Introducción: La enfermedad renal crónica representa un problema de salud pública por su elevada incidencia, su prevalencia, su alta morbimortalidad, sobre todo en aquellos que precisan de tratamiento renal sustitutivo. Uno de los factores que determinan la morbimortalidad de los pacientes en hemodiálisis (HD) es el acceso vascular del que disponen, y las complicaciones asociadas a los problemas de acceso vascular suponen una importante carga en nuestro trabajo diario, así como un elevado coste. Objetivos: Conocer la situación real de nuestra práctica clínica, compararla con otros estudios y medir el grado de cumplimiento de las recomendaciones de las Guías de Práctica Clínica en HD en lo relativo al acceso vascular de pacientes incidentes y prevalentes. Estudiar la supervivencia de los pacientes incidentes en función de su acceso vascular, ajustada a otros factores comórbidos. Pacientes y métodos: Se estudiaron los pacientes incidentes en HD desde enero de 2004 a octubre de 2009 (n = 422). Se analizaron: acceso vascular al inicio de HD, nefropatía de base, servicios de procedencia y enfermedades asociadas. Estudiamos el acceso vascular de nuestros pacientes prevalentes a fecha de octubre de 2009 (n = 299). Comparamos la supervivencia de los pacientes incidentes en función de su acceso vascular, ajustándolo a otros factores comórbidos. Resultados: El 67% de los pacientes prevalentes (62% hombres) portaban acceso vascular definitivo, y el 33%, un catéter venoso central (CVC). Del total de 422 pacientes incidentes, 42% provenían de la consulta por enfermedad renal crónica avanzada. El 54% eran diabéticos, el 92% hipertensos, el 28% presentaban cardiopatía isquémica filiada y un 13% arteriopatía periférica. Un 30% de los pacientes iniciaron HD a través de fístula arteriovenosa, un 1% portaban injerto sintético de PTFE (politetrafluoretileno) y un 69% CVC. El riesgo relativo de muerte asociado al uso de CVC al inicio de HD fue de 3,68 (intervalo de confianza: 95%, 2,93-6,35), ajustándolo a otros factores de comorbilidad (edad, diabetes mellitus, cardiopatía isquémica, arteriopatía periférica). Conclusiones: La alta mortalidad asociada al inicio de HD con CVC (riesgo relativo: 3,68), independientemente de otros factores, hacen de la reducción del uso de este acceso vascular un objetivo de primer orden. En nuestro medio no hemos podido conseguir los objetivos reseñados en las diferentes Guías en lo referente a la prevalencia e incidencia de los accesos vasculares para HD.
Background: Chronic kidney disease is a leading problem in public health due to its high incidence, prevalence and high morbidity and mortality, especially for those who require renal replacement therapy (RRT). As has already been described by other authors, the vascular access is one of the factors determining morbidity and mortality of patients in haemodialysis as well as their complications, which incur a high cost. Objectives: To know the real situation of our clinical practice, compare it with data from other studies, and to measure the degree of compliance by these patients with the recommendations of haemodialysis (HD) Clinical Practice Guidelines regarding vascular access . Also, to assess survival according to the type of vascular access used, adjusting for comorbidity factors. Patients and Methods: We studied the vascular access of our prevalent patients on haemodialysis by October 2009 (n=299, 62% men). Of these, 64% underwent HD through an autologous arteriovenous fistula (AVF), 3% were carrying synthetic grafts, and 33% had a central venous catheter (CVC). These percentages do not comply with the recommendations of the S.E.N. and KDOQI clinical guidelines. In order to know the real situation of our clinical practice, we compared our data with other studies, and measured the degree of compliance with the recommendations of the guidelines. The incident patients on HD were studied from January 2004 to October 2009 (n=422). We analysed basal nephropathy, associated diseases, and the type of vascular access at the start of HD. Results: A total of 30% had an AVF, 1% had synthetic grafts, and 69% had CVC. The calculated relative risk (RR) of death associated with the use of CVC at the start of HD was 3.68 (95% CI: 2.93-6.35) adjusted for other factors of comorbidity (age, diabetes mellitus, ischaemic heart disease, peripheral arterial disease). Conclusions: The high mortality associated at the beginning of HD with CVC (RR: 3.68), independently of other factors, make the decrease in the use of this vascular access an objective of first order. Presently, we have not been able to meet the objectives from the different Clinical Guidelines with respect to the prevalence and incidence of the vascular accesses for HD.
INTRODUCTION
Chronic kidney disease (CKD) is a public health problem due to its elevated incidence, prevalence, morbidity and mortality rates, and because it is considered as an independent cardiovascular risk factor, especially in patients that require renal replacement therapy (RRT).
According to the registry maintained by the Spanish Society of Nephrology (S.E.N.), 36 388 patients underwent RRT in Spain in 2007, over 46% of them on haemodialysis (HD). The incidence of patients on RRT is 125 patients per million population (pmp), a value that increases to 400pmp in the elderly age group (>70 years).1 One of the factors that determines the morbidity and mortality rates in HD patients is the type of vascular access used.
The recognised clinical practice guidelines, the European Best Practice Guidelines (EBPG),2 the Kidney Disease Outcomes Quality Initiative (KDOQI),3 and the guidelines from the S.E.N.,4 which are currently under review, establish as quality indicators in HD that the percentage of incident patients with a permanent vascular access point (arteriovenous fistula [AVF]) must be 50% (KDOQI) vs 80% (S.E.N.). Also, the percentage of prevalent patients with AVF in HD units must reach 80% (S.E.N), and the number of prevalent patients with a tunnelled central venous catheter (CVC) must be less than 10% (S.E.N. and KDOQI).
Several different studies have analysed the conditions in which HD patients are treated, including vascular accesses. The DOPPS study,5,6 in its various phases, describes a progressive increase in the use of CVC in incident patients on HD. By 2007, based on a representative sample of Spanish patients participating in this study, there was a greater relative risk (RR) of death (RR: 1.2) associated with CVC than with AVF.7 The ANSWER study8 in 2006 also reported high percentages of CVC use in incident HD patients (41%), similar to those described in 2006 by the Spanish Group for CKD9 in a sample of 1504 incident patients on RRT from 35 Spanish hospitals. More recently, in 2009, Gruss et al published a prospective study including 260 incident patients on HD and reported up to 47% of patients with CVC. They also observed high mortality rates (hazard ratio [HR]: 1.86) associated with this type of vascular access, which increased with the duration of use.10
The aim of our study was to evaluate the current situation in our clinical practice as regards the use of CVC in HD units, and the high mortality associated with this technique, comparing it to the published results from our field of medicine.
MATERIAL AND METHOD
We examined the vascular accesses in 299 prevalent patients on HD (62% males) at our unit of the Dr. Negrín University Hospital, Gran Canaria (HUGCDN) in October 2009, as well as the vascular accesses for the 422 incident patients on HD (66% males) between January 2004 and October 2009. We analysed the underlying nephropathy and associated diseases in each case. We also compared the results with the objectives set out by the clinical guidelines and with the results published in the mentioned studies. In the sample of incident patients, we did not include those with acute renal failure without previous CKD that started emergency HD and then recovered renal function. We analysed where the incident patients were referred from and how this affected the vascular access point at the start of HD, as well as the percentage of deaths in incident patients. We also calculated the RR of death associated with the use of CVC at the start of HD, and adjusted values for other factors of comorbidity.
We used SPSS software, version 17, for statistical analyses. We performed a descriptive analysis of the continuous and non-continuous variables. In order to compare for differences between the means of continuous variables, we used Student’s t-tests. We compared survival curves for incident patients on HD with CVC or AVF using Kaplan-Meier analyses and log-rank tests. We used a Cox regression analysis to evaluate whether other factors were influencing mortality in incident HD patients.
RESULTS
Prevalent patients
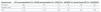
Of the total 299 prevalent patients in October 2009, 67% were undergoing dialysis through a permanent vascular access, and 33% through a CVC (Table 1).
Incident patients
Of the 422 patients that started RRT on HD, 93% were incident RRT patients, 6% came from peritoneal dialysis (PD), and 1% were patients with non-functioning kidney transplants. The mean age of this patient group was 62 years. When we analysed our sample by year, the annual incidence rate was fairly homogeneous, ranging between 62 patients in 2007 and 82 in 2008. In this group, 53.8% were diabetic, 91.7% had arterial hypertension, 28.2% had ischaemic heart disease of a known origin, and 12.6% had peripheral arterial disease, based on the data from the Canary Islands Renal Patient Registry.11
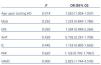
As regards where the patients came from, 42% were derived from advanced chronic kidney disease (ACKD) visits, 15% from other nephrological visits, 1% were transplant recipients with graft loss/dysfunction, 6% were from PD, 15% were from hospital emergency departments, and 21% were from other hospital departments. The patients started HD with a permanent vascular access in 31% of cases (AVF/PTFE [polytetrafluoroethylene] graft); and 77% of them (24% of the total) came from ACKD visits. Patients started HD with a CVC in 69% of cases, 74% of which were derived from other nephrological visits or other departments (Table 2). We compared the vascular accesses in incident patients from our unit with the recommendations from the guidelines and results from previously published studies (Table 3).
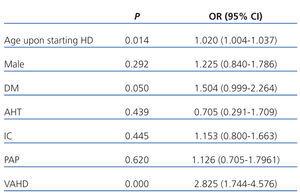
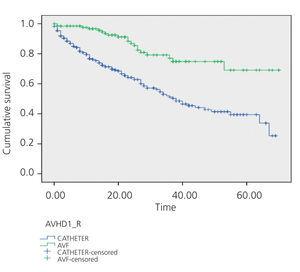
We compared survival curves between the group of incident HD patients with CVC and the group with AVF (Figure 1). The RR of death was 3.68 times greater in patients that started HD using a CVC (95% confidence interval [CI]: 2.93-6.35). Using the Cox regression analysis (Table 4), we examined which other factors may influence the mortality of our patients, and found a significant association with age (HR: 1.02) and the presence of diabetes mellitus (HR: 1.5), with an HR value associated with starting HD with a CVC of 2.85. We found no significant differences between the mean age of incident patients starting HD with a CVC and those starting with an AVF (62.7 years vs 61.2 years, respectively).
When comparing our results from October 2009 with those already analysed from our department in December 2005 and November 2007, we found no significant differences in the use of AVF and/or CVC in prevalent patients, although the use of CVC has progressively increased by 27%, 29%, and 33%, respectively, and the use of AVF has increased by 72%, 71%, and 67%.
DISCUSSION
There is a wealth of evidence in the literature regarding the mortality of patients on HD with a series of potentially modifiable factors, such as planning the entrance into HD, where patients are referred from, adequate control of phosphorous-calcium metabolism, anaemia and nutrition, and of course, the type of vascular access used.5-8,10,12
The studies published in our field have produced varying results in the level of compliance with the recommendations set forth by the clinical practice guidelines in terms of the type of vascular access to be used in HD, but they certainly are far from perfect.5-10 Are these recommendations realistic?
Many authors have analysed the possible causes of the disparities observed13:
- The current real profile of an incident HD patient: elderly, with multiple comorbidities.
- The characteristics of the various reference centres, the existence of ACKD visits, the formation of multi-disciplinary teams (nephrologists, vascular surgeons, and interventional radiologists).
- The equipment for monitoring vascular accesses in HD units.
- Protocols for early action, given the complications in permanent vascular accesses.
In our daily clinical practice, despite the fact that 42% of our patients are referred from ACKD visits, which would imply the ability to choose the correct technique, scheduled entrance, and a better control of other factors (anaemia, nutrition, etc.) and other preparations,12 up to 18% of these patients start HD with a CVC. In this group of patients, we registered at least one case of attempting a permanent vascular access (AVF) that failed. The incident population on HD in our sample had a mean age similar to that reported in other studies (62 years), although the incidence of diabetic nephropathy in our study was much higher (42% vs 21.5%),10,11 as is also shown in the most recent registries of patients on RRT published by the S.E.N. in 2009.14
One could interpret that these comorbidities are causing the elevated use of CVC on HD, but other authors have shown that, even in the non-diabetic population with no associated cardiovascular comorbidities and with nephrological monitoring previous to HD, the percentage of incident patients starting with a CVC is high (31.4%).15 Also, the difference in the mortality rates from patients with a CVC and those with an AVF is dependent on time, and is maintained even after adjusting for other comorbidity factors.10
In our study, we showed that elderly and diabetic patients die at a greater rate, but the factor most highly associated with mortality was starting HD with a CVC.
A decrease in the use of this type of vascular access should be a primary objective, necessitating the formation of multi-disciplinary teams (nephrologists, vascular surgeons, and interventional radiologists) and coordination for the monitoring of patients with advanced chronic kidney disease. Additionally, HD units should be equipped with the means to adequately monitor the permanent vascular accesses used and to guarantee emergency treatment of these, avoiding the need for CVC.
However, in our clinical experience, although we should optimise the monitoring of vascular accesses and use protocols for early action in the case of complications, we do have the impression that there is a sub-group of patients with CVC following several failed attempts at establishing a permanent access point, probably due to their precarious vascular system. This all leads us to reflect on the indication for this technique to be used in select populations: is the survival of these patients (diabetics, elderly, with compromised vascular system analysed using a venous map) greater when following a conservative treatment for CKD?
CONCLUSIONS
Throughout the years encompassed by our study, we have not been able to achieve the objectives set out by the different guidelines in terms of the prevalence and incidence of vascular accesses for HD. The high mortality associated with a start of HD using a CVC (RR: 3.68), independently of other factors, makes the decrease in the use of this type of vascular access a primary objective, taking into account the resources used and potential costs. Probably, the high prevalence of diabetic nephropathy in our field negatively influences the achievement of these objectives.
The implementation in our hospitals of monographic ACKD visits and the creation of multi-disciplinary teams (nephrologists, vascular surgeons, and vascular radiologists) could improve these results, as appears to be the case in isolated experiences.
Acknowledgements:
We would like to thank Dr José Carlos Rodríguez Pérez for his efforts in reviewing and correcting this manuscript.
Table 1. Vascular accesses used in prevalent patients. Comparison with guideline recommendations
Table 2. Vascular accesses in incident patients according to departments of origin
Table 3. Vascular accesses in incident patients. Comparison with guideline recommendations and previous studies
Table 4. Factors related to mortality. Cox regression
Figure 1. Survival curves