Familial steroid-resistant nephrotic syndrome (SRNS), also known as nephrotic syndrome, type 2 is defined as early onset proteinuria in childhood with hypoalbuminemia, hyperlipidemia, and edema that rapidly progress to end stage renal disease (ESRD), not respond to steroid therapy. The syndrome is mostly observed between three months and five years of age,1,2 while often progresses to chronic kidney disease (CKD) requiring dialysis.3
Familial SRNS is an autosomal recessive disorder, caused by mutations in the NPHS2 gene (PODOCIN), encodes podocin that contribute in stabilization of slit diaphragm assembly, the structural and functional integrity that for normal glomerular permeability is essential.2,4
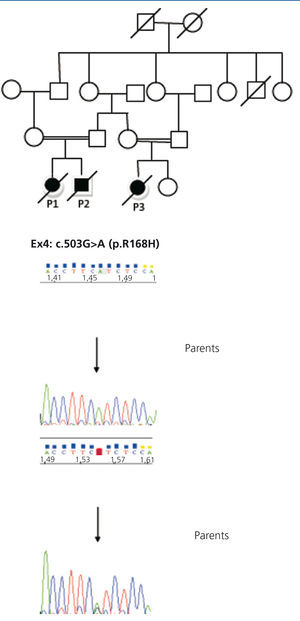
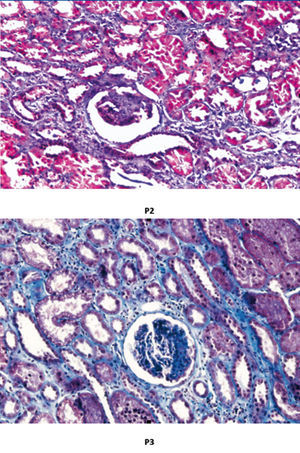
Herein, an Iranian family is presented here with three affected children with nephritic syndrome (Figure 1). An 8-years old boy (P1) was referred to the Children’ Medical Center Hospital (Tehran, Iran), with ESRD at the age of 8 years. There was history of death due to ESRD in his sibling. His sister (P2) had suffered from generalized edema since 8-month old. Urine analysis showed protein of 7.5g/dL and RBC of 8-10. Ultrasonography and DMSA showed single right kidney. Kidney biopsy indicated diffuse mesangial sclerosis (Figure 2). She was resistant to therapy and developed ESRD in 6th year of life and subsequently died 5 months later.
The index case (P1) had history of hospital admission because of anasarca edema at the age of 3 years. Urine analysis yielded protein of 1960mg/day, creatinine (Cr) of 128mg/mg and microscopic hematuria. Serum Cr level was 0.4mg/dL, GFR of 134mL/min/1.73, serum total protein of 3.68g/dL, and serum albumin of 1.69g/dL. Hypercholesterolemia (Chol=590mg/dL) and hypertriglyceridemia (TG=670mg/dL) were also detected. Although 2mg/kg prednisolone had been advised for the patient, he did not use it regularly. Therefore he was admitted with hypocalcaemia, laryngospasm and hypertension due to ESRD. He was put on hemodialysis, but he developed sagittal sinus thrombosis after 8 months; anticoagulant was started, but unfortunately he experienced intractable seizure after one month and subsequently died.
Six months after admission of P1 at our hospital, his cousin was also referred to our hospital with ESRD. She was diagnosed with nephrotic syndrome since 2 years prior to admission. She was manifested with generalized edema, vomiting and diarrhea. Urinalysis revealed protein 1.6g/d, RBC: Many. BUN was 5mg/dL, Cr level was 0.2mg/dL, total protein: 4.6g/dL, albumin: 1.5g/dL, Chol: 591mg/dL, and TG: 1,374mg/dL. Steroid and cyclophosphamide were advised, but she did not respond; her family did not comply with further medications. Kidney biopsy showed FSGS changes (Figure 2). She underwent hemodialysis for 6 months, but unfortunately she died because of sepsis in 5th year of life.
As of strong family history of nephritic syndrome, genetic tests were done on P1 and P3. The exons and flanking intronic regions of the genes [NPHS2 exons 1-8 and PLCE1 exons 2-32] were amplified by PCR. PCR amplicons were purified and subjected to direct sequencing using an automated capillary sequencer. Sequences were compared to the reference sequences deposited in the public database (NCBI). In the sample derived from two affected cousins of the family homozygosity for two sequence changes of the gene NPHS2 was demonstrated. Direct sequencing of all 8 exons of the NPHS2 (Podocin) gene have been performed for the index case. In exon 4 of the NPHS2 gene, c.503G>A X R168H homozygous mutation was found (Figure 1). Both parents of index case were heterozygous carrier with the same mutation compatible with recessive inheritance. These findings confirm the diagnosis of familial SRNS in this family.
The NPHS2 gene mutation leads to a variant of nephrotic syndrome that does not respond to steroid therapy, SRNS.4 Lack of effective treatment and poor prognosis of chronic renal insufficiency and ESRD, make SRNS a significant therapeutic dilemma for pediatricians and pediatric-nephrologists.5 In this study, an Iranian family of SRNS with 3 affected children was reported in which NPHS2 gene has been detected. This mutation has been defined previously.6 It is the first report of such mutation in an Iranian family. The NPHS2 allele harbouring these two variations in cis has repeatedly been found in patients with idiopathic nephrotic syndrome, particularly in the Turkish population.4,7
Histopathologic findings showed diffuse mesangial proliferation or minimal change lesions in the early phase and focal segmental glomerulonephritis, in the last phase of the disease. IgM and C3 deposits or both were described.1,8
These patients are mostly at risk of complications such as edema, infections, thromboembolic events, malnutrition, anemia, endocrine abnormalities, acute renal failure, hypertension, and impaired growth.5
For making a suitable therapeutic approach and avoiding unnecessary steroid therapy as well as prenatal diagnosis and selecting an unaffected living donor, genetic analysis for detecting possible podocin mutations is beneficial.8
Conflict of interest
The authors declare that there is no conflict of interest associated with this manuscript.
Figure 1. The pedigree of the family with familial steroid-resistant nephrotic syndrome
Figure 2. Renal biopsies of both cases shows segmental glomerular sclerosis and interstitial fibrosis with mild tubular dilatation (Trichrome staining, 400X)