Calcineurin inhibitors (CNIs) are the gold standard immunosuppression in kidney transplant recipients. These drugs have shown better results in graft survival and patient outcome during the first year after transplantation. However, long-term use is associated with acute and chronic nephrotoxicity, which predisposes to graft loss.
Belatacept is a fusion protein binding to CD80 or CD86 ligands on antigen presenting cells that selectively blocks T-cell costimulatory signals. Data derived from two phase III trials (BENEFIT and BENEFIT-EXT) demonstrated the efficacy and safety of Belatacept in combination with Basiliximab, steroids and mycophenolic acid preventing graft acute rejection in Epstein–Barr virus positive recipients. Recently, the results of BENEFIT and BENEFIT-EXT study after 7 year follow up confirmed former data and showed a significant reduction in death and graft loss associated with the use of belatacept.1
Given the relevance of its beneficial effects in kidney function, some authors have proposed switching CNIs into belatacept treatment in intolerant patients to calcineurin or mTOR inhibitors showing an improvement in renal function.2–5
In our country, the administration of Belatacept is restricted by public health insurance. Public hospitals may use belatacept after individualized assessment requiring specific approval by internal committees in each case.
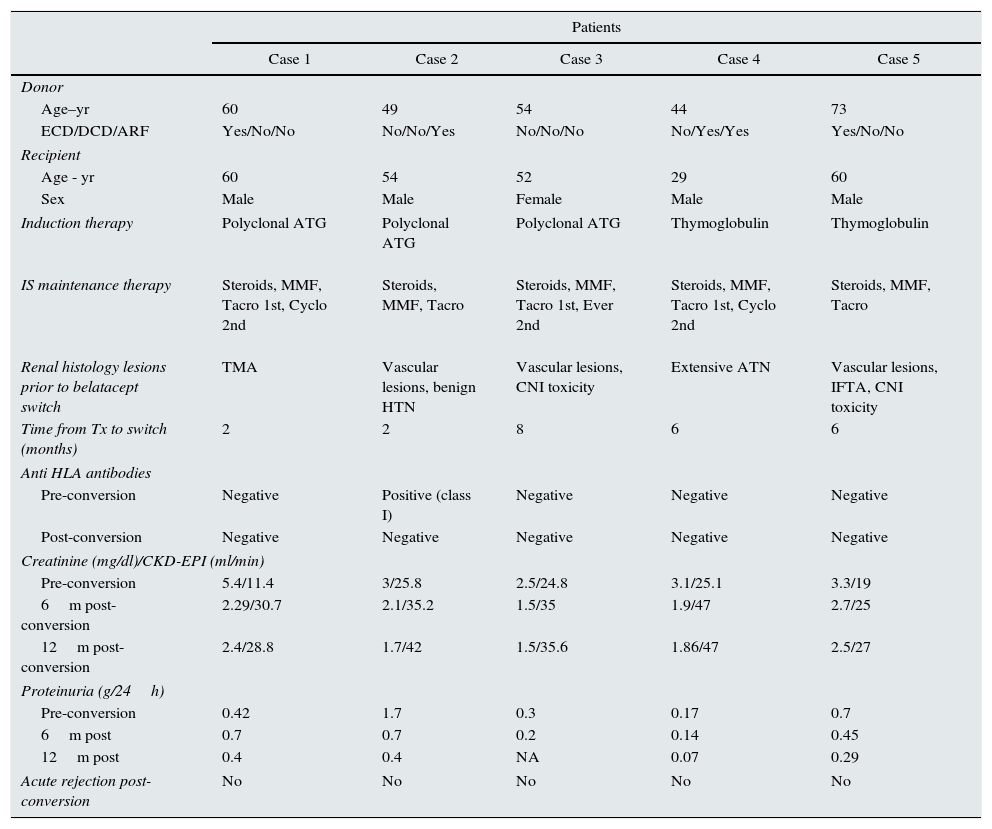
We summarize (Table 1) our clinical experience of switching to belatacept in 5 kidney transplant recipients through 2013–2015 after failure or intolerant therapy to tacrolimus and/or everolimus. All patients were Epstein–Barr virus positive.
Description clinical cases.
| Patients | |||||
|---|---|---|---|---|---|
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | |
| Donor | |||||
| Age–yr | 60 | 49 | 54 | 44 | 73 |
| ECD/DCD/ARF | Yes/No/No | No/No/Yes | No/No/No | No/Yes/Yes | Yes/No/No |
| Recipient | |||||
| Age - yr | 60 | 54 | 52 | 29 | 60 |
| Sex | Male | Male | Female | Male | Male |
| Induction therapy | Polyclonal ATG | Polyclonal ATG | Polyclonal ATG | Thymoglobulin | Thymoglobulin |
IS maintenance therapy | Steroids, MMF, Tacro 1st, Cyclo 2nd | Steroids, MMF, Tacro | Steroids, MMF, Tacro 1st, Ever 2nd | Steroids, MMF, Tacro 1st, Cyclo 2nd | Steroids, MMF, Tacro |
Renal histology lesions prior to belatacept switch | TMA | Vascular lesions, benign HTN | Vascular lesions, CNI toxicity | Extensive ATN | Vascular lesions, IFTA, CNI toxicity |
| Time from Tx to switch (months) | 2 | 2 | 8 | 6 | 6 |
| Anti HLA antibodies | |||||
| Pre-conversion | Negative | Positive (class I) | Negative | Negative | Negative |
| Post-conversion | Negative | Negative | Negative | Negative | Negative |
| Creatinine (mg/dl)/CKD-EPI (ml/min) | |||||
| Pre-conversion | 5.4/11.4 | 3/25.8 | 2.5/24.8 | 3.1/25.1 | 3.3/19 |
| 6m post-conversion | 2.29/30.7 | 2.1/35.2 | 1.5/35 | 1.9/47 | 2.7/25 |
| 12m post-conversion | 2.4/28.8 | 1.7/42 | 1.5/35.6 | 1.86/47 | 2.5/27 |
| Proteinuria (g/24h) | |||||
| Pre-conversion | 0.42 | 1.7 | 0.3 | 0.17 | 0.7 |
| 6m post | 0.7 | 0.7 | 0.2 | 0.14 | 0.45 |
| 12m post | 0.4 | 0.4 | NA | 0.07 | 0.29 |
| Acute rejection post-conversion | No | No | No | No | No |
ECD, expanded criteria donor; DCD, donor after circulatory death; ARF, Acute renal failure; IS, immunosuppression; Tx, transplantation; TMA, thrombotic microangiopathy; CNI, calcineurin inhibitors; HTN, arterial hypertension; ATN, acute tubular necrosis; IFTA, interstitial fibrosis and tubular atrophy; Tacro, Tacrolimus; Cyclo, Cyclosporine; Ever, Everolimus; MMF, mycophenolate mofetil; NA, not available.
Pre-transplant kidney biopsies were not performed. Clinical data were compatible with suboptimal donors, predisposing to a recipient poorer renal function. After transplantation patients received immunosuppression therapy consisting of anti-lymphocyte depleting antibodies, steroids and mycophenolic acid postponing tacrolimus starting to minimize delayed graft function. In four patients (cases 2, 3, 4 and 5) renal function was not adequate in the first month post-transplant. Analysis of graft biopsy showed CNI toxicity and chronic vascular lesions (likely related with donor background), but no evidence of acute rejection. Everolimus was considered an alternative to tacrolimus in all four cases. However it was not tolerated because of proteinuria or bone pain. In case 1 the reason for graft dysfunction was a thrombotic microangiopathy (TMA) due to the sequential use of tacrolimus first and cyclosporine later. They were converted to belatacept between 2 and 8 months post-transplantation showing immediate improvement of kidney function. Furthermore, anti HLA antibodies were negative after one year post-conversion.
Patients with low immunological risk (cases 1, 3, 4 and 5) received belatacept at a less intense dosage5 and in case 2 the dosage of belatacept was more intense5 due to positive class I anti-HLA antibodies (no donor specific antibodies).
All together, switching to belatacept is effective and safe in patients with failure therapy and/or intolerant to calcineurin or mTOR inhibitors at distinct time periods since transplantation. Moreover, belatacept was associated with better kidney function with no adverse events at short term and is an excellent alternative in grafts with renal dysfunction due to chronic vascular lesions or to CNI-TMA. This positive experience requires long-term assessments to confirm improvement in graft outcome.
Conflict of interestThe authors declare that they have no conflicts of interest.