Tissue oxygenation is maintained through various mechanisms, including blood pressure, circulating blood volume, and hemoglobin (Hb) concentration. In particular, Hb itself is considered an important factor because of its oxygen transportation function to systemic organs. Therefore, it is evident that oxygen supply would decrease in a severe anemic state.1 Recent reports have demonstrated the measurement of regional oxygen saturation (rSO2), a real-time marker of tissue oxygenation using near-infrared spectroscopy (NIRS).2,3 Measurement of rSO2 by using NIRS is a straightforward non-invasive procedure, which can be performed continuously. Nevertheless, only a few studies have investigated the association between systemic tissue oxygenation and the increase in Hb levels after blood transfusion in hemodialysis (HD) patients. In the current case study, we were able to monitor changes in the rSO2 of brain, liver, and lower-limb muscles during HD with and without blood transfusion.
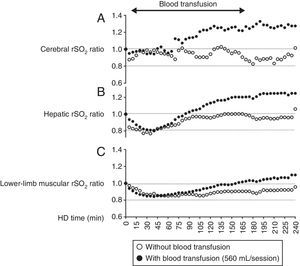
A 79-year-old woman undergoing HD was admitted to our hospital with acute obstructive suppurative cholangitis. Upon admission, we administered intravenous antibiotics and performed endoscopic biliary drainage, which resulted in a gradual improvement of her symptoms. Her anemia had been previously managed with an erythropoietin-beta (3000IU/session, 3 times/week); however, her Hb levels decreased to 6.8g/dL. Therefore, blood transfusion during HD was performed. She provided written informed consent to participate in monitoring of her systemic rSO2 during HD with or without blood transfusion. The rSO2 levels were monitored at the forehead, right hypochondriac region above the liver, and lower leg above the gastrocnemii muscles by using the INVOS 5100c (Covidien Japan). She received a transfusion of 560mL of concentrated red blood cells during HD and her Hb levels increased from 6.8 to 10.0g/dL after HD (Table 1). Furthermore, we compared the time course of rSO2 ratio in each organ, with and without blood transfusion. The rSO2 ratio was defined as the ratio of rSO2 values at t (min) during HD and initial rSO2 value before HD. As shown in Fig. 1, the changes in rSO2 ratio during HD without blood transfusion were modest in each organ, whereas the rSO2 ratio at each organ increased with blood transfusion, particularly in cerebral and hepatic regions.
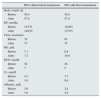
Vital signs and laboratory findings under HD with or without blood transfusion.
| HD without blood transfusion | HD with blood transfusion | |
|---|---|---|
| Body weight, kg | ||
| Before | 59.0 | 58.9 |
| After | 57.8 | 57.9 |
| BP, mmHg | ||
| Before | 147/71 | 118/93 |
| After | 149/74 | 173/75 |
| Pulse, beats/min | ||
| Before | 78 | 85 |
| After | 77 | 75 |
| Hb, g/dL | ||
| Before | 7.1 | 6.8 |
| After | 7.2 | 10.0 |
| BUN, mg/dL | ||
| Before | 38 | 26 |
| After | 7 | 5 |
| Cr, mg/dL | ||
| Before | 4.3 | 3.7 |
| After | 1.0 | 0.9 |
| Albumin, g/dL | ||
| Before | 2.9 | 2.8 |
| After | 3.0 | 3.0 |
BP, blood pressure; BUN, blood urea nitrogen; Cr, creatinine; Hb, hemoglobin; HD, hemodialysis.
Changes in regional oxygen saturation (rSO2) of the forehead (A), liver (B), and lower leg (C) as per the oxygenation values of cerebral, hepatic, and muscle tissue, respectively, under hemodialysis (HD) with or without blood transfusion. rSO2 ratio is defined as the ratio of rSO2 value at t (min) during HD and the initial rSO2 value before HD (rSO2 at t (min) during HD/initial rSO2 before HD).
In the world including United States, Europe, and Japan in around 1990, the use of erythropoiesis stimulating agents (ESA) in clinical settings was approved, which dramatically improved the Hb levels in patients with HD. However, even in the present day, blood transfusion during HD is still necessary for improving Hb levels in HD patients with severe anemia. Indeed, in comparison of blood transfusion frequency between ESA responsive and hyporesponsive HD patients, hyporesponsive patients had approximately 5 to 7-fold higher burden of blood transfusion than those with responsiveness.4 In addition, changes in systemic oxygenation induced by blood transfusion during HD have not been investigated extensively.
The brain has an auto-regulatory mechanism to maintain cerebral oxygenation. In HD patients, normalization of hematocrit by ESA did not increase cerebral oxygenation.5 Moreover, cerebral oxygenation in these patients was well-maintained when compared to pre-dialysis patients,6 and cerebral rSO2 values did not change by ultrafiltration under well-managed Hb levels.7 In the present case, rSO2 values did not change in any organ during HD without blood transfusion, which is similar to a previous report.7 On the other hand, each rSO2 values improved with an increase in Hb levels after blood transfusion. Particularly in the brain, oxygen supply decreases in patients with severe anemia1; furthermore, acute anemia by phlebotomy induces the deterioration of intracellular oxygen reactions in mice.8 Thus, presence of severe anemia may lead to a decrease in cerebral oxygenation despite the auto-regulatory mechanism of the brain. Therefore, the improvement of cerebral oxygenation after blood transfusion could be explained by the increase of oxygen-carrying capacity, which is associated with the increase in Hb levels.
Regarding the changes in rSO2 of each organ after blood transfusion, the improvement of lower-limb muscular rSO2 was relatively lower than that of cerebral and hepatic rSO2 even in this case without peripheral artery disease. In HD patients, the prevalence of subclinical peripheral artery disease reached around 20–25%,9 and its presence may directly influence the lower-limb muscular rSO2 via a decrease in oxygen supply induced by the dysfunction of macro- and micro-circulation. Furthermore, the skeletal muscle index has been reported to be lower in HD patients than in healthy subjects.10 Therefore, the changes in lower-limb muscular rSO2 value during HD might be influenced by the circulatory impairment and skeletal muscle weakness. However, the mechanism responsible for the differences in rSO2 improvement between different organs, induced by blood transfusion during HD, remains unclear and requires further investigation.
Our study suggests that blood transfusion during HD could be an effective method to improve tissue oxygenation, particularly cerebral and hepatic oxygenation in HD patients with severe anemia.
FinancingNone.
Conflict of interest statementThe authors have declared that no conflict of interest exists.