Dear Editor,
Since, 1966 different reports have associated minimal change disease (MCD) with different immunogens1 as well as the presence of acute renal failure (ARF) in the MCD,2 which pathogenic mechanisms are being debated up to the present.
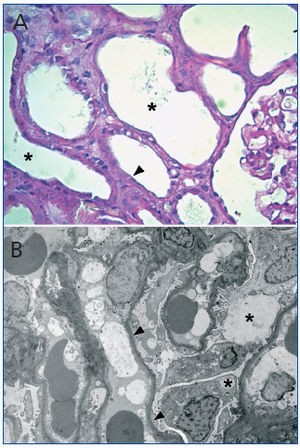
A 44-year old man was admitted to our hospital with edema in his face and legs and cervical lymphadenopathy which occurred 18 days after influenza vaccine (Agrippal®, Novartis). The laboratory showed: creatinine 44mg/l, urea 106mg/dl. In the urinalysis was evident: proteinuria 4g/24h and hyaline casts. Serological test (ANA, DNA, ANCAp, ANCAc, C3, C4, HBsAg, HCV and HIV) were negative. Renal biopsy was performed. Light microscopy showed evidence of severe acute tubular injury (Figure 1 A) and a moderate, diffuse interstitial inflammatory infiltrate consisting of mononuclear cells and severe edema. The immunofluorescence did not show deposits of IgG, IgA, IgM, C3 and C1q. Ultrastructural examination showed diffuse foot-process effacement, microvillous transformation and cytoplasmic vacuolization without basement-membrane remodeling (Figure 1 B). Minimal change disease, acute tubular injury, and moderate active interstitial nephritis were diagnosed. The patient started on oral prednisone (60mg/d), furosemide (80mg/d), enalapril (40mg/d), atorvastatin (20mg/d), Espironolactone-A (100mg/d), ranitidine 300 (mg/d) and low-sodium diet. The proteinuria (200mg/24h) and ARF (creatinine 1 mg/l), resolved rapidly.
Although, the pathogenic mechanisms proposed for MCD are not exactly known, some evidences suggest a T cells dysfunction with the production of a permeability factor. Moreover, it has been suggested a possible "cross-talk" between dendritic cells and Th lymphocytes with a consequent intrarenal cytokine production.3 In addition, both the modulation of the actin cytoskeleton at the glomerular diaphragm filtration level that induce by B7-1 expression,4 and the destabilization of the synaptopodin protein5 would be others probable causes of visceral epithelial injury.
On the other hand, it is unclear because patients with MCD may be more sensitive to develop ARF, compared to other nephrotic glomerulopathies. The mechanism underlying to this clinical-pathological entity has not been fully clarified. Several mechanisms attempt to explain the ARF in the nephrotic syndrome. The extensive interstitial edema observed in the present case, could lead to an increased intrarenal pressure and consequently explains the sharp drop in GFR observed in our patient. This finding is supported by one of the stronger hypothesis that explains this situation: nefrosarca hypothesis.6 Nevertheless, the hypothesis that links the ARF of nephrotic syndrome with changes in the coefficient of ultrafiltration should be considered.7 Finally, Chen et al. have hypothesized that cytokines secreted induce the production of endothelin-1, which generate contraction of mesangial cells resulting in a decrease of the filtration area.8
In summary, in the present case the immune response after influenza vaccination generated the podocitopathy known as minimal change disease possibly due to hypersesitivity syndrome. In this clinical-pathological context the patient developed acute renal failure which pathogenic bases are still controversial and debated in the biomedical area.
Acknowledgements
The authors wish to thank Mrs Elena Pereyra and Mrs Lucía Artino for their excellent technical assistance.
Conflict of interest
The authors declare that there is no conflict of interest associated with this manuscript.
Figure 1.