Olmesartan is an angiotensin II receptor antagonist used for managing hypertension. Despite being an effective and secure drug, several reports have shown that olmesartan treatment can induce “sprue-like” enteropathy.1 Histological studies of kidney tissue from patients have often shown duodenal villous atrophy, increased intraepithelial lymphocytes and collagen depositions.2 The pathophysiological mechanisms causing the olmesartan-induced sprue-like enteropathy (OSLE) are not fully elucidated, but recent observations suggest a cell-mediated hypersensitivity reaction3 possibly related to the haplotype DQ2/DQ8.4 Persistent diarrhea often accompanies enteropathy due to olmesartan use, which could have an impact on renal function. Indeed, three previous reports have shown renal involvement secondary to diarrhea due to olmesartan-related enteropathy.5–7 Here we present a series of 19 cases of enteropathy related to olmesartan. Fourteen of these patients showed acute renal failure at admission, which was reverted after rehydration and discontinuing olmesartan.
Nineteen cases (9 females; median age 70, ranging from 56 to 88 years old) of OSLE were admitted to our hospital between September 2012 and June 2016. Patients went to the hospital due to persistent diarrhea that was non-responsive to conventional treatment. Prior to admission, patients had been treated with olmesartan for an average of 30 months (9–84 months). Most patients were taking 40mg/day olmesartan (10–40mg/day). OSLE was diagnosed after ruling out other possible causes for enteropathy (seronegative for tissular transglutaminase antibodies) and determining that the patient fulfilled the criteria set by Rubio et al.1 Sixteen patients needed hospitalization for a time period ranging from 1 to 35 days and one was treated in the intensive care unit. Treatment consisted of rehydration therapy and olmesartan discontinuation, which reverted the enteropathy and associated diarrhea. At the time of this publication histological analyses in 12 patients showed full tissue recovery.
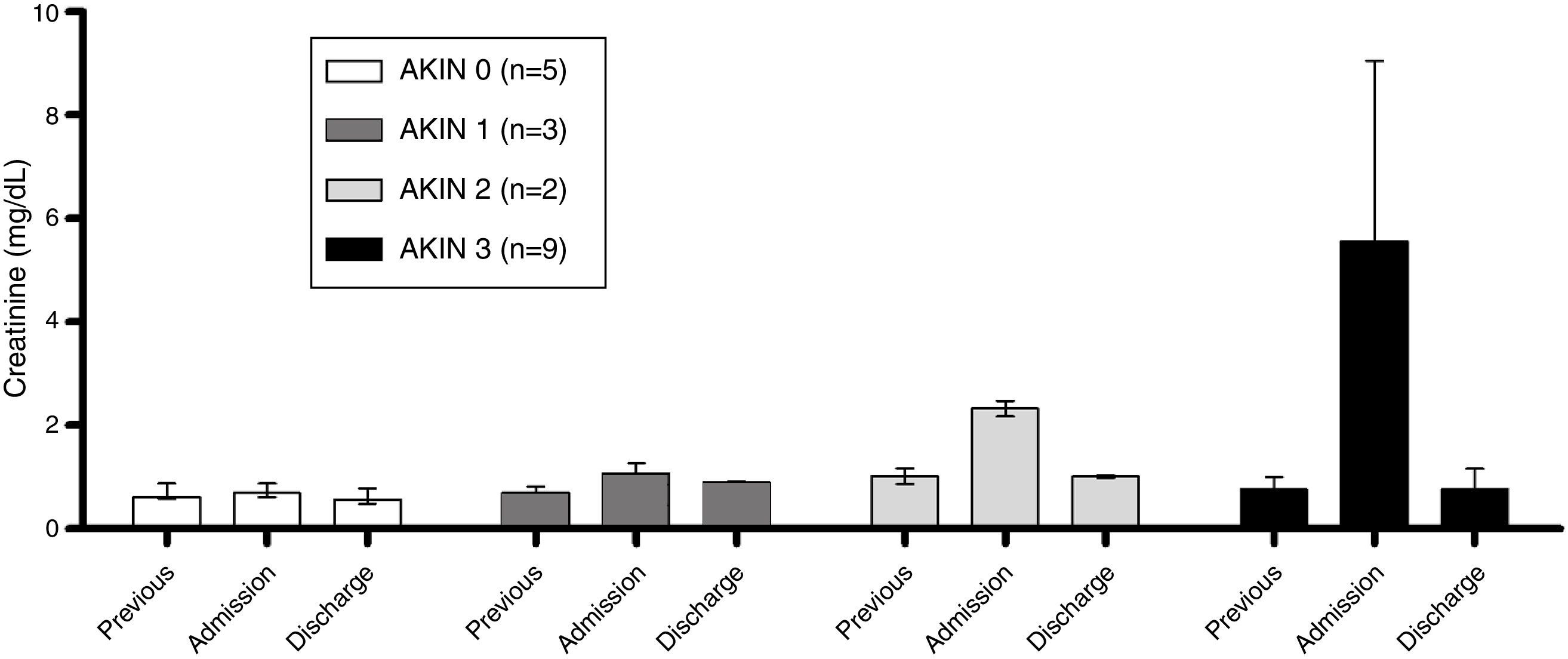
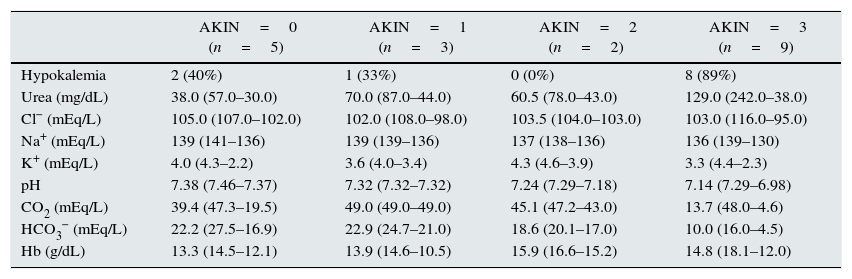
None of the patients had previous history of chronic renal disease, and estimated glomerular filtrate was normal prior to injury (86.0±17.4mL/min/1.73m2). At admission, electrolyte imbalance was observed (Table 1) while serum creatinine was considerably higher in comparison to previous values (Figure 1). Acute Kidney Injury Network (AKIN) classification8 showed 5 patients with no renal involvement, 3 patients at stage 1, 2 at stage 2 and 9 at stage 3. In addition, hypokalemia and metabolic acidosis was present in these patients (Table 1).
Incidence of hypokalemia and serum biochemical values at hospital admission in olmesartan-related enteropathy patients classified by the Acute Kidney Injury Network (AKIN) stages.
| AKIN=0 (n=5) | AKIN=1 (n=3) | AKIN=2 (n=2) | AKIN=3 (n=9) | |
|---|---|---|---|---|
| Hypokalemia | 2 (40%) | 1 (33%) | 0 (0%) | 8 (89%) |
| Urea (mg/dL) | 38.0 (57.0–30.0) | 70.0 (87.0–44.0) | 60.5 (78.0–43.0) | 129.0 (242.0–38.0) |
| Cl− (mEq/L) | 105.0 (107.0–102.0) | 102.0 (108.0–98.0) | 103.5 (104.0–103.0) | 103.0 (116.0–95.0) |
| Na+ (mEq/L) | 139 (141–136) | 139 (139–136) | 137 (138–136) | 136 (139–130) |
| K+ (mEq/L) | 4.0 (4.3–2.2) | 3.6 (4.0–3.4) | 4.3 (4.6–3.9) | 3.3 (4.4–2.3) |
| pH | 7.38 (7.46–7.37) | 7.32 (7.32–7.32) | 7.24 (7.29–7.18) | 7.14 (7.29–6.98) |
| CO2 (mEq/L) | 39.4 (47.3–19.5) | 49.0 (49.0–49.0) | 45.1 (47.2–43.0) | 13.7 (48.0–4.6) |
| HCO3− (mEq/L) | 22.2 (27.5–16.9) | 22.9 (24.7–21.0) | 18.6 (20.1–17.0) | 10.0 (16.0–4.5) |
| Hb (g/dL) | 13.3 (14.5–12.1) | 13.9 (14.6–10.5) | 15.9 (16.6–15.2) | 14.8 (18.1–12.0) |
Hypokalemia (K+ <3.5mEq/L) data has been reported as count (percentage). The rest of the data is reported as median (max–min). Hb, hemoglobin.
We have presented a series of cases (14 out of a total of 19) in which acute renal injury was secondary to dehydration due to OSLE. Renal involvement was severe in 11 patients (2 cases of AKIN stage 2 and 9 cases AKIN stage 3) accompanied by hypokalemia and metabolic acidosis.
The data obtained in this case series is similar to 2 cases in Spain with high creatinine and low potassium levels associated with enteropathy in patients treated with olmesartan, which reverted after drug discontinuation.5 Along the same lines, another case of enteropathy related to olmesartan with high serum creatinine and hypokalemia has been reported.9 Chronic enteropathy could be associated with severe dehydration and weight loss by diarrhea, which would explain the renal involvement observed in these patients.
Olmesartan is commonly used for hypertension treatment. Although it is a safe and reliable drug, the Food and Drug Administration has recommended suspending treatment if intestinal problems occur.10 Our data highlight the severe effects on renal tissue due to chronic diarrhea secondary to OSLE. More than half of the patients had stage 2 or 3 AKIN, in which kidney tissue was affected. It is likely that the duration and severity of the diarrhea episodes and the patient's hydration pattern contribute to the extent of kidney injury. Rehydration therapy and suspension of olmesartan treatment reverted symptoms and renal function was normal at discharge. However, in some cases, the extent of kidney tissue damage was high, which in turn could jeopardize patients’ renal function.
Besides weight loss, dehydration and other complications secondary to diarrhea, the renal involvement shown in this case series highlights the necessity of including olmesartan treatment in the differential diagnosis of chronic diarrhea in order to minimize the effects on kidney tissue and preserve patients’ renal function.