft and 14 lost graft function.
Seventeen cases of BPAR were recorded, nine of which were treated with pulses of metilprednisolone (MPD); 1 with MPD plus intravenous immunoglobulin, 5 with anti-thymocyte globulin (ATG) and 1 with MPD plus ATG. Treatment was not known in the remaining case.
ImmunosuppressionIS regimens used at the time of transplantation and at the date of the last follow-up are presented in Table 2. Most patients were treated with a triple drug regimen; additionally, induction imunosuppression consisted of basiliximab in 30 patients (31.6%), ATG in 17 (17.9%) and daclizumab in 2 (2.1%).
Immunosuppressive regimens upon transplantation and at the end of follow-up.
| IS regimen | At the time of transplantation, n=95 | At the end of follow-up, n=68 |
|---|---|---|
| TAC+MMF+prednisolone, n (%) | 34 (35.8) | 33 (48.5) |
| CsA+MMF+prednisolone, n (%) | 46 (48.4) | 26 (38.2) |
| CsA+Aza+prednisolone, n (%) | 14 (14.7) | 2 (2.9) |
| Sirolimus+MMF+prednisolone, n (%) | 1 (1.1) | 0 |
| Everolimus +prednisolone, n (%) | 0 | 4 (5.9) |
| Other, n (%) | 0 | 3 (4.4) |
CsA: ciclosporin A, TAC: tacrolimus, AZA: azathioprine, MMF: mofetil mycophenolate. During the follow-up period, 13 patients died and 14 lost their allograft and were therefore excluded.
Twenty-one patients received ATG as induction therapy or as part of acute rejection treatment. At the end of follow-up all patients were on a low-dose steroid regimen consisting of 5mg of prednisolone or equivalent per day.
From the initial cohort of 99 patients, we were able to collect data regarding previous antiviral treatment on 88 patients (88.9%), confirming that none of those had been treated for HBV, having had spontaneous negativation of HBsAg.
None of the patients had a history of HBV antiviral prophylaxis or use of rituximab.
Loss of immunity and reactivationDuring the time of follow-up 95 patients had 339 HBV serological tests, which corresponded to a median of 3 tests per patient (IQR 1–5), or 0.44 tests per patient-year. Twelve patients (13.9%) lost immunity and two patients (2%) showed evidence of reactivation.
The first case was a 67 year-old male who had received a cadaveric allograft in 2007; at the time of transplantation anti-HBc and anti-HBs were positive (7.74 and 986mUI/ml, respectively). Immunosuppression consisted of a triple regimen of cyclosporine, MMF (mycophenolate mofetil) and prednisolone. No major complications occurred until 2013, when he was admitted with a history of cough and weight loss. Aspergilus fumigatus was isolated in a Bronchoalveolar sample and itraconazol was started. Two weeks later, liver enzymes levels increased; itraconazol toxicity was suspected and the drug was stopped. HBV serological markers were compatible with reverse seroconversion with reappearance of HBsAg, and reactivation was diagnosed as the patient had a viral load of 1.7×108IU/ml. Anti-HBs titer was 50.7mUI/ml. Liver biopsy showed mild cholestasis, inflammatory infiltrate, ground-glass hepatocytes, nuclear expression of HBcAg and absence of HBsAg. The patient was started on entecavir, but expired a week later due to acute liver failure.
The second patient was a 42 year-old male who had received its 3rd transplant from a deceased donor in 2006; at the time of transplantation anti-HBc was 10.7mIU/ml and anti-HBs was 2.67mIU/ml. Induction immunosuppression included ATG and maintenance imunosuppression consisted of tacrolimus, MMF and prednisolone; baseline creatinine was 3.5mg/dl. He was admitted with Pneumonia in 2014. Upon admission, liver enzymes were increased. HBV serological markers showed evidence of reverse seroconversion with reappearance of HBsAg, and reactivation was diagnosed as the patient had a viral load of 1.6×104IU/ml. Anti-HBs was 1.6mIU/ml. Entecavir was started with disappearance of HBsAg and viremia, which became undetectable. At the time of discharge serum creatinine was 4mg/dl. The patient lost his graft 10 months later due to chronic allograft nephropathy and restarted hemodialysis.
Of the 12 patients who lost immunity during follow-up, the choice of IS drug did not seem to have any impact. Particularly, the use of MMF and use of ATG were not associated with loss of immunity (p=0.241 and 0.524, respectively) (table 3). In the multivariate model adjusted for gender, older age (>60 years-old) was associated with loss of immunity (HR 4.853, p=0.024, CI [1.235; 19.071[) as was the presence of BPAR (HR 5.921, p=0.015, CI [1.416; 24.759[).
Risk factors associated with loss of immunity (univariate analysis).
| Variable | n | HR | 95% CI | p value |
|---|---|---|---|---|
| All patients | 95 | |||
| Male gender | 62 | 2.299 | 0.493–10.710 | 0.289 |
| Age >60 | 17 | 6.943 | 1.904–25.310 | 0.003 |
| Number of previous transplants >0 | 11 | 0.037 | 0.00–109.989 | 0.42 |
| Cause of CKD | 95 | |||
| Diabetes | 11 | Reference | ||
| Hypertension | 8 | 0.761 | 0.069–8.431 | 0.824 |
| Policystic kidney disease | 14 | 1.276 | 0.226–7.214 | 0.783 |
| IgA Nephropathy | 8 | 0.678 | 0.61–7.486 | 0.751 |
| Glomerulonephritis | 15 | 0.459 | 0.61–3.449 | 0.451 |
| Other/Unknown | 39 | – | – | – |
| Induction imunossupression | ||||
| ATG vs none | 16 | 0.636 | 0.075–5.392 | 0.468 |
| Basiliximab vs none | 30 | 3.975 | 0.960–16.461 | 0.057 |
| Use of ATG | 21 | 1.549 | 0.403–5.949 | 0.524 |
| Use of MMF | 85 | 3.690 | 0.417–32.279 | 0.241 |
| Biopsy-proven acute rejection | 17 | 7.944 | 2.223–28.389 | 0.001 |
HBV reactivation is a potentially fatal condition with mortality rates reported as high as 25%.4 In our study the rate of HBV reactivation in patients with previously resolved infection was approximately 2%, resulting in death in one patient. This highlights the importance of assessing potential risk factors for reactivation since prophylaxis can prevent its occurrence.
Only 4 retrospective studies addressed the risk of reactivation in HBsAg-negative and anti-HBc-positive KTR.7–9,13 The number of patients was small and reactivation rates varied from 0 to 6.5%. Risk factors for reactivation included older age, presence of rejection, use of rituximab and loss/absence of anti-HBs, but findings were not consistent among the 4 studies possibly due to the small number of cases in each study. We found that 13.9% of the patients with resolved HBV infection and positive anti-HBs titers lost immunity. In our series, older age and presence of BPAR were independent risk factors for loss of anti-HBs, which in its turn might increase the risk of reactivation. Age can be a risk factor since older patients tend to produce weaker immunological response and tend to have lower levels of anti-HBs.8 Acute rejection is thought to be a risk factor through an increase of immunosuppression used for its treatment and this has been confirmed in other solid-organ transplants (SOT).8
It is postulated that IS agents such as B-Cell depleting drugs like rituximab are associated with a high risk of HBV reactivation even in patients with resolved HBV infection.4,13,14 In our study, none of our patients had received rituximab. Relationship between other drugs used in kidney transplantation and reactivation is less consistent.8,15 We found no association between the type of IS drug used and loss of anti-HBs.
Our study is limited by its retrospective nature, and we are unaware of when the patients included in our study acquired HBV infection and the timing of their acquisition of positive anti-HBs titers after the infection. We were also unable to assess previous HBV vaccination history. Both could influence anti-HBs titers and the risk of HBV reactivation after renal transplantation, although there are no studies addressing this issue.
The retrospective nature of our study and the absence of HBV genotype testing in our reactivation cases do not allow us to completely rule out the possibility of re-infection instead of reactivation. However, both patients were diagnosed in an inpatient setting and none had recent history of high risk behavior or contact with blood products. Besides, both were highly immunosuppressed – one of the patients had a severe opportunistic infection and the other a high cumulative IS load given the history of 3 transplants, which favors the hypothesis of reactivation.
Our transplant center did not test HBV viral load in KTR with resolved HBV infection, and serological HBV testing did not follow a systematic protocol. This way, we cannot assure that asymptomatic reactivations might have been missed during the follow-up period, and this way we might have underestimated the reactivation rates in our population. At last, the small number of reactivation cases did not allow us to infer about potential risk factors for reactivation. Our study however has some specific strengths; in an era of declining HBV incidence in the Western Countries, we have managed to retrieve a fairly high number of patients and a long term follow-up.
The American Association for the Study of Liver Diseases recommends routine use of appropriate antiviral prophylaxis in all patients who are HBsAg-positive prior to or at the initiation of chemotherapy, immunosuppressive therapy, hematopoietic stem cell transplantation, or solid organ transplantation.12 When B-cell depleting agents like rituximab are used in patients with resolved infection (HBsAg-negative, anti-HBc-positive) antiviral prophylaxis can be anticipated to result in similar risk reduction of HBV reactivation as described for HBsAg-positive patients,14 otherwise recommendations regarding antiviral prophylaxis in KTR with resolved HBV infection are lacking. Current guidelines do not recommend using anti-HBs titer to guide initiation of prophylaxis since there is no threshold level that universally prevents HBV reactivation.10,12,14 However, anti-HBs titer is still believed to confer protection against reactivation.8,13,16 Considering that loss of anti-HBs increases the risk of reactivation,7,8,17,18 patients who are at increased risk of anti-HBs loss, such as older patients and those with BPAR as found in our study, might benefit from closer surveillance of HBV DNA levels4,10,19 or even antiviral prophylaxis. Although evidence is scarce regarding HBV DNA monitoring in patients with resolved HBV infection we suggest, as a cost-effective measure, a baseline measurement of HBV DNA levels for all candidates to kidney transplantation with resolved HBV infection (anti-HBc positive, HBsAg negative) to exclude occult viral replication. For those with positive HBV DNA we suggest antiviral prophylaxis starting from the time of transplantation and follow-up with periodical assessment of aminotransferases and HBV DNA levels. If the initial baseline HBV DNA is negative, we suggest serological HBV follow-up (HBsAg and anti-HBs) and close monitoring of aminotransferases levels. In case of HBsAg seroreversion or elevated aminotransferases, we suggest HBV DNA assessment. However, even with negative baseline negative HBV DNA; we acknowledge that some of these patients, especially if they are at higher risk of reactivation, might benefit from HBV DNA surveillance from the time of transplantation. In our study the small number of cases of HBV reactivation precludes any conclusion, and further studies are needed.
ConclusionsIn conclusion, the risk of HBV reactivation in KTR with previous clinically resolved infection is not negligible at 2%. Older age and acute rejection were associated with loss of anti-HBs, and these patients might benefit from closer surveillance of HBV DNA level. Routine serological and/or HBV viral load monitoring in HBsAg-negative, anti-HBc-positive patients is recommended and should be emphasized in these patients.
Author contributionsMeng C: design of study, data collection, drafting article. Belino C, Pereira L, Sampaio S, Tavares: data analysis, drafting article. Pinho A: critical revision and statistical analysis. Bustorff M: design of study, drafting and critical revision. Sarmento A and Pestana M: critical revision.
Conflict of interestThe authors declare no conflict of interest.