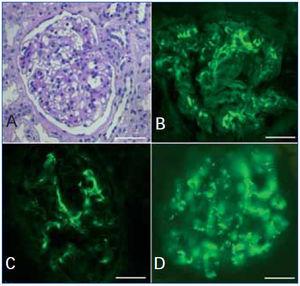
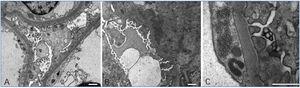
The classification of lupus nephritis was revised by the ISN/RPS in 2003. The increasingly recognized phenomenon of apparent minimal change disease (MCD) in the context of systemic lupus erythematosus (SLE), is not accepted in the above classification and is associated to a recent new pathological entity called lupus podocitopathy.1 A 32-year-old caucasian woman presented with arthralgia and swelling of the face, hands, and legs. Physical exam revealed pretibial edema and a patch of skin thickening on the left flank, consistent with morphea. Blood presure was 130/70mmHg; proteinuria 4.5g/dl; serum creatinine 0.9mg/dl; and albumin 2 g/dl. Urinalysis revealed fat casts. Serology was negative for hepatitis B, C, HIV-1 and HIV-2. ANA titer was 1/1300, C3 70mg/dl and anti ds-DNA was elevated. There was no history of nonsteroidal anti-inflammatory drug use in the patient. A diagnosis of SLE was made. Sections from the needle renal biopsy showed cortex with 10 normocellular glomeruli with mild mesangial hypercellularity and mesangial matrix increased. There were no evident tubular, interstitial, and vascular lesions (Figure 1 A). Immunofluorescence microscopy revealed mesangial granular deposition of IgG (2+) (Figure 1 B), IgA (1+), IgM (1+), C3 (2+) (Figure 1 C) and C1q (3+) (Figure 1 D). Ultrastructural analysis showed diffuse effacement (~80%) of the epithelial cell food processes and vacuoles (Figure 2 A). Moreover few electron-dense deposits were noted in mildly expanded mesangium (Figure 2 B). Subepithelial or subendothelial deposits were not observed in the biopsy. Numerous tubulorreticular inclusions within endothelial cells of glomerular capillary were also seen (Figure 2 C). A diagnosis of lupus podocytopathy and lupus nephritis Class I (ISN/RPS) was made. Of particular interest is the podocyte involvement in different types of lupus glomerulonephritis. For example, patients with non-nephrotic proteinuria and lupus nephritis Class I and II (ISN-RPS) have not revealed significant evidence of effacement of the foot processes. Nevertheless, some adult and children show minimal or proliferative mesangial lupus nephritis and nephrotic proteinuria without peripheral immune complex, exhibiting extensive podocyte effacement, consistent with lupus podocytopathy1. It is difficult to propose an exact pathogenic mechanism for this lesion given that immune deposits are no detected in glomerular basement membrane, even though it has been hypothesized different mechanisms. Abnormal release of IL-13 from aberrant T cell2, crosstalk between renal dendritic cells and Th cells3 may directly damage to podocytes. Our patient was treated with high-dose prednisone. Six month later she remained normotensive, had no edema, with normal serum creatinine and decreased urinary protein excretion (0,5g/d). In agreement with this result Kraft et al1 have shown a significant reduction in proteinuria at last follow-up. Therefore, the podocytopathy in the SLE context responded to oral corticosteroids, remarking the important therapeutic implications of the diagnosis of this particular entity. In summary, lupus podocytopathy has become an intersting point both clinical discussion and futures investigations about the role of podocyte and it should be added to the classification of lupus nephritis.
Conflict of interest
The authors declare that there is no conflict of interest associated with this manuscript.
Figure 1. Light microscopy and immunofluorescence findings
Figure 2. Ultrastructural findings