Diabetic kidney disease is the leading cause of end-stage chronic kidney disease (CKD). The renin–angiotensin–aldosterone system (RAAS) blockade has been shown to slow the progression of diabetic kidney disease. Our objectives were: to study the percentage of patients with diabetic kidney disease treated with RAAS blockade, to determine its renal function, safety profile and assess whether its administration is associated with increased progression of CKD after 3 years of follow-up.
Materials and methodsRetrospective study. 197 diabetic kidney disease patients were included and divided into three groups according to the treatment: patients who had never received RAAS blockade (non-RAAS blockade), patients who at some point had received RAAS blockade (inconstant-RAAS blockade) and patients who received RAAS blockade (constant-RAAS blockade). Clinical characteristics and analytical variables such as renal function, electrolytes, glycosylated hemoglobin and glomerular filtration rate according to CKD-EPI and MDRD formulas were assessed. We also studied their clinical course (baseline, 1 and 3 years follow-up) in terms of treatment group, survival, risk factors and renal prognosis.
ResultsNon-RAAS blockade patients had worse renal function and older age (p<0.05) at baseline compared to RAAS blockade patients. Patients who received RAAS blockade were not found to have greater toxicity or chronic kidney disease progression and no differences in renal prognosis were identified. Mortality was higher in non-RAAS blockade patients, older patients and patients with worse renal function (p<0.05). In the multivariate analysis, older age and worse renal function were risk factors for mortality.
ConclusionsTreatment with RAAS blockade is more common in diabetic kidney disease patients with eGFR≥30ml/min/1.73m2. In our study, there were no differences in the evolution of renal function between the three groups. Older age and worse renal function were associated with higher mortality in patients who did not receive RAAS blockade.
La enfermedad renal diabética es la primera causa de enfermedad renal crónica terminal en nuestro medio. El bloqueo del sistema renina-angiotensina aldosterona (BSRAA) enlentece la progresión de la enfermedad renal diabética. Nuestros objetivos son: estudiar pacientes tratados con BSRAA, comparando su evolución según el filtrado glomerular, su perfil de seguridad y si se asocia a una progresión mayor de la enfermedad renal crónica.
Materiales y métodosEstudio retrospectivo de 197 pacientes con enfermedad renal diabética. Se dividieron en tres grupos según tratamiento: pacientes que no recibieron BSRAA (no BSRAA), pacientes que en algún momento lo recibieron (BSRAA discontinuado) y pacientes que recibieron BSRAA (BSRAA mantenido). Se estudiaron características clínicas y analíticas: función renal, ionograma, hemoglobina glicosilada, filtrado glomerular según CKD-EPI y MDRD. Analizamos su evolución (basal, año y 3 años) en relación con el grupo de tratamiento, supervivencia, factores de riesgo y pronóstico renal.
ResultadosLos pacientes no BSRAA presentaron en el momento basal peor función renal y edad más avanzada (p<0,05) en comparación con los que recibieron BSRAA. Los pacientes que recibieron BSRAA no mostraron mayor toxicidad, ni más progresión de la enfermedad renal crónica, y no evidenciamos diferencias en el pronóstico renal. La mortalidad fue mayor en pacientes no BSRAA, de mayor edad y peor función renal (p<0,05). En el análisis multivariado los factores de riesgo de mortalidad fueron edad avanzada y peor función renal.
ConclusionesEl tratamiento con BSRAA es más frecuente en pacientes con FGe≥30mL/min/1,73m2. No observamos diferencias en la evolución de la función renal entre los tres grupos. La mayor mortalidad observada en pacientes que no recibieron BSRAA se relacionó con la edad avanzada y peor función renal.
Diabetes mellitus (DM) is a pandemic disease affecting 415 million people worldwide. According to the projections of the International Diabetes Federation, the number of affected individuals is expected to increase to 642 million by 2040, the vast majority of which are in developing countries.1
Life expectancy is reduced in patients with DM and cardiovascular disease is the main cause of mortality.1,2 Thirty percent of DM type 1 patients and 10–40% of patients with type 2 DM will develop diabetic kidney disease (DKD) that may lead to advanced chronic kidney disease (CKD) requiring renal replacement therapy (RRT).1 In fact, DKD is one of the main causes of advanced CKD and RRT. In Catalonia, it is the second leading cause of RRT, with an incidence of 22%.3 Ten years after being diagnosed of DM2, 25% will present microalbuminuria, 5% will present macroalbuminuria and 0.8% will have an increase in serum creatinine or advanced kidney failure.4
The renin–angiotensin–aldosterone system (RAAS) is involved in cardiorenal regulation of patients with DM. Angiotensin II, acting on type 1 receptors (AT1), have multiple effects: induces vasoconstriction, increases the tubular reabsorption of Na+, increases oxidative stress, and favors renal production of fibrogenic and inflammatory cytokines. Thus, the inhibition of Angiotensin II production or blocking the type 1 receptor of angiotensin II have been shown to be beneficial for cardiorenal protection in the patient affected with DKD.5–7
Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARB) reduce mortality, cardiovascular risk and slows down the progression of kidney disease; therefore, most guidelines recommend the use of these drugs as a first option in diabetic patients with CKD.1,8–10 In DKD patients, the renoprotective effects of RAAS blockade (RAASB) are superior to other antihypertensive drugs. The RAASB using ACE inhibitors or ARB delays both the onset and the increase of albuminuria, and also slows down the deterioration of glomerular filtration rate (GFR).11–13 However, presently the level of evidence about the potential beneficial effect of RAASB in DKD patients with advanced CKD is low.14,12
Despite the antiproteinuric effects of RAASB, many diabetic patients on this treatment do not show a reduction in the progression of renal disease. Thus, strategies are needed to make the modulation of RAAS more effective or discover other strategies independent of RAAS. The clinical tendency is to withdraw these drugs in patients with GFR<30ml/min, (CKD stages 4–5). A study using small number of patients showed that the discontinuation of RAASB, ACEI/ARB, in patients with advanced CKD (46% diabetics) delayed the need for RRT.15 It should be noted that the majority of these patients had advanced age (mean 73 years) and some of them have renovascular disease. In addition, a non-significant increase in proteinuria was observed.16 Therefore, the beneficial effect of RAASB in patients with advanced CKD is controversial. We propose to study patients with DKD and establish the percentage on patients being treated with RAASB, and also compare the percent of patients on RAASB with GFR greater or lower than 30ml/min and at each CKD stage. Furthermore, we want to study the safety profile of these drugs and whether the administration of RAASB have an effect on CKD progression and the prognosis of the patients.
MethodsSample selectionThis is an observational and retrospective study including 197 patients with DKD followed from 2009 to 2014. The inclusion criteria were: more than 18 years old with DM type 2 and DKD (GFR≤60ml/min and/or albuminuria≥30mg/g in two determinations). They were followed for at least one year in the outpatient clinics of the Nephrology Department-Hospital del Mar. The exclusion criteria were patients under 18 years of age, absence of DKD and a follow-up of less than one year.
Clinical variablesThe data was collected from the clinical history. The variables studied were age, gender, race, and time of evolution of diabetes. Parameters of renal function such as creatinine or urea, eGFR by MDRD and CKD-EPI formulas; glycosylated hemoglobin (HbA1c) as a marker of glycemic control were also recorded. Systolic and diastolic blood pressure (SBP, DBP), and the antihypertensive treatment, mainly SRAAB (ACE inhibitors, ARBs, antialdosterone) were also collected. The causes of SRAAB withdraw impairment of renal function (decrease of 30% of eGFR or increase in serum creatinine of 30%), hyperkalemia (serum potassium level above 5.5mEq/L) or other causes were recorded. In addition, we evaluated the complications presented during the study period (ischemic heart disease, stroke, diabetic retinopathy and peripheral vasculopathy) and the need for RRT, either in the form of kidney transplant, hemodialysis or peritoneal dialysis. Finally, mortality was also recorded.
All biochemical parameters and treatments were collected at baseline, at one year and at three years of follow-up. Baseline was the first visit to the nephrology outpatient clinic. For analysis, the participants were divided into three groups according to the SRAAB treatment regimen: patients who never received the treatment (non-RAASB) (n=42), patients who received SRAAB at some point during the follow-up (inconstant-SRAAB) (n=73) and patients who continued the treatment with BRAAS throughout the follow-up period (constant-SRAAB) (n=82). The participants were also divided according to the eGFR, into two groups: <30ml/min/1.73m2 (CKD stage 4/5) (n=60) and ≥30ml/min/1.73m2 (n=137).
Statistical analysisProcessing and analysis of data was performed using the statistical program IBM SPSS® version 19.0. The quantitative variables with normal distribution are presented as mean and standard deviation. The variables that did not follow a normal distribution are presented as median and interquartile range. The qualitative variables are expressed as a percentage. The chi-squared test was used for the comparison of qualitative variables and for the comparison of the means between two samples we used the t-Student for independent data and U Mann–Whitney in case of non-normality of the variable. For comparison between means with more than two categories, the ANOVA test was used, together with the Tukey test for multiple comparisons between different groups. Regarding the survival analysis and the initiation of renal replacement therapy, Kaplan–Meier curves and Log-Rank tests were used. A Cox multivariate regression analysis of proportional risks was performed to evaluate mortality risk factors adjusted for the following variables: age, renal function, history of ischemic heart disease, history of cerebrovascular accident, history of peripheral vascular disease, history of diabetic retinopathy, sex and treatment with SRAAB. Statistical significance was considered when p<0.05.
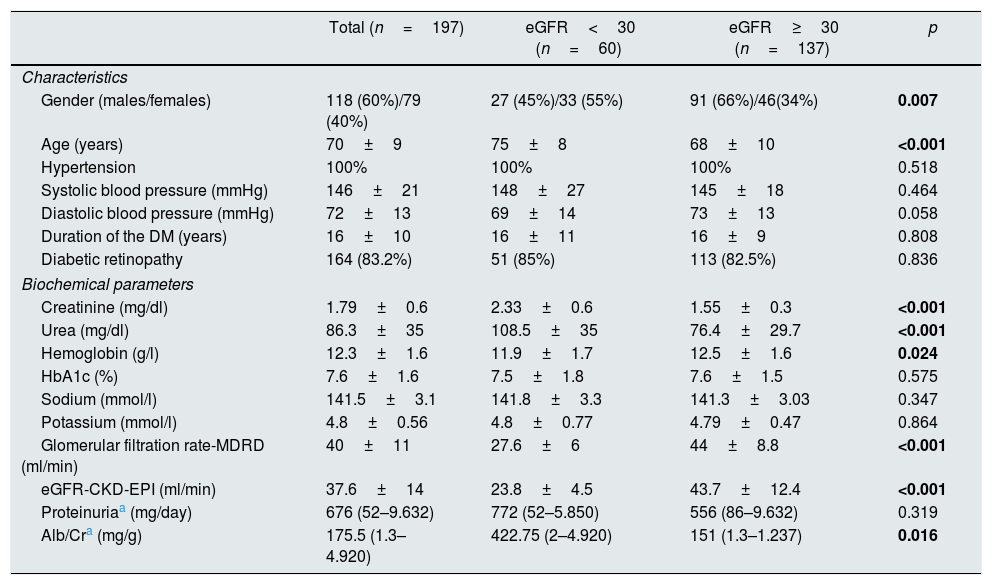
ResultsCharacteristics of the patientsWe analyzed 197 patients with an average age of 70±9 years, 60% males (n=118). Table 1 shows baseline characteristics, analytical parameters related to renal function and parameters related to diabetic disease in the entire sample of patients and divided according to the eGFR. As shown, all patients were on antihypertensive treatment. At the start of the follow-up period, 60 (30.5%) patients had a GFR<30ml/min/1.73m2. Average SBP and DBP were 146±21 and 72±13mmHg, respectively; HbA1c was 7.6±1.6% and the average hemoglobin 12.3±16g/dl. The average of eGFR by MDRD was 40±11ml/min/1.73m2, and by CKD-EPI 37.6±14ml/min/173m2. The mean duration of DM was 16±10 years and diabetic retinopathy was present in 164 patients (83.2%). Proteinuria was 676 (52–9632) mg/24h, the albuminuria/Cr ratio (Alb/Cr) 175.5 (1.3–4920) mg/g and the serum creatinine was 1.79±0.66mg/dl. The mean serum concentration of sodium and potassium were 141.5±33.1 and 4.8±0.6mEq/l respectively.
Baseline demographic, clinical and biochemical characteristics of the population.
| Total (n=197) | eGFR<30 (n=60) | eGFR≥30 (n=137) | p | |
|---|---|---|---|---|
| Characteristics | ||||
| Gender (males/females) | 118 (60%)/79 (40%) | 27 (45%)/33 (55%) | 91 (66%)/46(34%) | 0.007 |
| Age (years) | 70±9 | 75±8 | 68±10 | <0.001 |
| Hypertension | 100% | 100% | 100% | 0.518 |
| Systolic blood pressure (mmHg) | 146±21 | 148±27 | 145±18 | 0.464 |
| Diastolic blood pressure (mmHg) | 72±13 | 69±14 | 73±13 | 0.058 |
| Duration of the DM (years) | 16±10 | 16±11 | 16±9 | 0.808 |
| Diabetic retinopathy | 164 (83.2%) | 51 (85%) | 113 (82.5%) | 0.836 |
| Biochemical parameters | ||||
| Creatinine (mg/dl) | 1.79±0.6 | 2.33±0.6 | 1.55±0.3 | <0.001 |
| Urea (mg/dl) | 86.3±35 | 108.5±35 | 76.4±29.7 | <0.001 |
| Hemoglobin (g/l) | 12.3±1.6 | 11.9±1.7 | 12.5±1.6 | 0.024 |
| HbA1c (%) | 7.6±1.6 | 7.5±1.8 | 7.6±1.5 | 0.575 |
| Sodium (mmol/l) | 141.5±3.1 | 141.8±3.3 | 141.3±3.03 | 0.347 |
| Potassium (mmol/l) | 4.8±0.56 | 4.8±0.77 | 4.79±0.47 | 0.864 |
| Glomerular filtration rate-MDRD (ml/min) | 40±11 | 27.6±6 | 44±8.8 | <0.001 |
| eGFR-CKD-EPI (ml/min) | 37.6±14 | 23.8±4.5 | 43.7±12.4 | <0.001 |
| Proteinuriaa (mg/day) | 676 (52–9.632) | 772 (52–5.850) | 556 (86–9.632) | 0.319 |
| Alb/Cra (mg/g) | 175.5 (1.3–4.920) | 422.75 (2–4.920) | 151 (1.3–1.237) | 0.016 |
Alb/Cr: albumin/creatinine ratio; DM: diabetes mellitus; eGFR: estimated glomerular filtration rate; HbA1c: glycosylated hemoglobin.
Bold values are p values with statistical significance.
It should be noted that patients with CKD stages 4/5 were older than patients with eGFR≥30ml/min/1.73m2 (p<0.001). The distribution of gender was different according to renal function; in patients with eGFR≥30ml/min/1.73m2, the majority were men, whereas with eGFR<30ml/min/1.73m2, the majority were women. Patients with eGFR<30ml/min/1.73m2 (n=60), had lower hemoglobin levels than those with an eGFR≥30ml/min/1.73m2 (n=137) (p=0.024). A trend toward lower HbA1c was observed in patients with GFR<30ml/min/1.73m2.
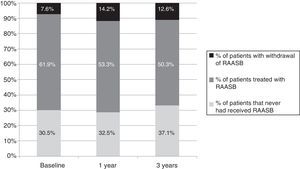
Treatment of patients with diabetic kidney disease with renin–angiotensin–aldosterone system blockadeAt baseline, 62% of patients (n=122) were on treatment with RAASB, this number decreases at year one of follow-up (53%, n=105). After 3 years, 50.3% of patients were on RAASB (n=80).
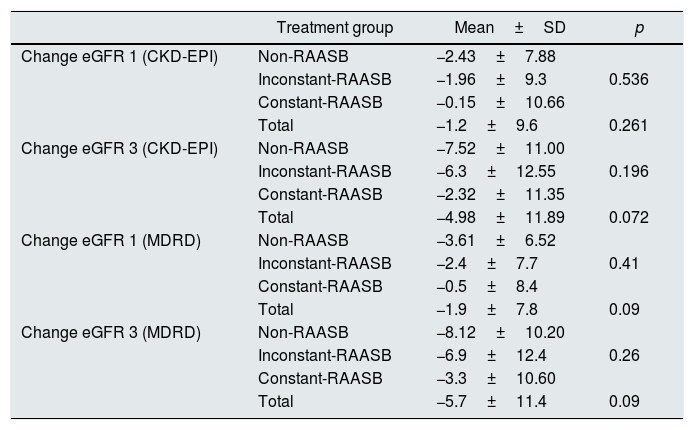
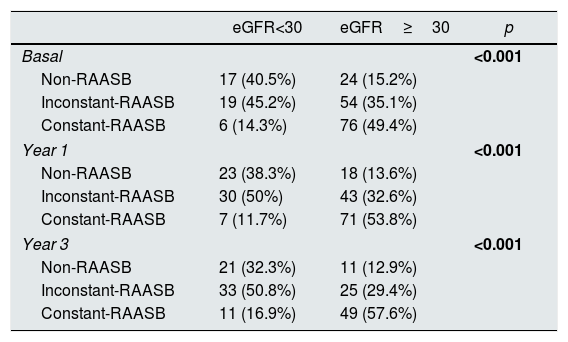
Table 2 shows the treatment used in patients separated according to the change in eGFR from baseline to 1 and 3 years of follow-up. The change in eGFR was calculated with MDRD and CKD-EPI formulas. The treatment did not produce a significant effect in the decrease of eGFR. However, the eGFR was significantly different between treatment groups at the three time points of the study (p<0.001 in the three cases). Treatment was less frequently prescribed in patients with GFR<30ml/min/1.73m2 than patients with eGFR≥30ml/min/1.73m2. Likewise, the rate of treatment discontinuation was high in patients with eGFR<30ml/min/1.73m2 (p<0.001).
Change in estimated glomerular filtration rate according to treatment group.
| Treatment group | Mean±SD | p | |
|---|---|---|---|
| Change eGFR 1 (CKD-EPI) | Non-RAASB | −2.43±7.88 | |
| Inconstant-RAASB | −1.96±9.3 | 0.536 | |
| Constant-RAASB | −0.15±10.66 | ||
| Total | −1.2±9.6 | 0.261 | |
| Change eGFR 3 (CKD-EPI) | Non-RAASB | −7.52±11.00 | |
| Inconstant-RAASB | −6.3±12.55 | 0.196 | |
| Constant-RAASB | −2.32±11.35 | ||
| Total | −4.98±11.89 | 0.072 | |
| Change eGFR 1 (MDRD) | Non-RAASB | −3.61±6.52 | |
| Inconstant-RAASB | −2.4±7.7 | 0.41 | |
| Constant-RAASB | −0.5±8.4 | ||
| Total | −1.9±7.8 | 0.09 | |
| Change eGFR 3 (MDRD) | Non-RAASB | −8.12±10.20 | |
| Inconstant-RAASB | −6.9±12.4 | 0.26 | |
| Constant-RAASB | −3.3±10.60 | ||
| Total | −5.7±11.4 | 0.09 |
Comparison of means by one-way ANOVA test. The values p<0.05 are considered significant.
Change eGFR 1 (CKD-EPI): differences in glomerular filtration rates from baseline to one year of follow-up estimated with the CKD-EPI formula; change eGFR 3 (CKD-EPI): differences in the glomerular filtration rate between baseline and the third year of follow-up estimated with the CKD-EPI formula; change eGFR 1 MDRD: differences in glomerular filtration rates between the baseline and one year of follow-up estimated with the MDRD formula; change eGFR 3 MDRD: differences in the glomerular filtration rate between the initial moment and the third year of follow-up estimated with the MDRD formula.
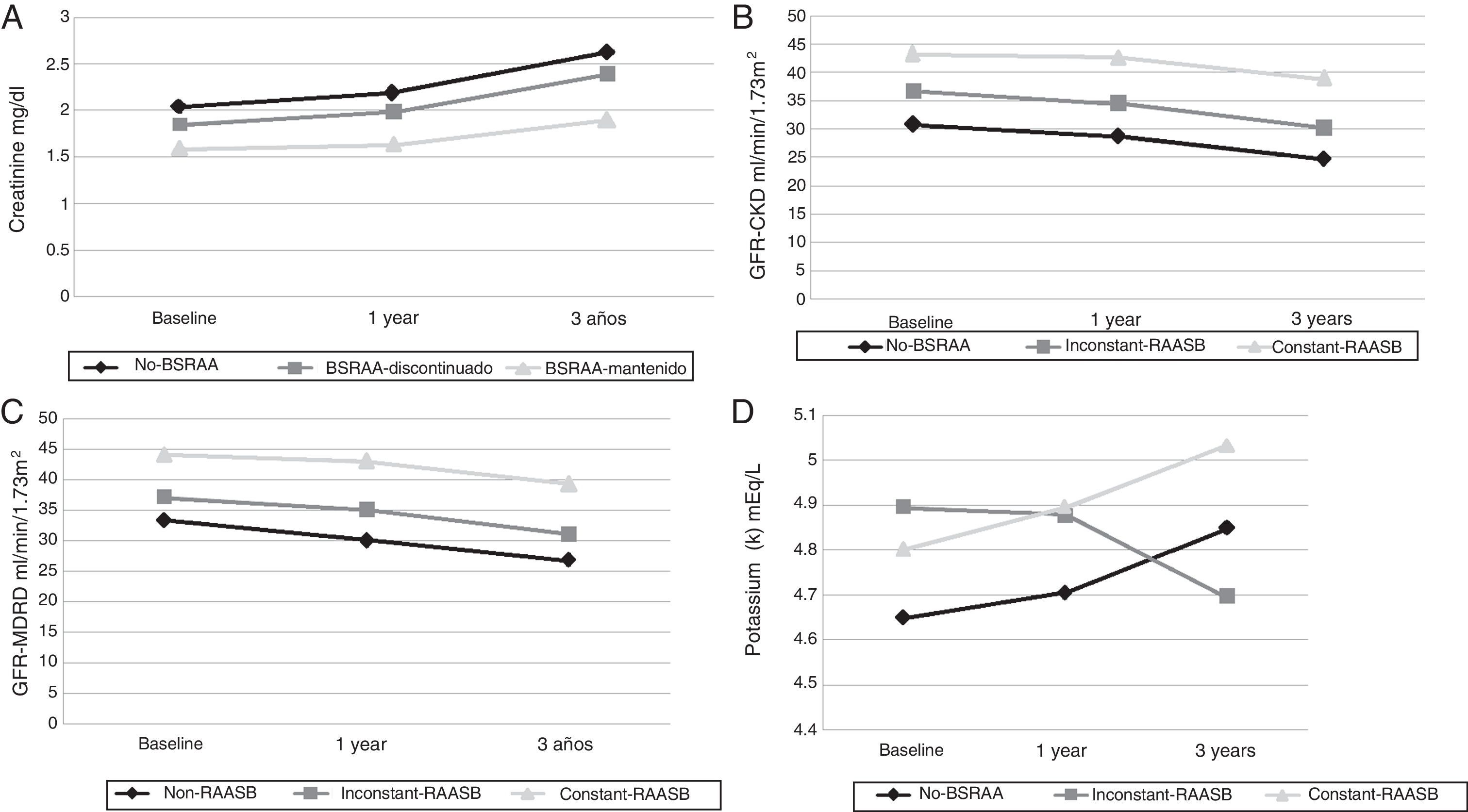
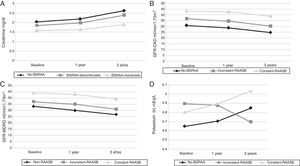
The biochemical parameters of the three treatment groups were compared using one-way ANOVA and the Tukey test when statistical differences were found. The SBP and DBP were not significantly different between the treatment groups, except for the DBP of the first year of follow-up (p=0.007). We observed that patients who did not receive RAASB at any time had worse renal function and this was evident since baseline (Table 3). Thus, creatinine was always lower in patients who received RAASB as compared to patients who did not receive RAASB during the follow-up period, or who received it at some point during the study. These differences were observed at baseline, at one year and at 3 years of follow-up (Fig. 1). Surprisingly, the degree of proteinuria was not different between the treatment groups. Serum potassium was increased in patients with constant-RAASB, and it was decreased in patients who had inconstant-RAASB (Fig. 1D).
Distribution of treatments according to the glomerular filtration rate.
| eGFR<30 | eGFR≥30 | p | |
|---|---|---|---|
| Basal | <0.001 | ||
| Non-RAASB | 17 (40.5%) | 24 (15.2%) | |
| Inconstant-RAASB | 19 (45.2%) | 54 (35.1%) | |
| Constant-RAASB | 6 (14.3%) | 76 (49.4%) | |
| Year 1 | <0.001 | ||
| Non-RAASB | 23 (38.3%) | 18 (13.6%) | |
| Inconstant-RAASB | 30 (50%) | 43 (32.6%) | |
| Constant-RAASB | 7 (11.7%) | 71 (53.8%) | |
| Year 3 | <0.001 | ||
| Non-RAASB | 21 (32.3%) | 11 (12.9%) | |
| Inconstant-RAASB | 33 (50.8%) | 25 (29.4%) | |
| Constant-RAASB | 11 (16.9%) | 49 (57.6%) | |
Statistically significant differences were observed between the eGFR calculated with the MDRD formula and the distribution of patients in the three treatment groups.
Inconstant-RAASB: during follow-up patients were prescribed RAASB, but for a shorter period of time than the full follow-up (3 years); Constant-RAASB: patients were prescribed RAASB and their administration was maintained during the three years of follow-up; non-RAASB: patients were not prescribed RAASB during follow-up.
Bold values are p values with statistical significance.
Changes of various biochemical parameters throughout the follow-up.
A) Evolution of serum creatinine levels during the follow-up. The graph shows the serum creatinine throughout the study according to the different treatment groups. Differences are observed in the treatment and the values of serum creatinine (p<0.001, p<0.001, p<0.001). However, no differences were observed during the follow-up period in each group individually. Results are expressed as mean serum creatinine mg/dl.
B) Evolution of the eGFR by CKD-EPI throughout the follow-up period. No significant differences were observed between the baseline and the first year, nor between the baseline and the third year. However, they were significant diferences observed between treatment groups and eGFR.
C) Evolution of the eGFR-MDR rate throughout the follow-up. No ssignificant differences were observed between baseline and first year, nor between baseline and third year. However, there were significant differences between treatment groups and eGFR.
D) Evolution of serum potassium concentrations throughout the follow-up. No significant differences were found between the different treatment.
RAASB: renin angiotensin aldosterone system blockade.
Changes in eGFR, calculated with both formulas, throughout the follow-up in relation to the treatment group are shown in Table 2. There were no statistically significant differences in any of the two study periods (1 and 3 years). The mean change in eGFR calculated with the two formulas can be seen in Fig. 1B and C.
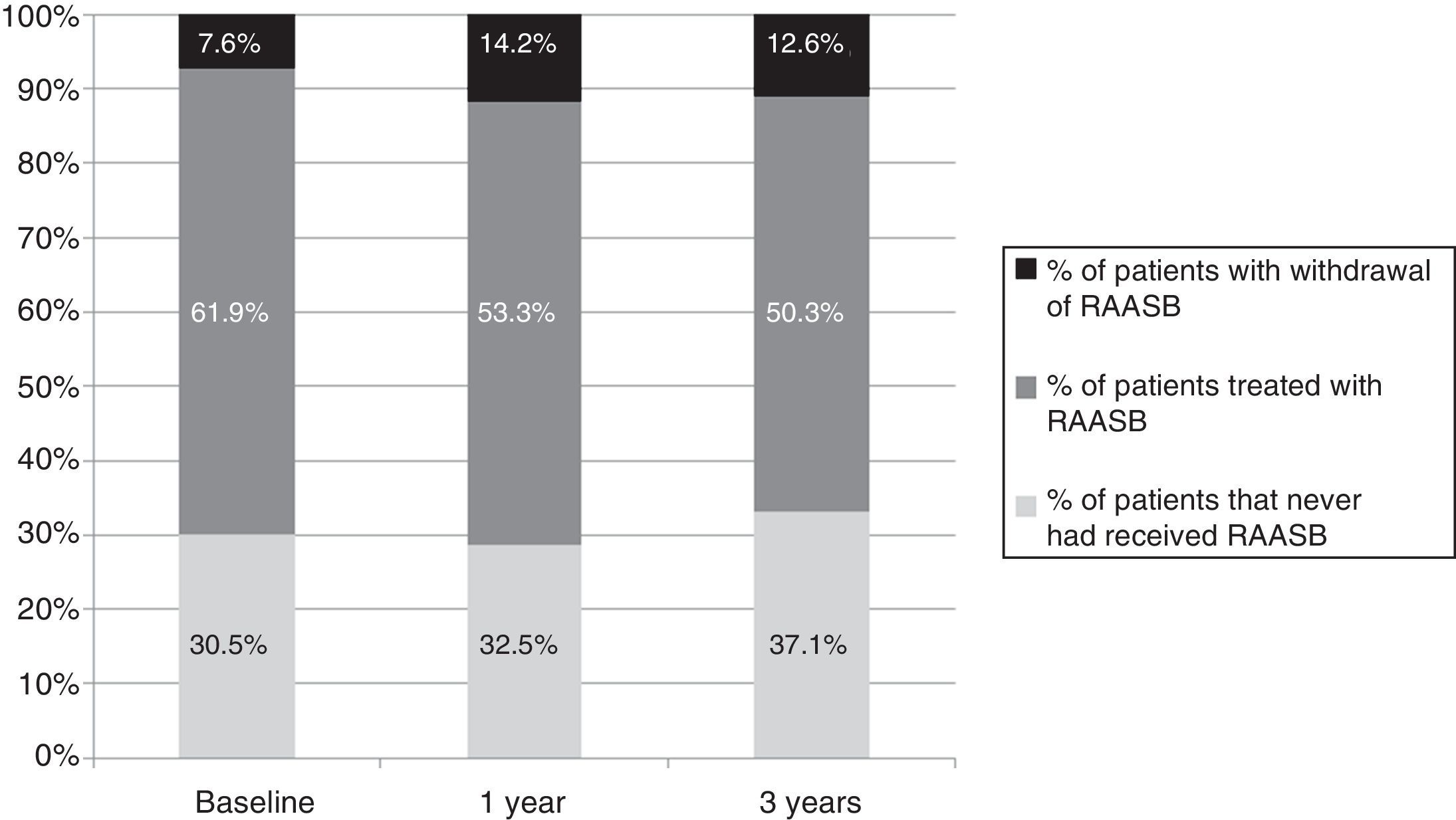
Discontinuation of the renin–angiotensin–aldosterone system blockadeThe proportion of patients in each treatment group during the follow-up period is shown in Fig. 2. At baseline (first visit to the nephrology outpatient clinic), 137 patients were on RAASB and the treatment was discontinued in 15 cases (12%), 14 of them were on monotherapy and one in combination therapy ACEI–ARB. In addition, one patient had the antialdosterone treatment discontinued, but ARB was maintained.
Evolution of the RAASB prescription. Patients who never received treatment with RAASB during the follow-up period and those who received are represented as a percentage (%). Among the patient prescribed, the % of patients in which it was withdrawn is indicated.
RAASB: renin angiotensin aldosterone system blockade.
At one year of follow-up, of the 133 patients treated with RAASB, 28 patients (21%) withdrew the treatment. Between baseline and the first year there were patients that, due to clinical indications, were started on medication. At the end of the study follow-up (third year), of the total of 100 patients on treatment with RAASB (total of 159 patients being followed), 20 patients (20%) had the treatment discontinued.
Discontinuation of renin–angiotensin–aldosterone system blockade and evolution of renal functionIn patients with low eGFR, treatment with RAASB was less frequent at baseline and during the follow-up (Table 3). In addition, the renal function was more deteriorated in patients in whom the treatment was withdrawn. In fact, the main reason why the treatment was withdrawn was the deterioration of renal function. Deterioration of renal function was the cause of withdrawal of RAASB in 13 of 15 cases at baseline, 22 of 28 cases at the first year and 19 of 20 cases at the third year of follow-up. Discontinuation of treatment due to hyperkalemia occurred in 5 patients, 3 at baseline and 2 at the first year of follow-up. Symptomatic arterial hypotension along with other clinical reasons was also cause for withdrawal but with a lower frequency.
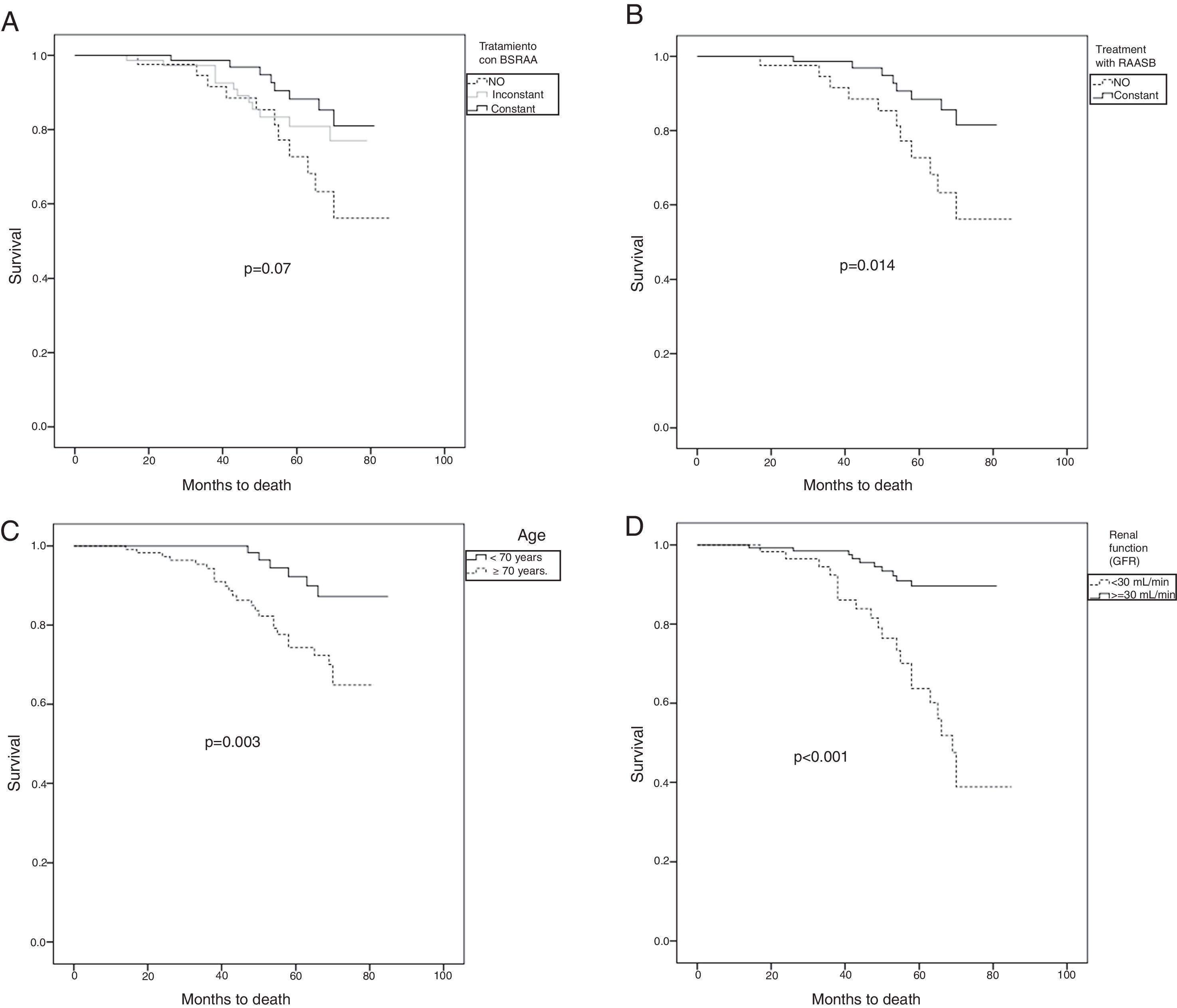
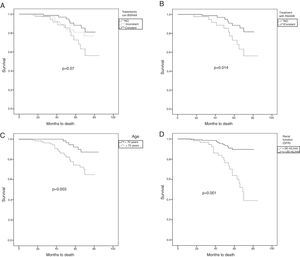
Development of complications associated with diabetic kidney disease and mortalityMortality was assessed using the Kaplan–Meier curves and the Log-Rank test (Fig. 3). The sample of patients was divided according to the treatment received: non-SRAAB, constant-SRAAB or inconstant-SRAAB during the follow-up period (Fig. 3A). No significant differences were found between the treatment groups. Subsequently, we analyzed the sample excluding the patients in whom the treatment was discontinued (Fig. 3B). Patients who did not receive treatment with SRAAB had higher mortality (p=0.014). In addition, patients were divided into those under and over 70 years of age (Fig. 3C). Those who were 70 years or older had higher mortality (p<0.003). Finally, we divided the cohort according to renal function measured by the CKD-EPI formula (<30 vs ≥30ml/min/1.73m2) (Fig. 3D). Patients with worse renal function had higher mortality (p<0.001).
Kaplan–Meier survival curves and Log-Rank test. Comparison of patient survival separated byo: A) treatment without RAASB, maintained RAASB and RAASB discontinued. B) Treatment or no treatment with RAASB (p=0.014). C) Under 70 years vs. equal to or greater than 70 years (p=0.003). D) Renal function measured by eGFR CKD-EPI with eGFR≤30ml/min/1.73m2 vs. eGFR>30ml/min/1.73m2 (p<0.0001).
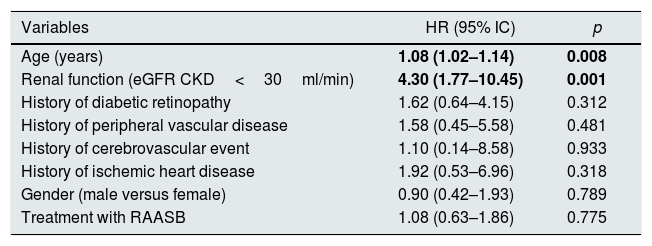
We analyzed the risk factors of higher mortality during the follow-up. In the multivariate Cox regression analysis for proportional hazards, we found that the eGFR <30ml/min/1.73m2 and age are independent risk factors for mortality. And, the treatment with RAASB did not show statistical significance (Table 4).
Multivariate regression analysis of Cox for proportional hazards of mortality.
| Variables | HR (95% IC) | p |
|---|---|---|
| Age (years) | 1.08 (1.02–1.14) | 0.008 |
| Renal function (eGFR CKD<30ml/min) | 4.30 (1.77–10.45) | 0.001 |
| History of diabetic retinopathy | 1.62 (0.64–4.15) | 0.312 |
| History of peripheral vascular disease | 1.58 (0.45–5.58) | 0.481 |
| History of cerebrovascular event | 1.10 (0.14–8.58) | 0.933 |
| History of ischemic heart disease | 1.92 (0.53–6.96) | 0.318 |
| Gender (male versus female) | 0.90 (0.42–1.93) | 0.789 |
| Treatment with RAASB | 1.08 (0.63–1.86) | 0.775 |
RAASB: renin angiotensin aldosterone system blockade; eGFR: estimated glomerular filtration rate; HR: hazard ratio; IC: confidence interval.
Bold values are HR and p values with statistical significance.
The need for RRT was not different in the various SRAAB treatment groups throughout the follow-up period. Thus, the need for RRT (kidney transplant or dialysis) was similar regardless of treatment. Also, we did not observe differences regarding SRAAB and the need for RRT in the combined study of both dialysis and renal transplantation (data not shown).
DiscussionIn our study, we observed that 79% of patients with DKD in our environment have undergone treatment with SRAAB (in 41.5% the treatment is maintained and in 37.5% it is discontinued). In patients with eGFR <30ml/min/1.73m2), the prescription of treatment was less frequent as compared to patients with preserved eGFR.17 The use of RAASB in patients with CKD stages 4–5 is controversial. While there are studies that postulate a beneficial effect, other studies suggest that after its withdrawal there is an increase in eGFR.18 Previous studies have shown that the prescription of RAASB has been increasing over time, suggesting that the emergence of formulas to calculate the eGFR has facilitated the increase in prescription.19 Thus, in Canada a 67% prescription was observed in patients with CKD followed by primary care physician.17 Similarly, 67% of patients affected with CKD stages 4–5 continued treatment with RAASB in Poland.20 In our setting, to our knowledge they are not previous studies designed to determine the prescription of RAASB in patients with advanced DKD.
One of the main targets of the RAASB, besides the treatment of hypertension, is the reduction kidney disease progression in DKD.21,22 Several studies have shown that both ACEIs and ARB are able of reduce the progression of DKD. The RENAAL study analyzed 1513 DM type 2 patients with nephropathy, treated with losartan or placebo in addition to their conventional antihypertensive treatment, and showed that administration of losartan resulted in a delay in the progression of CKD.23 In type 2 DM, normotensive with microalbuminuria followed for 7 years, Ravid et al. observed that treatment with enalapril was associated with a 42% reduction in the absolute risk of developing established diabetic nephropathy and the discontinuation of treatment was accompanied by a worsening of renal function.24 Murakami et al. observed a better renal function in the 2010s compared with that from 2000s in diabetics with advanced CKD, this difference was attributed to the more widespread use of RAASB.19
Regarding the use of double blockade (ACEI–ARB), results from recent studies in patients with DKD, such as the ONTARGET study, contraindicate the use of the combined treatment of ACE inhibitors and ARB, since it results in a decrease in urinary albumin excretion, but at the expense of a decrease in eGFR.25 The European Renal Best Practice Workgroup Diabetes guidelines for the management of DKD patients with CKD stage 3b or greater (eGFR<45ml/min), do not recommend the use of combined ACEI–ARB therapy.10
The RAASB slows down the progression of the DKD.1,7 By contrast, in our study we did not observe differences in the progression of renal function (in terms of plasma creatinine, eGFR and need for RRT) between the groups divided according to treatment with RAASB. These results may be attributed to several facts: 1) worse renal function at baseline, 2) shorter follow-up of patients and 3) small sample size (not being able to reach the necessary statistical power), especially for patients with DKD and eGFR<30ml/min/1.73m2.
Our group patients not treated with RAASB (mentioned in the study as non-RAASB) the initial renal function was worse and patients were older; this may make this group of patients to have a greater and faster deterioration of renal function and a more need for RRT. However, we did not observe a greater need for RRT in any of the groups studied, this effect could be explained by different factors: a) the short time of follow-up (3 years), b) small sample size, and c) age differences between groups.
We observed a statistically significant increase in mortality in the group of patients that never received RAASB as compared to patients that were maintained on treatment, patients older than 70 years and patients with worse renal function (eGFR<30ml/min/1.73m2). However, in the multivariate analysis of independent risk factors for mortality we observed that only age and renal function were statistically significant. Previous studies by our group and others have shown that in patients with terminal CKD, age is an independent risk factor for mortality.26
In relation to the treatment groups, it was observed an association between the patient eGFR and the treatment group. Thus, patients who presented a more precarious renal function and more advanced age were generally excluded from treatment with RAASB. In the group of patients in whom the RAASB was discontinued, there was no improvement in long-term renal function (as per creatinine decrease or increase in eGFR). In contrast, other studies performed in patients with CKD stages 3–4 (48% DM in the maintenance group and 45% DM in the withdrawn group) and hyperkalemia, have shown that maintaining the treatment with RAASB helps to preserve the renal function.27
The RAASB treatment was discontinued in 12% of patients at baseline, in 20% at the first year and in 19% at the third year of follow-up. The main reason was worsening of renal function (87% of total withdrawals), followed by hyperkalemia (10%). This percentage is similar to the previously reports from other studies.28
The main limitations of our study are the small number of participants (especially the group of patients with CKD stages 4–5), the difference in age between the treatment groups (7 years), and the short period of follow-up, which could alter the obtained results. Another limitation is the retrospective nature of the study. Finally, this study was conducted in a single center (Hospital del Mar), the participants were all Caucasian and most of them elderly.
There is an ongoing study called “STOP-ACEi”. This is a multicentre, randomized controlled clinical trial including 410 patients with CKD grade 4–5 on ACE inhibitors, ARB or both. Patients are randomized into two arms: control (continue treatment with RAASB) or treatment withdraw, with 205 patients in each group. The follow-up period will be 3 years and the primary endpoint will be to assess the evolution of renal function.29 Probably the result of this study will help to clarify in this type of patients.
In summary, the results of the present study show that in the population affected by diabetic kidney disease, patients who did not follow RAASB had a worse baseline renal function (increased serum creatinine and decreased eGFR) and advanced age. The evolution of patients who did not receive treatment, in spite of more deteriorated baseline renal function, was similar to the patients who received treatment in terms of need for RRT and cardiovascular events. Mortality was higher in patients with worse renal function and more advanced age. It is necessary to perform studies in populations of similar characteristics of age and degree of renal failure, with longer follow-up. Likewise, new prospective multicenter studies testing the effect of RAASB withdrawal in diabetic patients with advanced renal disease will be very useful in the future.
Authorship/collaboratorsSB and COG have contributed equally to the work.
Conflicts of interestThe authors declare that they have no conflicts of interest.
This work has been supported by the following research grants: Health Research Fund-Carlos III-FEDER Institute (ISCIII-FEDER PI16/00620); Health Research Fund-Carlos III-FEDER Institute (ISCIII-FEDER PI14/00557); and Red de Investigacion Renal Research Fund-Carlos III Institute, RETICS Subprogram (RD16/0009/0013_REDinREN).This work has been performed within the basis of the Doctorate of Medicine of the Autonomous University of Barcelona (UAB).
Please cite this article as: Bermejo S, García CO, Rodríguez E, Barrios C, Otero S, Mojal S, et al. Bloqueo del sistema renina-angiotensina-aldosterona en pacientes con enfermedad renal diabética avanzada. Nefrologia. 2018;38:197–206.