Chronic kidney disease (CKD) represents a great health care problem. It is associated with poor prognosis and a high risk of cardiovascular and renal complications, even in younger patients.1 As a result, early detection and prevention of progression of CKD to advanced stages should be considered a priority.2 CKD is classified based on cause, estimated glomerular filtration rate (eGFR) (G1–G5), and albuminuria categories (A1–A3), and is commonly defined as an eGFR <60ml/min/1.73m2 and/or elevated urine albumin-to-creatinine ratio (UACR) (≥30mg/g).2 Although previous studies have analyzed the prevalence of CKD in Spain,3,4 evidence from real-world data can provide a broader view of CKD impact and improve the understanding of its burden on healthcare systems.
We performed an observational, retrospective, and real-world data-based study using the BIG-PAC database. This database comprises information from 1.8 million persons of primary health centers and referral hospitals within 7 Autonomous Communities of the Spanish national health system.5 Adult subjects with at least one measurement of both eGFR and UACR in local laboratory tests closest to 1st January 2018 (up to 6 months) were included. The study population (n=70,973) was staged according to KDIGO definitions based on eGFR and UACR values.2 The study was approved by the Investigation Ethics Committee of Consorci Sanitari from Terrassa. No informed consent was provided, as this was a secondary data study and data were fully anonymized and dissociated from patients.2
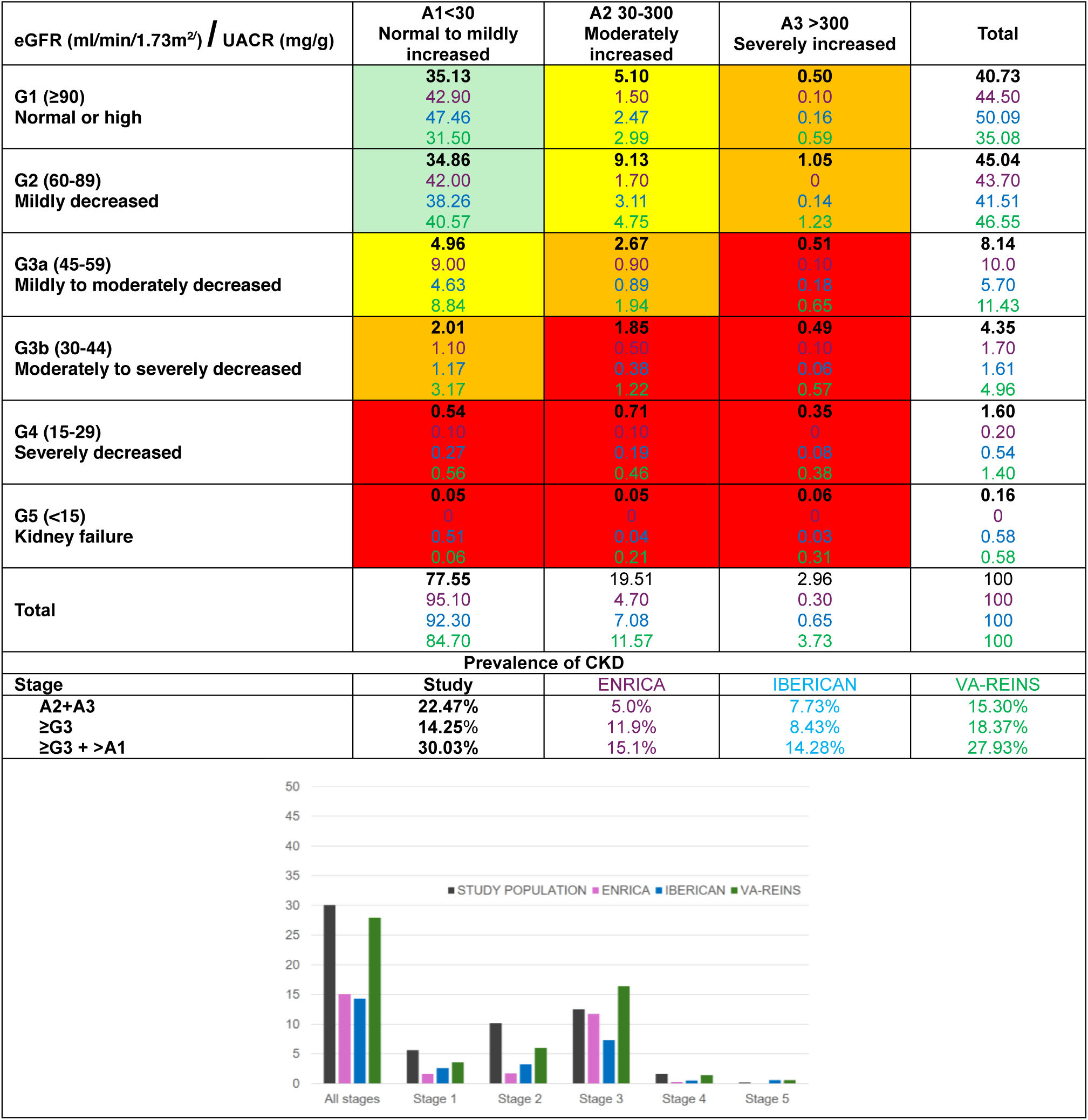
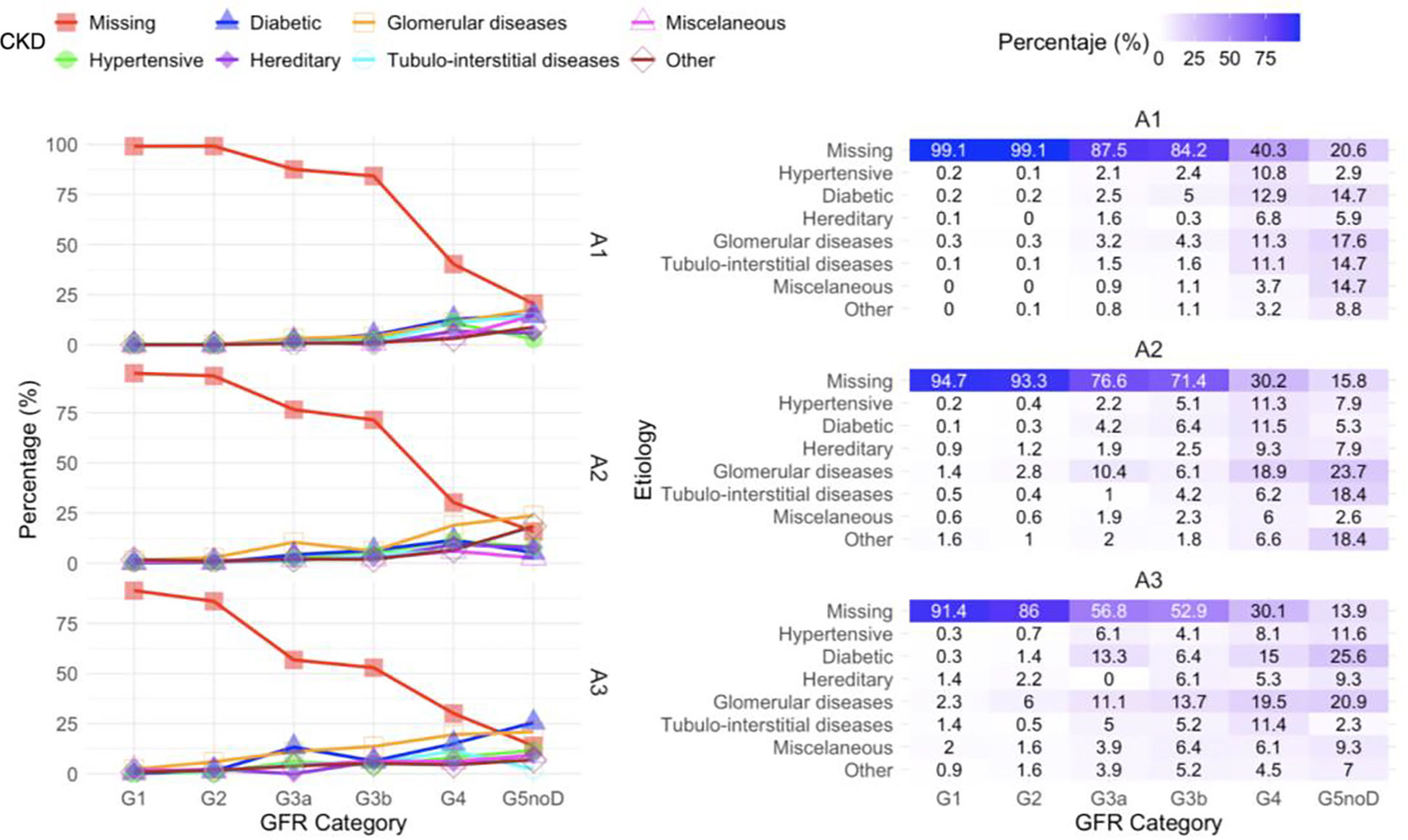
Overall, mean (SD) age was 64.16 (15.34) years, 48.8% were women, 32.0% had diabetes, and 19.7% cardiovascular disease. For the analysis of the proportion of patients classified according to eGFR and UACR (Fig. 1), those patients on renal replacement therapy at baseline (n=588; 0.83%) were excluded. Overall, 14.25% of patients had an eGFR <60ml/min/1.73m2, 22.47% albuminuria (19.51% 30–300mg/g and 2.96% >300mg/g), and 30.03% CKD defined by any of both criteria (30.86% if patients on renal replacement therapy had been included). Among patients with CKD (eGFR <60ml/min/1.73m2 or UACR >30mg/g or on renal replacement therapy), 82.04% did not have an etiological diagnosis code (Fig. 2).
Prevalence (%) of chronic kidney disease in our study population (excluding patients on renal replacement therapy at baseline), ENRICA, IBERICAN and VA-REINS studies.
Study: ENRICA4; IBERICAN5; VA-REINS.7
Green chart: low risk (if there are no other markers of kidney disease, nor CKD); yellow chart: moderately increased risk; orange chart: high risk; red chart: very high risk. GFR: glomerular filtration rate; eGFR: estimated glomerular filtration rate; UACR: urine albumin-to-creatinine ratio.
Our data showed that around 30% of patients with blood and urine tests collected in electronic health records had CKD. This number is quite higher than the prevalence previously reported in Spanish studies in the last years. ENRICA-RENAL was a Spanish population-based survey that evaluated 11,505 individuals, randomly selected from the general population, included between June 2008 and October 2010. In this study, 11.9% of patients had eGFR <60ml/min/1.73m2, 5.0% albuminuria, and 15.2% CKD defined by any of both criteria.3 IBERICAN was a multicenter cross-sectional study that recruited 7895 patients attending primary care settings from June 2014 and December 2018. These numbers in IBERICAN were 8.43%, 7.73% and 14.31%, respectively.4 By contrast, our figures were more in line with those of the VA-REINS study that included information from 7 million users of the national US Department of Veterans Affairs. In this study, the prevalence of CKD in 2014 was 27.93%.6
All these studies have relevant methodological differences, providing complementary information. ENRICA-RENAL and IBERICAN collected data from the general population and patients treated in primary care setting.3,4 However, in our real-world data study, patients had more comorbidities and greater access to healthcare. As a result, our study provides a clearer view of the real impact of CKD on the healthcare system in Spain.
On the other hand, our study showed that in clinical practice there is a low rate of CKD cause coding. This is mainly due to the fact that in routine practice, only those diagnoses that require hospital admission are coded, but not those in the earlier stages that are attended only in consultations. In this context, using real-world data together with advanced analysis strategies (business intelligence) will allow better planning and management of resources to treat CKD. Thus, automated systems and artificial intelligence will be helpful to solve problems due to lack of information in medical records, facilitating the early identification, risk stratification of CKD, and ultimately, to personalized medicine.7
In summary, 3 out of 10 patients with blood and urine tests collected in Healthcare Information Systems had CKD. To the best of our knowledge, this is the first study aimed to evaluate the real magnitude of CKD in Healthcare Information Systems in Spain, detecting gaps in information related to the coding of etiology. These findings strongly suggest that it is necessary a “call to action” to use the real-world information collected in information systems to better understand the real impact of CKD on health systems and plan efficient interventions against CKD.