Idiopathic pulmonary fibrosis (IPF) is a chronic, progressive fibrotic disorder of the lung parenchyma. Rapidly progressive glomerulonephritis (RPGN) is a disease characterized by acute loss of renal function with glomerulonephritis, which is diagnosed by a pathologic pattern of crescent formation. A subgroup of RPGN is associated with anti-neutrophil cytoplasmic antibodies (ANCA). ANCA are abnormal auto-antibodies which are particularly related to small-vessel vasculitis in the kidneys. The perinuclear (p-ANCA) and cytoplasmic (c-ANCA) immunofluorescent patterns mainly correspond to antibodies directed against myeloperoxidase (MPO) and proteinase-3 (PR3), respectively. Herein, we report a case of a 37-year-old man with a history of ANCA (−) IPF who abruptly developed ANCA (+) RPGN with pulmonary renal syndrome after 12.5 years.
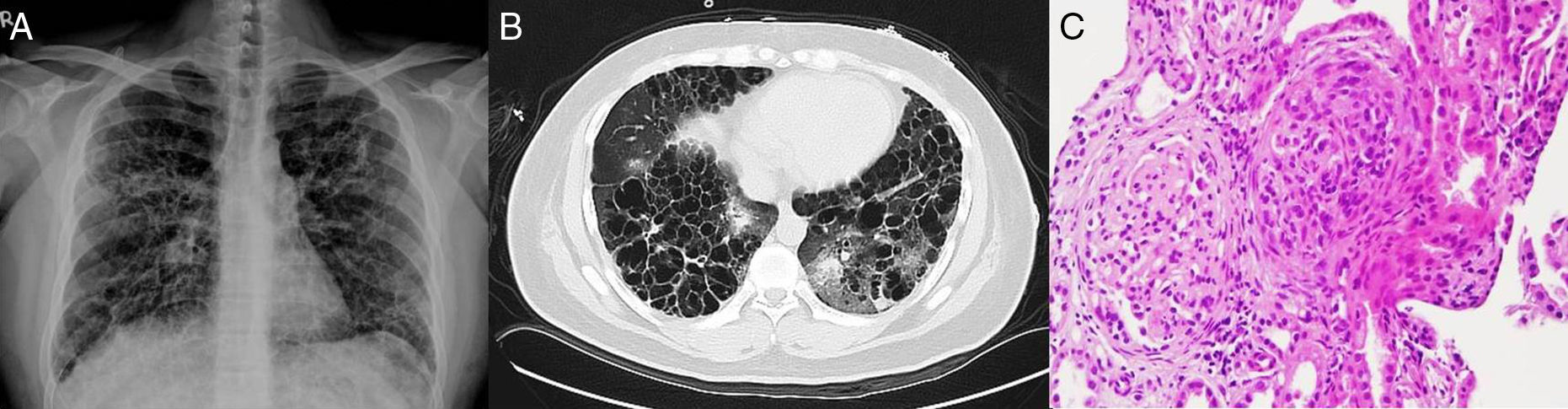
A 37-year-old man had a history of ANCA (−) IPF and gouty arthritis under control with prednisolone 5mg QOD and colchicines 0.5mg QD for over 12.5 years. A month prior to presentation, he began to experience intermittent muscle aches, arthralgias over bilateral hands and foamy urine. He finally presented to the emergency department with complaints of progressive shortness of breath, hemoptysis, poor urine output, and bilateral lower leg edema for one week. The physical examination was notable for respiratory discomfort, bilateral rales and grade 1 pitting edema of bilateral lower limbs. No petechiae, ecchymosis or costovertebral angle tenderness were noted. Blood tests showed leukocytosis, azotemia (BUN: 159mg/dL, creatinine: 21.1mg/dL), hyperkalemia, and anion gap metabolic acidosis. Urinalysis revealed proteinuria and hematuria. Immunologic studies showed mildly decreased C3 (76.5mg/dL, reference range: 90–180mg/dL) and positive MPO-ANCA (28IU/ml, reference range: negative <3.5, positive >5IU/mL). Chest X-ray showed infiltrates in both lungs. Non-contrast computed tomography of the chest showed interstitial reticular fibrotic infiltration with honeycomb appearance of bilateral lungs and consolidation in the left lung zone. Renal ultrasonography demonstrated normal-sized kidneys with increased cortical echogenicity. Ultrasound-guided renal biopsy was performed and revealed a proliferative glomerulonephritis with sclerosis and crescentic formation (Fig. 1). Immunofluorescent microscopy of the glomeruli was negative for staining of IgA, IgG, IgM, C1 and C3. Based on the above-mentioned examination results and clinical manifestations, severe MPO-ANCA (+) RPGN with pulmonary-renal syndrome was diagnosed. During the initial admission, emergent hemodialysis and plasmapheresis (5 sessions) were performed. Immunosuppressant therapy including pulse steroids (methylprednisolone 500mg daily for 6 days) followed by oral prednisolone (5mg BID) and azathioprine (50mg daily) and targeted therapy with rituximab (total 3g over 3 divided fractions) were also added. Nonetheless, high ANCA titers and poor renal function persisted so immunosuppression therapy and hemodialysis were maintained. Unfortunately, the patient died 1.5 years later from septic shock due to community-acquired pneumonia.
Imaging studies of the lungs and microscopic slides of renal tissue. (A) Chest X ray – Interstitial reticular fibrotic infiltration with honey comb appearance over both lungs. (B) Non-contrast computed tomography of the chest shows pulmonary fibrosis with cystic change in bilateral lung fields, with lower lung zones predominance. Infiltrates and ground-glass opacity in bilateral peri-hilar regions were also noted. (C) Renal biopsy (400×) – Glomeruli showed mesoangiocapillary proliferation and segmental sclerosis. Fibro-cellular crescents are also seen.
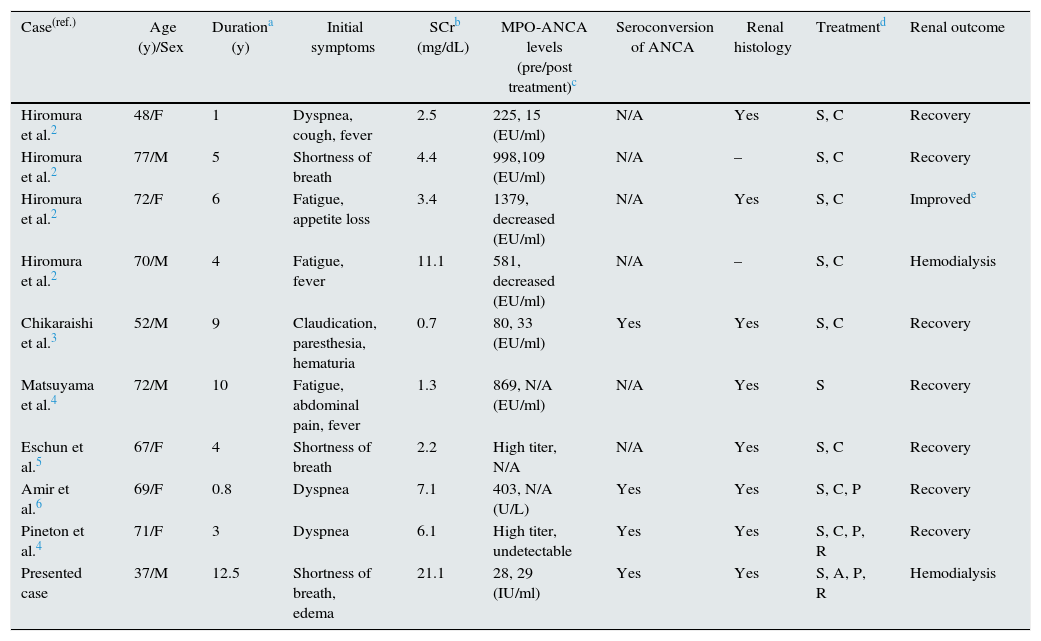
IPF may be an insidious lesion of vasculitis or a separate entity. It is now known that a subset of IPF patients are ANCA positive.1 A recent study examined the differences between ANCA positive and ANCA negative IPF. The levels of serum creatinine and C-reactive protein in patients with positive ANCA are significantly higher than those with negative ANCA. The survival rate of patients with higher titers of ANCA was less than patients with lower levels, implying the concentration of ANCA not only reflects the degree of systemic inflammation, but also indicates a more unfavorable prognosis. Most ANCA (+) IPF is MPO-ANCA, which is related to the development of crescentic glomerulonephritis in animal models7 and could develop into RPGN clinically. In our literature search, we found 10 patients with acute ANCA (+) RPGN in IPF patients, all of whom had MPO-ANCA2–4,8–10 (Table 1). Seven out of the 10 reported cases were Asians; however, the initial symptoms, time duration between IPF diagnosis and onset of RPGN, serum levels of MPO-ANCA varied widely, indicating the clinical manifestations of such cases are highly unpredictable. Recent studies have revealed two major pathways to tissue damage from ANCA associated vasculitis: the neutrophil pathway and the T-cell pathway. In the neutrophil pathway, an infection leads to the priming of neutrophils with an increase of adhesion molecules and ANCA-binding antigens on their surface. The binding of ANCA on neutrophils activates the degranulation process and cause damage to the endothelial layer. Under the T-cell pathway, regulatory T cells take over the function of tertiary lymphoid organs and promote further immune response. These two mechanisms interact with each other and magnify the cascade of inflammation and consequently causing vasculitis.5
Clinical characteristics of patients with idiopathic pulmonary fibrosis who developed into rapidly progressive glomerulonephritis.
| Case(ref.) | Age (y)/Sex | Durationa (y) | Initial symptoms | SCrb (mg/dL) | MPO-ANCA levels (pre/post treatment)c | Seroconversion of ANCA | Renal histology | Treatmentd | Renal outcome |
|---|---|---|---|---|---|---|---|---|---|
| Hiromura et al.2 | 48/F | 1 | Dyspnea, cough, fever | 2.5 | 225, 15 (EU/ml) | N/A | Yes | S, C | Recovery |
| Hiromura et al.2 | 77/M | 5 | Shortness of breath | 4.4 | 998,109 (EU/ml) | N/A | – | S, C | Recovery |
| Hiromura et al.2 | 72/F | 6 | Fatigue, appetite loss | 3.4 | 1379, decreased (EU/ml) | N/A | Yes | S, C | Improvede |
| Hiromura et al.2 | 70/M | 4 | Fatigue, fever | 11.1 | 581, decreased (EU/ml) | N/A | – | S, C | Hemodialysis |
| Chikaraishi et al.3 | 52/M | 9 | Claudication, paresthesia, hematuria | 0.7 | 80, 33 (EU/ml) | Yes | Yes | S, C | Recovery |
| Matsuyama et al.4 | 72/M | 10 | Fatigue, abdominal pain, fever | 1.3 | 869, N/A (EU/ml) | N/A | Yes | S | Recovery |
| Eschun et al.5 | 67/F | 4 | Shortness of breath | 2.2 | High titer, N/A | N/A | Yes | S, C | Recovery |
| Amir et al.6 | 69/F | 0.8 | Dyspnea | 7.1 | 403, N/A (U/L) | Yes | Yes | S, C, P | Recovery |
| Pineton et al.4 | 71/F | 3 | Dyspnea | 6.1 | High titer, undetectable | Yes | Yes | S, C, P, R | Recovery |
| Presented case | 37/M | 12.5 | Shortness of breath, edema | 21.1 | 28, 29 (IU/ml) | Yes | Yes | S, A, P, R | Hemodialysis |
ref.: reference, y: year, M: male, F: female, N/A: not applicable.
To the best of our knowledge, the present case was the youngest and the longest interval between IPF and RPGN diagnoses in the reported literature. Despite ANCA-negativity at IPF diagnosis 12.5 years ago, he subsequently developed ANCA-positive RPGN; the trigger of this seroconversion is unknown. The long duration might have been affected by the patient's regular use of prednisolone and colchicine, as colchicine may down-regulate multiple inflammatory responses and slow down the cascade of vasculitis.6 In conclusion, this case highlights the importance of regular monitoring levels of ANCA and alertness for renal involvement in patients with IPF.
Conflict of interestsThe authors declare that they have no conflict of interests.