COVID-19 reinfections in immunocompromised patients are a challenge for scientific community. Here we present the first case of a kidney transplant receipt with a lethal COVID-19 reinfection.
He is a 60-year-old male, with chronic kidney disease (CKD) due to focal and segmental glomeruloesclerosis that received his first kidney transplant 2004. In treatment with prednisone and rapamycin since 2007 when we was diagnosed of a hepatocellular carcinoma.
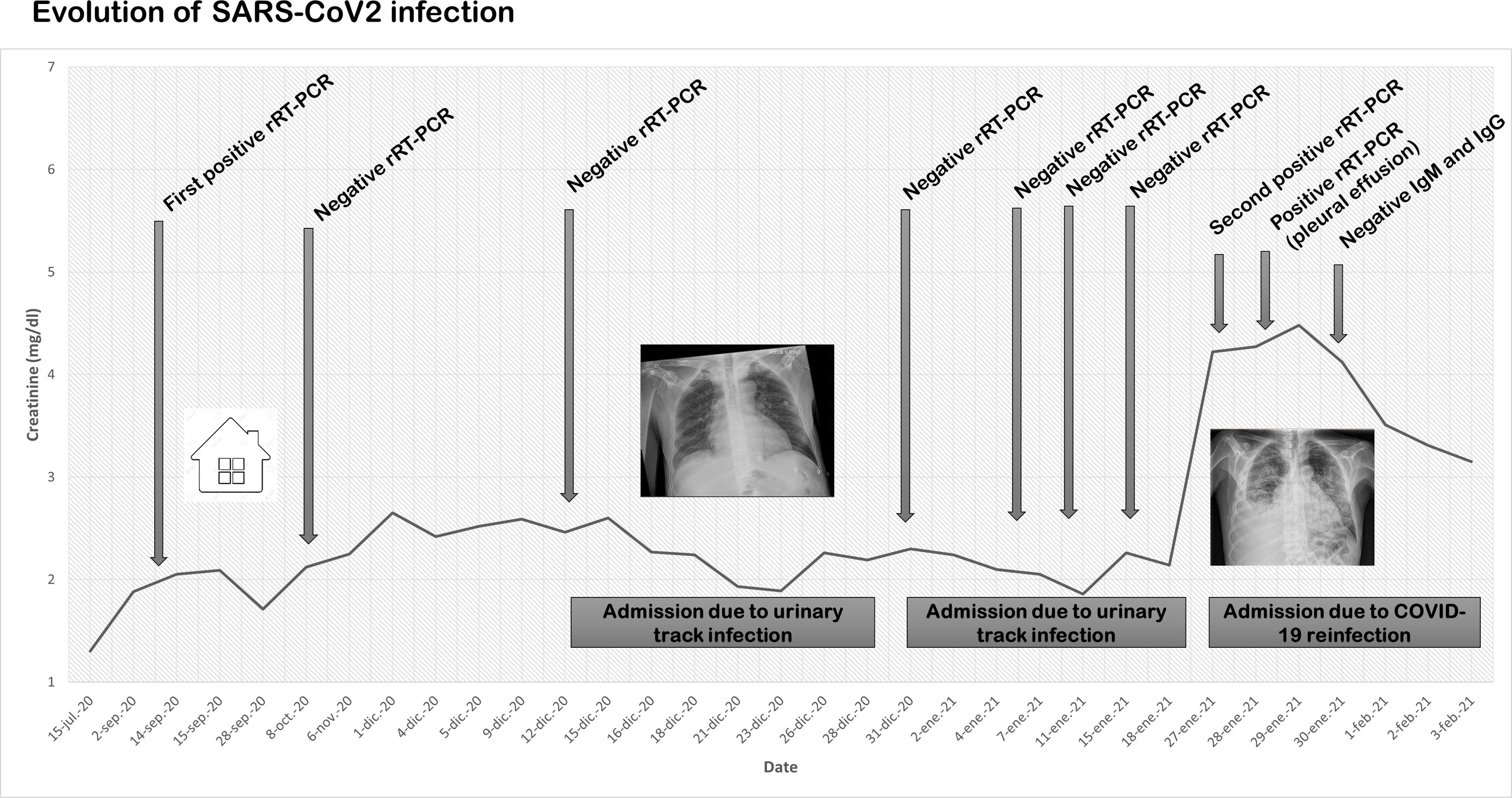
In August 2020, after a close contact to a COVID-19 family member, he developed mild symptoms (cough and low-grade fever) and SARS-CoV-2 infection was confirmed by a positive nasopharyngeal real-time reverse transcription-polymerase chain reaction (rRT-PCR) (Fig. 1). The clinical course was favorable, and he did not need further clinical assistance in that moment. A confirmatory rRT-PCR was performed showing a negative result.
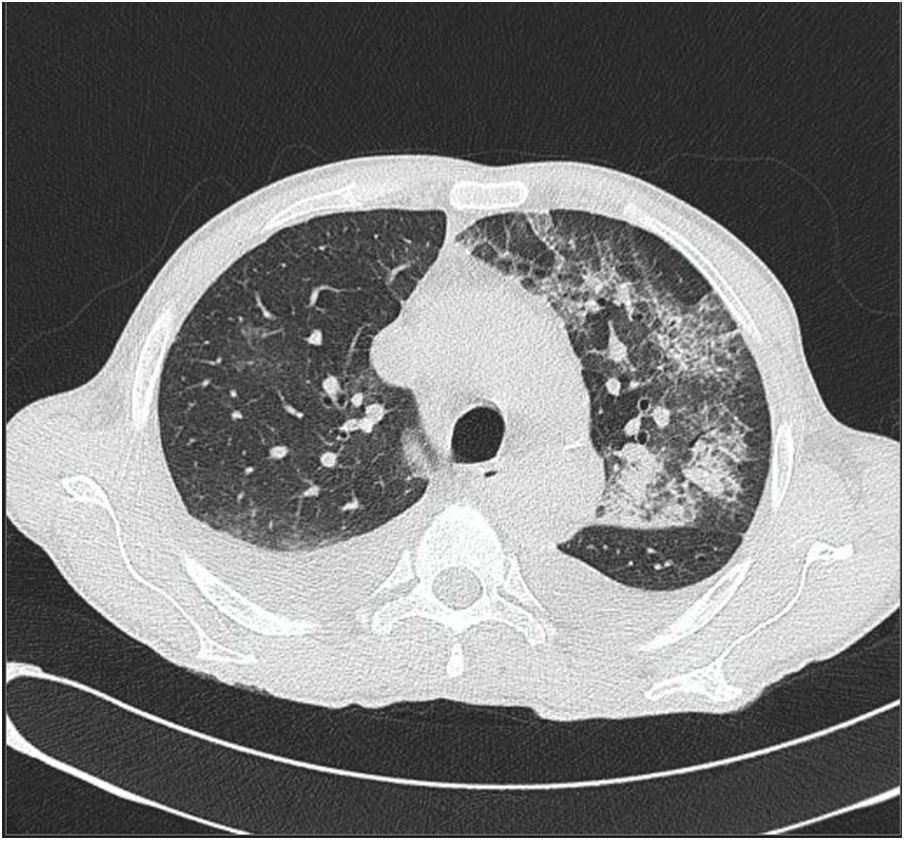
In December 2020 and January 2021, he was admitted in the hospital due to two episodes of urinary tract infection caused by Staphilococcus aureus and Serratia marcenses. In both hospitalizations, rRT-PCR were repeated five times (12th, 30th December and 4th, 9th, 17th January 2021) resulting negative in all of them. A chest X-ray performed on 12th December 2020 showed very low intensity bilateral infiltrates. In addition, on 8th January 2021, a chest-abdomen computed tomography scan demonstrated bilateral infiltrates in both hemithorax, probably as a residual lesion of the SARS-CoV-2 previous infection (Fig. 2). After diuretic and antibiotic treatment, chest X-ray improved significantly, and the patient was discharge asymptomatic 20th January 2021.
However, 28th January 2021, the patient was again admitted due to respiratory fever and acute injury of the allograft function. A chest X-ray showed bilateral infiltrates with unilateral pleural effusion. A new rRT-PCR confirmed SARS-CoV-2 infection by the same viral genotype, so immunosuppression was stopped, and dexamethasone was started. A thoracentesis of the pleural effusion demonstrated SARS-CoV-2 in the obtained sample. Antibodies (IgM and IgG) for SARS-CoV2 resulted negative. Although he was theoretically immunosuppressed, lymphocyte populations were normal. Despite established treatment including high flux oxygen, the patient deceased on 5th February 2021.
Several doubts have emerged around reinfections in general population. Technical errors in specimen collection or false negative results in rRT-PCR have been demonstrated in many patients driving to mistakes in COVID-19 reinfections. In addition, virus or non-active fragments of them can persist in sputum for weeks showing false positive results. However, the most part of the published reinfections have shown an asymptomatic course in the second positive rRT-PCR episode.1 This situation interestingly differs from our patient who presented a pauci-symptomatic course of COVID-19 infection with a lethal reinfection 5 months later.
Our patient presented some confirmatory features of a COVID-19 reinfection. First, he had positive rRT-PCR concurring with a family member contact and some mild symptoms. Despite this classical clinical picture, and even using a highly specific rRT-PCR, in some circumstances false positives can occur. Second, we confirmed negative rRT-PCR in several times, but radiological images showed residual bilateral lesions suggestive of COVID-19 past infection. Third, he developed new symptoms and chest X-ray worsen significantly simultaneously. In addition, in the reinfection episode, pleural effusion revealed the presence of SARS-COV-2 in the lungs.
Reasons for reinfection have not been widely studied, in part because immune response to SARS-CoV-2 has not been yet addressed.2 Probably, immunosuppressive factors can contribute to limit viral clearance and to impair cellular and humoral immunity in COVID-19 as in other infections.3 The clinical course of our patient agrees with this hypothesis. Although lymphocyte populations were normal at admission, in our patient concurred the personal history of the active neoplasia and the immunosuppression due to kidney transplant. Unfortunately, data regarding humoral or cellular immunity was not available after the first episode.
On this regard, reinfections can raise some concerns about the COVID-19 vaccines efficacy in those populations with risk factors for attenuating humoral immunity. In addition, pivotal COVID-19 vaccines randomized clinical trials have systematically excluded CKD patients so there is an important lack of information about their efficacy in that population. A very recent investigation letter has shown that a single dose of SARS-CoV2 mRNA vaccine generates a poor antispike antibody response, situation than can explain a COVID-19 reinfection, especially more than 4 months before the primoinfection.4 On the other hand, we must be cautious with those patients with prior episodes of COVID-19 who develop new symptoms and chest X-ray lesions and, of course, always recommend maintaining infection preventive measures.
In conclusion, reinfections in kidney transplants are plausible and require paying attention to those patients who developed COVID-19 symptoms even if they have had a previous episode.