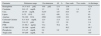
Chronic hypercalcemia can be an important complication of anabolic steroid and vitamin supplement abuse. We report the case of a 30-year-old bodybuilder that for more than 4 years used injectable anabolic-androgenic steroids (AAS) and one veterinary polyvitamin formulation with vitamin A (2,100,000IU), D (ergocalciferol: 60,000IU), and E (55IU) on a monthly basis. He also reported self-injecting mineral oil intramuscularly for esthetic purposes for more than 2 years. He presented to the emergency room with an acute, severe epigastric pain, associated with nausea and vomiting. Laboratory evaluation (Table 1) demonstrated an elevated amylase 2500IU/L (50–160IU/L); lipase of 612IU/L (0–75IU/L); a corrected serum calcium of 12.5mg/dL (8.5–10.5mg/dL); PTH of 73.2pg/mL (15–68.3pg/mL) and 25(OH)D of 65.1ng/mL (30–100ng/mL). Serum creatinine was 1.2mg/dL (0.6–1.2mg/dL). Abdominal ultrasound showed a diffusely edematous pancreas, bilateral ureterolithiasis and nephrocalcinosis. A high-resolution CT of the chest and abdomen was performed and revealed absence of granulomas and lymphadenopathies. He had a tormented clinical course, with acute kidney injury (attributed to volume depletion and renal vasoconstriction in the setting of hypercalcemia) without the need of hemodialysis; protracted vomiting that lead to a laparoscopic duodenum–jejunum anastomosis with improvement of complains and multiple infectious complications. Serum calcium and PTH returned to normal levels (9mg/dL and 35pg/mL, respectively) after vitamin D discontinuation, vigorous venous hydration with 0.9% saline infusion and therapy with furosemide and corticosteroids. After more than 60 days of hospitalization he was discharged home having made a full recovery.
Laboratory evaluation
| Parameter | Reference range | On admission | 48h | One week | Two weeks | At discharge |
|---|---|---|---|---|---|---|
| Hemoglobin | 14.3–18.3g/dL | 14.8g/dL | 13.1 | 13.6 | 12.9 | |
| Creatinine | 0.6–1.2mg/dL | 1.2 | 3.8 | 1.92 | 1.4 | 0.7 |
| Urea | 20–44mg/dL | 52.93 | 125 | 84.4 | 43 | 36 |
| Lipase | 0–75IU/L | 612 | 456 | 321 | 63 | |
| Amylase | 50–160IU/L | 2500 | 1430 | 234 | 88 | |
| Corrected Calcium | 8.5–10.5mg/dL | 12.5 | 12.3 | 11.1 | 9.0 | |
| Albumin | 2.9–5.2g/dL | 3.0 | 2.5 | 3.0 | 2.4 | |
| PTH | 15–68.3pg/mL | 73.2 | 70.2 | 38 | 35 | |
| 25-OH-VIT D | 30–100ng/mL | 65.1 | 56.2 | 69.7 | ||
| Phosphorus | 2.5–4.5mg/dL | 3.8 | 3.0 | 3.2 | 4.0 | |
| Triglyceride | 50–200mg/dL | 61 | 185 |
With the desire to improve performance, some athletes or amateurs use performance-enhancing drugs. The widespread use of these substances without medical prescription or clinical follow-up can lead to serious health problems as described on several reports.1–3 We believe that the main clinical features seen in this patient are due to chronic hypercalcemia due to multiple substance abuse and paraffinomas. The association between focal segmental glomerulosclerosis and anabolic steroids abuse may be explained by increase in lean body mass and potential direct nephrotoxic effects of anabolic steroids.1 Furthermore, this drug modulates steroid hydroxylase activity predisposing to hypercalcemia.4 The association of vitamin A toxicity and hypercalcemia is rare but well recognized. It is attributed to a direct effect on bone (activation of bone reabsorption with increased osteoclast activity),5 on the parathyroid, or in both.6 According to Chertow et al., vitamin A stimulate PTH secretion in bovine parathyroid tissue and in men.6,7 The minimum dose of vitamin A required to produce hypercalcemia cannot be stated with certainty; toxicity has been described from doses ranging from 50,000 to 500,000IU/day.5 Although we did not measure the value of vitamin A in blood, the patient injected more than 2,100,000IU/month (which correspond 70.000IU of vitamin A/day) for more than 4 years, which is compatible with toxicity. Hypercalcemia is a well-known but uncommon complication of vitamin D intake.8 Usually results from doses that exceed 10,000IU/day, and is generally associated with serum levels of 25-hydroxyvitamin D that are well above 150ng/mL.8 In this case, 60,000IU of ergocalciferol were inject monthly and serum vitamin D was in the upper limit of normal. The tolerable upper level of daily vitamin D intake recently set by the Institute of Medicine is 4000IU.8 Vitamin A and D can act synergistically to cause hypercalcemia. Contrary to what we were expecting, the patient described here presented with hypercalcemia and moderated increased serum PTH, instead of suppression of the activity of this hormone by multidrug and vitamin abuse. Multifactorial mechanisms may be involved and some possible explanations are: vitamin A intoxication may have had a leading role in the development of hypercalcemia and itself may increase PTH secretion6; parathyroid overactivity has been described in critical illness associated with sepsis and renal failure (life-threatening tertiary hyperparathyroidism).9 Primary hyperparathyroidism from adenoma or hyperplasia was excluded by negative imaging studies and the restoration of serum calcium and PTH to normal levels after discontinuation of the drugs. Finally, in the case reported here there was a peculiar involvement of the neck and the arms due to self-injection of mineral oil, more apparent after the significant weight loss observed (more than 30kg) by the patient (Fig. 1). Biopsy of the affected skin revealed multinucleated giant cells and inflammatory infiltrates. These lesions, called paraffinomas, may have contributed to hypercalcemia due to PTH-independent, extrarenal production of 1,25-dihydroxy-vitamin D by activated mononuclear cells.10
In conclusion, clinicians need to be aware that AAS and multivitamin abuse can occur with relative frequency and their use can be surreptitious. The simultaneous occurrence of nephrocalcinosis, nephrolithiasis, acute kidney injury and acute pancreatitis may be a clue to the diagnosis of associated chronic hypercalcemia.