Renalase, with possible monoamine oxidase activity, is implicated in degradation of catecholamines; which suggests novel mechanisms of cardiovascular complications in patients with chronic kidney diseases. Epicardial adipose tissue (EAT) has been found to correlate with cardiovascular diseases (CVD) in dialysis patients. The present study aimed to evaluate the association of serum renalase levels with EAT thickness and other CVD risk factors in peritoneal dialysis (PD) patients.
MethodsThe study included 40 PD patients and 40 healthy controls. All subjects underwent blood pressure and anthropometric measurements. Serum renalase was assessed by using a commercially available assay. Transthoracic echocardiography was used to measure EAT thickness and left ventricular mass index (LVMI) in all subjects.
ResultsThe median serum renalase level was significantly higher in the PD patients than in the control group [176.5 (100–278.3) vs 122 (53.3–170.0)ng/ml] (p=0.001). Renalase was positively correlated with C-reactive protein (r=0.705, p<0.001) and negatively correlated with RRF (r=−0.511, p=0.021). No correlation was observed between renalase and EAT thickness or LVMI. There was a strong correlation between EAT thickness and LVMI in both the PD patients and the controls (r=0.848, p<0.001 and r=0.640, p<0.001 respectively).
ConclusionsThis study indicates that renalase is associated with CRP and residual renal function but not with EAT thickness as CVD risk factors in PD patients.
La renalasa, posiblemente con actividad monoaminooxidasa, está implicada en la degradación de catecolaminas, lo que indica nuevos mecanismos de complicaciones cardiovasculares en pacientes con enfermedades renales crónicas. Se ha encontrado que el tejido adiposo epicárdico (TAE) se correlaciona con las enfermedades cardiovasculares (ECV) en pacientes de diálisis. El presente estudio tuvo como objetivo evaluar la asociación de los niveles de renalasa sérica con el espesor del EAT y otros factores de riesgo de ECV en pacientes de diálisis peritoneal (DP).
MétodosEl estudio incluyó a 40 pacientes de DP y a 40 controles sanos. Se tomaron la presión arterial y las medidas antropométricas de todos los individuos. Se evaluó la renalasa sérica mediante un ensayo disponible comercialmente. Se utilizó la ecocardiografía transtorácica para medir el espesor del TAE y el índice de masa ventricular izquierda (IMVI) en todos los individuos.
ResultadosLa mediana del nivel de renalasa sérica fue significativamente mayor en los pacientes de DP que en el grupo control (176,5 [100-278,3] frente a 122 [5,3-170,0] ng/ml) (p=0,001). La renalasa se correlacionó positivamente con la proteína C reactiva (r=0,705; p<0,001) y negativamente con la FRR (r=-0,511, p=0,021). No se observó correlación entre la renalasa y el espesor del TAE ni el IMVI. Hubo una fuerte correlación entre el espesor del TAE y el IMVI tanto en los pacientes de DP como en los controles (r=0,848; p<0,001 y r=0,640; p<0,001, respectivamente).
ConclusionesEste estudio indica que la renalasa está asociada con la proteína C reactiva y la función renal residual, pero no con el espesor del TAE, como factores de riesgo de ECV en pacientes de DP.
Cardiovascular disease (CVD), defined as the presence of either congestive heart failure, ischemic heart disease, or left ventricular hypertrophy (LVH), remains the leading cause of morbidity and mortality among patients with end stage renal disease (ESRD) treated with dialysis.1,2 In addition to conventional risk factors, these patients are exposed to kidney disease specific factors including uremic toxins, anemia, vascular calcification, endothelial dysfunction, oxidative stress and hypervolemia, which accelerate development of CVD.3 Recently, epicardial adipose tissue (EAT), the visceral adipose tissue surrounding the heart and subepicardial coronary vessels, has been found to correlate with several cardiac comorbidities, including coronary artery disease and left ventricular dysfunction in patients undergoing peritoneal dialysis (PD) or hemodialysis.4–6 The relation between EAT and CVD is not fully understood but has been attributed to the several proatherosclerotic and proinflammatory hormones and cytokines such as TNF-a, IL-6, and adipocytokines, which are secreted from EAT and influence cardiac function.5,7
Renalase, a recently discovered enzyme with monoamine oxidase activity, is implicated in degradation of catecholamines. This suggests novel mechanisms of cardiovascular complications in patients with chronic kidney diseases (CKD).8 Studies have demonstrated a stepwise increase in serum renalase concentration with higher stages of kidney disease and markedly increased serum renalase levels in patients with ESRD both on hemodialysis and PD.9–11 The present study aimed to evaluate the possible correlations of serum renalase levels with EAT thickness and other CVD risk factors in PD patients.
Material and methodsStudy populationThis is a cross-sectional study involving patients with ESRD older than 18 years old who received PD for at least 6 months (n=50) in our outpatient peritoneal dialysis unit and 40 healthy controls. Patients with structural heart disease (n=1), cardiac myopathy or pericardial disease (n=2), active infection (n=5), or other chronic inflammatory conditions (n=2) were excluded. Ultimately, a total of 40 PD patients (22 males and 18 females; mean age, 45.3±13.8 years) were analyzed for the study. All patients were on continuous ambulatory PD with four manual exchanges daily using 1500–2500ml solutions. Glucose concentrations of the solutions were adjusted depending on the patients’ body fluid status. When indicated, the patients received icodextrin or nutritional treatment. The dose of dialysis was prescribed to reach a weekly Kt/V urea target of >1.7. The control group included 40 age- and gender-matched healthy individuals (22 males and 18 females; mean age: 44.7±12.9 years) without any relevant systemic diseases. All subjects gave written informed consent, and the study protocol was reviewed and approved by the local ethics committee. The study was carried out in adherence to the principles of the Declaration of Helsinki.
Data collection and laboratory measurementsDemographic findings of the patients were obtained from the patients’ charts. All subjects underwent blood pressure (BP) and anthropometric measurements (height in cm, body weight in kg) and venous blood drawing. Systolic and diastolic BPs of the participants were measured by using a sphygmomanometer with an appropriate cuff size with the subject in the sitting position after 5min or more of rest. The mean value of three readings was used for the analysis. Blood samples were obtained by trained personnel from all the participants via antecubital venipuncture after a 12-hour overnight fast. Complete blood count, serum albumin, glucose, creatinine, parathormone (PTH), ferritin, C-reactive protein (CRP), total cholesterol, low density lipoprotein (LDL) cholesterol, triglycerides and high density lipoprotein (HDL) cholesterol levels were assessed in all the participants by using standard laboratory techniques for hospital use. For measurement of renalase, 5ml of venous blood specimens were obtained, centrifuged at appropriate conditions and kept at −80 degrees for maximum 1 month. The enzyme-linked immunosorbent assay (ELISA) kit by Uscn Life Science Inc. (China), using a monoclonal antibody specific to renalase, was used. Renalase levels are expressed in ng/ml.
Measurement of LVHAll the participants underwent two dimensional M-mode transthoracic color Doppler echocardiography imaging with a Philips IE-33 system and S5-1 transducer (1e5mHz, Philips, Bothell, WA, USA). Echocardiography was performed in all the participants by the same cardiologist. In left lateral decubitis position from parasternal longaxis views, standard M-mode measurements of interventricular septum thickness (IVST), left ventricular end-diastolic diameter (LVEDD), and left ventricular posterior wall thickness (LVPWT) were measured. Left ventricular mass (LVM) was calculated by using the Penn Cube Conversion formula.12,13
LVM (g)=1.04×[(LVEDD+IVST+LVPWT)3−(LVEDD)3]−13.6. LVM was divided by body surface area to find left ventricular mass index (LVMI). LVMI of >131g/m2 for men and >100g/m2 for women was accepted as LVH.14
Measurement of EAT thicknessEpicardial adipose tissue was identified as the echo-free space between the outer wall of the myocardium and the visceral layer of the pericardium, and its thickness was measured perpendicularly on the free wall of the right ventricle at the end-systole in three cardiac cycles. Parasternal long- and short-axis views were used. The average value of three cardiac cycles from each echocardiographic view was considered.
Statistical analysisFor statistical analysis, Statistical Package for Social Sciences for Windows 16.0 was used. Continuous variables were expressed as mean±standard deviation (in the presence of a normal distribution) or median and interquartile differences in 25th and 75th percentiles (in the absence of a normal distribution). Intergroup comparisons were made with Student's t test (in data with a normal distribution) or with Mann–Whitney U test (in data without a normal distribution). Categorical variables were compared with Chi-square test or Fischer Exact test, where appropriate. Pearson correlation coefficient was used for continuous variables with normal distribution and Spearman correlation coefficient was used for continuous variables which are not normally distributed. p<0.05 was considered significant.
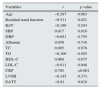
ResultsThe demographic and biochemical parameters of the PD patients and healthy subjects are presented in Table 1. The groups were well-matched for age and gender. BMI was significantly lower in the control group than in the PD patients. As expected, the average systolic and diastolic blood pressures were significantly higher in the PD patients than in the controls. Renal function tests were in normal ranges in the healthy subjects. Serum ferritin and PTH levels were significantly higher but hemoglobin, serum albumin and HDL cholesterol levels were significantly lower in the PD patients than in the control group. Echocardiographic evaluations revealed significantly increased LVMI and EAT thickness in the PD patients compared to the controls (Table 1). Mean serum renalase was significantly higher in the PD patients than in the control group (p=0.001) (Fig. 1). Table 2 shows correlations of renalase with cardiovascular risk factors in the PD patients. Twenty patients (50%) had residual renal function (RRF) and renalase levels were negatively correlated with RRF (r=−0.511, p=0.021) in these patients. Renalase was positively correlated with CRP (r=0.705, p<0.001). No correlation was observed between renalase and EAT thickness (r=−0.81 and p=0.618) or LVMI (r=−0.145, p=0.373). Also, renalase did not correlate with other CVD risk factors. Interestingly, there was a strong correlation between EAT thickness and LVMI in both the PD patients (r=0.848, p<0.001) and the controls (r=0.640, p<0.001).
Demographic and clinical parameters in PD patients and control group.
| Parameter | PD patients (n=40) | Control group (n=40) | p |
|---|---|---|---|
| Age (years) | 45.3±13.8 | 44.7±12.9 | 0.841 |
| Gender (male, n, %) | 22 (55%) | 22 (55%) | 1.000 |
| BMI (kg/m2) | 26.0±5.2 | 24.0±1.8 | 0.026 |
| Presence of DM (n, %) | 3 (7.5%) | – | – |
| Use of anti-hypertensive agents (n, %) | 21 (52.5%) | – | |
| Atherosclerotic cardiac disease (n,%) | 10 (25%) | ||
| Stroke (n,%) | 3 (7.5%) | ||
| Smoking (n,%) | 2 (5%) | ||
| Time on PD (month) | 80.4±56.1 | – | – |
| Cause of CKD (%) | |||
| DM | 7.5 | – | – |
| Glomerulonephritis | 22.5 | – | – |
| Hypertension | 30 | – | – |
| Polycystic kidney disease | – | – | – |
| Chronic pyelonephritis | 5 | – | – |
| Unknown | 35 | – | – |
| SBP (mmHg) | 125 (100–135) | 110 (100–120) | 0.003 |
| DBP (mmHg) | 78 (70–85) | 70 (60–70) | <0.001 |
| Kt/V | 2.12 (1.98–2.40) | – | – |
| Residual renal function (ml/min/1.73m2) | 0.12 (0– 1.41) | – | – |
| Hemoglobin (g/dl) | 11 (10–12) | 14 (13–15.1) | <0.001 |
| Glucose (mg/dl) | 84 (78–90) | 88 (78–90) | 0.576 |
| Albumin (g/dl) | 3.9 (3.5–4.1) | 4.6 (4.2–4.7) | <0.001 |
| Cr (mg/dl) | 8.3 (6.8–10) | 0.8 (0.7–0.8) | <0.001 |
| Ferritin (ng/ml) | 220 (110–338) | 69 (45–120) | <0.001 |
| PTH (pg/ml) | 414 (205–660) | 43 (37–54) | <0.001 |
| TC (mg/dl) | 185 (143–218) | 187 (167–198) | 0.950 |
| TG (mg/dl) | 142 (96–201) | 147 (135–180) | 0.675 |
| HDL-C (mg/dl) | 43.8±16.2 | 50.2±11.0 | 0.040 |
| LDL-C (mg/dl) | 92.0±33.0 | 101.0±17.0 | 0.130 |
| CRP (mg/l) | 5.7 (3–7.85) | 3 (2.1–3.59) | <0.001 |
| EATT(mm) | 0.51 (0.42–0.60) | 0.24 (0.20–0.26) | <0.001 |
| LVMI (g/m2) | 155 (116–212) | 95 (89–111) | <0.001 |
Categorical data are presented as frequencies and percentages; continuous variables are presented as mean±standard deviations or median and interquartile ranges (IQR: the range of values lying between 25th and 75th centiles) depending on their distributions.
Abbreviations: BMI, body mass index; Cr, creatinine; DBP, diastolic blood pressure; DM, diabetes mellitus; EATT, epicardial adipose tissue thickness; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; LVMI, left ventricular mass index; PD, peritoneal dialysis; PTH, parathyroid hormone; SBP, systolic blood pressure; TC, total cholesterol; TG, triglyceride.
Correlation analysis of renalase with cardiovascular risk factors in PD patients.
| Variables | r | p value |
|---|---|---|
| Age | −0.297 | 0.063 |
| Residual renal function | −0.511 | 0.021 |
| Kt/V | −0.189 | 0.243 |
| SBP | 0.017 | 0.916 |
| DBP | −0.051 | 0.755 |
| Albumin | 0.059 | 0.716 |
| TC | 0.005 | 0.978 |
| TG | −0.109 | 0.503 |
| HDL-C | 0.068 | 0.675 |
| LDL-C | −0.011 | 0.948 |
| CRP | 0.705 | <0.001 |
| LVMI | −0.145 | 0.373 |
| EATT | −0.81 | 0.618 |
Abbreviations: CRP, C-reactive protein; DBP, diastolic blood pressure; EATT, epicardial adipose tissue thickness; LVMI, left ventricular mass index; PD, peritoneal dialysis; SBP, systolic blood pressure.
The present study revealed that increased serum renalase was closely correlated with residual renal function in the PD patients. In agreement with this finding, other studies also reported higher levels of serum renalase in PD and hemodialysis patients than in healthy volunteers, which were correlated with residual renal function.9,10,15,16 Furthermore, serum renalase levels were negatively correlated with glomerular filtration rates and increased in a graded fashion from CKD stage 2–5 in both CKD and kidney transplant patients.11,17,18 Since renalase is an amine oxidase that metabolizes circulating catecholamines and reduce their plasma levels, experimental and genetic studies proposed a protective effect of renalase in regulation of blood pressure and development of cardiovascular complications in kidney disease patients. A further link between polymorphisms in the renalase gene and the risk of development of hypertension and cardiovascular diseases was also reported in these patients.8,19–21 In those studies, measuring renalase levels by western blot using a polyclonal antibody resulted in marked renalase deficiency in patients with end-stage renal disease. On the contrary, studies reported markedly increased levels when renalase was measured by ELISA in dialysis patients and kidney allograft recipients.15,22,23 The present study, for the first time, evaluated the possible association of serum renalase levels with cardiovascular risk factors in PD patients, but could not demonstrate a significant correlation between renalase and LVH, EAT thickness or hypertension. Some points may explain why the relation between renalase and cardiovascular risk reported in experimental and genetic studies were not observed in the PD patients in the current study. First, it might have been due to the method used, i.e. ELISA. It has been speculated that ELISA may recognize epitopes undetected with original polyclonal antibody or accumulated renalase breakdown products or may cross- react with an unrelated epitope, meaning that the measured level could be very high but unrelated to activity.24 However, the manufacturers of the assay claim that only renalase 1 levels are measured, and also there are no data on possible cross-reactivity. Second, as reported by Xu et al., there can be renalase inhibitors in plasma and therefore, activation of renalase can be very low and unremarkable although the enzyme levels are high.8 Finally, renalase is secreted not only by the kidney, but also by cardiomyocytes, liver and adipose tissue, thus, in the case of ESRD, other organs and tissues may oversecrete renalase, thus leading to very high serum levels.10
In the present study, renalase was found to be closely correlated with CRP. There have been few studies showing a relation between renalase and inflammation. Qi et al. reported that serum renalase levels were correlated with disease activity in lupus nephritis.25 They found that renalase had a positive correlation with erythrocyte sedimentation rate but a negative correlation with albumin. Among heart transplant recipients, renalase was correlated weakly with time after transplantation and TRAIL (TNF-Related Apoptosis Inducing Ligand); and strongly with kidney function, IL-6 and Von Willebrand factor.26 To the best of our knowledge, this is the first report describing a relation between renalase and CRP in PD patients.
The present study, for the first time, demonstrated a close association between EAT thickness and LVMI in the PD patients. Interestingly, similar relation was also true in the control group. Consistent with the present study, Iacobellis et al. reported a strong relation between echocardiographic EAT and LVM in healthy subjects.27 To explain this association, they proposed that increased visceral fat could have directly affected left ventricular output and stroke volume to perfuse the increased body mass. An interesting point about the findings of the present study was that although a significant correlation was found between EAT thickness and LVMI in the controls, this correlation was even stronger in the PD patients. Despite the presence of other factors including anemia, inflammation, hypervolemia, hypertension and activation of the renin-angiotension system as causes of LVH in the PD patients, which are not seen in the healthy individuals, this stronger correlation may suggest EAT thickness as an important factor in development of LVH in PD.
There are some limitations of the present study. First, this is a single-center study with a relatively small patient population. Second, the causal and effect relationship cannot be suggested due to its cross-sectional design. Therefore, a multi-center, prospective trial is needed to confirm the conclusions. Third, serum renalase levels were measured, but serum renalase activity was not, which could have eliminated the concerns on clinical usage of renalase levels. However, interpretation of data on renalase activity is rather difficult due to the growing criticism on potential monoamine oxidase activity of renalase.28,29
In conclusion, this study indicates that renalase is not related with EAT thickness or LVH, but closely associated with inflammation in PD patients. Better standardization of methods for measurement of renalase or its activity in serum may clarify the role of renalase in the pathogenesis of cardiovascular disorders in patients with ESRD.
FundingNo funding.
AuthorshipEach author has contributed substantially to the research, preparation and production of the paper and approves of its submission to the journal.
Conflicts of interestThe authors declare that they have no conflicts of interest.
None.







![Comparison of serum renalase levels between patients and healthy subjects. Median serum renalase level was significantly higher in PD patients than in control group [176.5 (100–278.3) vs 122 (53.3–170.0)ng/ml] (p=0.001).](https://static.elsevier.es/multimedia/02116995/0000003700000002/v1_201704211146/S0211699516302089/v1_201704211146/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w94GCRvdQBB6xyQjMrWMzrts=)




