Introducción: Las pobres condiciones socioeconómicas de la población es uno de los causales de la falta de prevención primaria y secundaria de la enfermedad renal crónica e influiría negativamente en la sobrevida de los pacientes en hemodiálisis (HD) crónica. Objetivo: Confirmar si el bajo o nulo ingreso económico de la población incidente en HD es un factor de mal pronóstico vital. Métodos: Utilizamos la población incidente en HD del Registro Argentino de Diálisis Crónica. El seguimiento fue de 12 meses, realizándose un análisis por intención de tratar. Se aplicó el Modelo de Cox para evaluar la asociación entre ingresos económicos y la sobrevida de los pacientes ajustando por edad, sexo, diabetes, comorbilidades, laboratorio inicial y primer acceso vascular. Resultados: Analizamos 13.466 pacientes adultos (edad al inicio: 60,4 [±15,6] años, 57,2% varones, 39,2% diabéticos) que fueron asignados a 2 grupos: 1) «Sin ingresos», 5.661 pacientes (edad al inicio: 60,3 [±15,4] años, 53,1% varones, 41,4% diabéticos); 2) «Con ingresos», 7.805 pacientes (edad al inicio: 60,5 [±15,8] años, 60,1% varones, 37,5% diabéticos). «Sin ingresos» mostró un hazard ratio de 1,19 (intervalo de confianza [IC] 95%: 1,11-1,28) en el univariado; de 1,23 (IC 95%: 1,14-1,32) considerando edad y género; de 1,22 (IC 95%: 1,13-1,31) agregando diabetes mellitus; de 1,26 (IC 95%: 1,18-1,36) agregando comorbilidades; de 1,25 (IC 95%: 1,16-1,35) adicionando laboratorio inicial y de 1,24 (IC 95%: 1,15-1,33) si se incluye acceso vascular transitorio. En todos los modelos la significación resultó en una p = 0,000. Conclusiones: Los bajos o nulos ingresos económicos del paciente en el momento del ingreso a HD es un factor de riesgo independiente de menor sobrevida inmediata.
Introduction: Poor socioeconomic status in the patient population is one of the causes of the lack of primary and secondary prevention of chronic kidney disease and negatively affects the survival of patients on chronic haemodialysis (HD). Objective: To confirm whether the low or absent income of the incident population on HD is a factor of poor prognosis. Methods: We used the incident HD population of the Argentine Registry of Chronic Dialysis. Follow-up lasted 12 months, performing an intention to treat analysis. We applied the Cox model to assess the association between income and survival of patients after adjusting for age, sex, diabetes, comorbidities, initial laboratory results, and first vascular access. Results: We analysed 13466 adult patients (age at onset: 60.4 ±15.6 years; 57.2% were male, and 39.2% diabetic) who were assigned to 2 groups: 1) "no income" group, 5661 patients (age at onset: 60.3 ±15.4 years; 53.1% were male and 41.4% diabetic), 2) "with income" group, 7805 patients (age at onset, 60.5 ±15-8] years; 60.1% were male and 37.5% diabetic). The "no income" group had a hazard ratio of 1.19 (95% confidence interval [CI]: 1.11-1.28) in the univariate analysis, 1.23 (95% CI: 1.14-1.32 ) considering age and gender, 1.22 (95% CI: 1.13-1.31) by adding diabetes mellitus, 1.26 (95% CI: 1.18-1.36) by adding comorbidities, 1.25 (95% CI: 1.16- 1.35) by adding the initial laboratory results, and 1.24 (95% CI: 1.15- 1.33) if temporary vascular access is included. All models resulted in a significance of P=.000. Conclusions: Low or no income of patients at the time of entry into HD is an independent risk factor for immediate lower survival.
INTRODUCTION
The total population in Argentina reached 39 745 613 inhabitants in the year 2008, an approximate 1% population increase since 2004.1 The incidence rate of patients on chronic dialysis (CD) increased by 4.38% during this time period, from 137.5 to 143.1 patients per million population (pmp), a 1.1% increase each year. The prevalence rate of CD increased by an even greater percentage (3.2% annual), increasing from 550.3pmp in 2004 to 623.4pmp in 2008.2,3
Chronic kidney disease (CKD) causes very high rates of morbidity and mortality, proportional to the CKD stage, with 30 times higher rates of cardiovascular mortality in stage V patients. This depends, among other factors, on the availability of access to renal replacement therapy and to a greater extent on access to primary and secondary kidney disease prevention measures in early stages of the disease.
It can be said that there are no restrictions on the availability of chronic dialysis treatment in Argentina. Any citizen that reaches a stage of terminal renal failure (TRF) with the need for dialysis is accepted by both public and private health centres. Even so, the low adjusted incidence rates of patients entering CD in some Argentine provinces lead us to strongly suspect that the health systems in these areas suffer some level of deficit in communication with chronic kidney disease patients.2,3 Consequently, it is quite probable that the totality of the Argentine population is not being contacted in time using the correct methods in order to carry out primary and secondary prevention measures for kidney disease.
In addition to this inequality in the detection of kidney disease, over one third of the incident population on CD lives in poverty.2,3 Major epidemiological studies carried out at the national level have shown that poverty indicators are observed in between 30% and 33% of the general population. The study carried out by the Catholic University of Argentina (Universidad Catolica Argentina) also shows that 14.6% of homes have a severe housing deficit. As of 2009, 31.6% of homes had no seweage system, 9.8% were without running water, and 8.8% of households were overcrowded (a strong indicator in the “unsatisfied basic needs index”); additionally, 15.9% of homes have incomes that do not satisfy their basic food needs (10.8% moderate and 5.1% severe).4
Life in situations where basic needs are not met, more commonly known as poverty, has not been examined thoroughly as a risk factor for mortality in the population of patients on CD using indexes or adequate multivariate studies, since, in order to understand its true effect, the socioeconomic variable must also be adjusted for other variables known to affect mortality in these patients. The few studies that have mentioned the poor conditions of CD patients suggest that these conditions have negative effects on survival, as well as on the probability of having access to a kidney transplant. By using a multivariate analysis to design a new prognostic index, we were able to demonstrate that insufficient income for patients and their family members was a variable of negative prognosis for the 1-year survival of 5360 new incident patients on chronic haemodialysis, giving a score of 1 for the final score obtained, where a higher score indicates a lower survival rate.5 Additionally, Abraham et al in India and Caskey et al in England-Wales found an association between poor socioeconomic conditions and a higher mortality rate on dialysis. In this last study, the authors observed a lower probability of transplant in the group with the greatest economic need.6,7 However, Eisenstein et al, in a study from the USA based on estimated income by housing area and race, found no significant differences in mortality rates while on haemodialysis among the different income level groups (low, middle, and high).8
The aim of this study was to analyse whether a low or absent income in the incident population on chronic haemodialysis is a factor for a poor prognosis, adjusting for the variables that have been shown to influence 1-year survival.
METHODS
Observational, retrospective, longitudinal and predictive analytical study.
Selection
We used the data obtained through the National Registry of Chronic Dialysis. In Argentina, it is mandatory to register patients when they enter or exit a CD programme. When the patient is admitted into a programme, a questionnaire called the first registry of a chronic dialysis patient (primer ingreso de paciente a dialisis cronica, DRI) which, signed under oath by the CD Centre Director, must be submitted to the central office of the Registry under the Central Coordinating Institute for Ablation and Implants (Instituto Central Único Coordinador de Ablación e Implante, INCUCAI). The questionnaire includes demographic variables, pre-existing diseases, initial laboratory results, and socioeconomic and occupational variables from when the patient first started chronic dialysis treatment. This form must be completed by the attending nephrologists and social workers.9 Insufficient or absent income is very closely checked through the evaluations made by the social workers both through a review of paperwork and on-site evaluation of the living conditions at the patient’s home in order to corroborate or disprove the information provided.
Our study included patients 18 years of age or older that started for the first time a chronic haemodialysis (HD) programme in any of the haemodialysis centres (n=462) in Argentina (24 provinces) between 1 April 2004 and 31 December 2008. The observation period came to a close on 31 December 2009, in order to guarantee a theoretical follow-up period of one year. We excluded all patients that did not have complete data for all variables considered in the study. The patients were censored in the case of recovered renal function, and event was defined as the death of a patient. As such, we performed an intention to treat analysis, with follow-up until patient death, whether or not the patient underwent a transplant. The start time for the follow-up period was day 1, and so all patients were included, even those with less than 90 days of follow-up.
The population was divided into two groups: 1) “No income,” including patients that did not have any income declared, from neither the patients themselves or those who shared their home, at the start of treatment. 2) “With income,” including patients with declared income at the start of treatment.
Statistical Method
Continuous variables were expressed as mean and standard deviation, and categorical variables were expressed in terms of frequency and proportion. For the comparison of numerical variables from both groups, we used Student’s t-tests for parametric variables and Wilcoxon tests for non-parametric variables; we used Pearson’s chi-square test for qualitative variables, and considered a P-value <.05 to be statistically significant.
In the survival analysis, we used the Kaplan-Meier (KM) method. We used the log-rank test (Mantel-Cox) for a simple comparison between the two populations.
We applied five different Cox proportional hazards models to test for differences between the two groups, adjusting for covariates that were considered to be predictive a priori based on previous studies.3,5 We determined hazard ratio (HR) or Exp (B) values for the independent variable “income” (dichotomous: no income and with income) after adjusting for the effect of other independent variables in the equation. The variable “income” was present in all models. In all cases, variables were considered as pre-existing conditions or conditions at the start of the therapy. We excluded those independent variables that were highly correlated with each other. The proportional hazard was calculated based on log (-log) survival.
Model 1. “Age at start of treatment” and “Male” (3 covariates).
Model 2. To the previous variables we added: “Diabetes mellitus as a cause of TRF” (4 covariates).
Model 3. In addition to the previously mentioned variables, we added the following comorbidities as dichotomous variables (yes/no): “Presence of persistent angina or background of myocardial infarction”, “presence of arterial hypertension”, “presence of cardiac arrhythmia”, “presence of congestive heart failure”, “presence of chronic pulmonary disease”, “presence or background of cerebrovascular disease (including dementia, hemiplegia)”, “presence of peripheral vascular disease (including amputated patients)”, “solid cancer without metastasis in the last 5 years (excludes basal/squamous skin cancer)”, “solid cancer with metastasis in the last 5 years”, “acute and chronic leukaemia”, and “lymphoma (includes myeloma according to the Charlson criteria)” (15 covariates).
Model 4. In addition to the Model 3 variables, we added the following variables from the initial laboratory Results: “positive HIVAb”, “positive HBsAg”, “positive HBVAb”, “initial albumin <3.5g/dl”, “initial haematocrit”, and “initial glomerular filtration rate” (glomerular filtration rate according to the abbreviated Levey formula MDRD-7)10 (21 covariates).
Model 5. In addition to the Model 4 variables, we added “starting haemodialysis with a temporary vascular access (non-tunnelled catheter)” (22 covariates).
We performed all statistical analyses using SPSS version 15.0 statistical software for Windows (SPSS Inc., Chicago, IL).
RESULTS
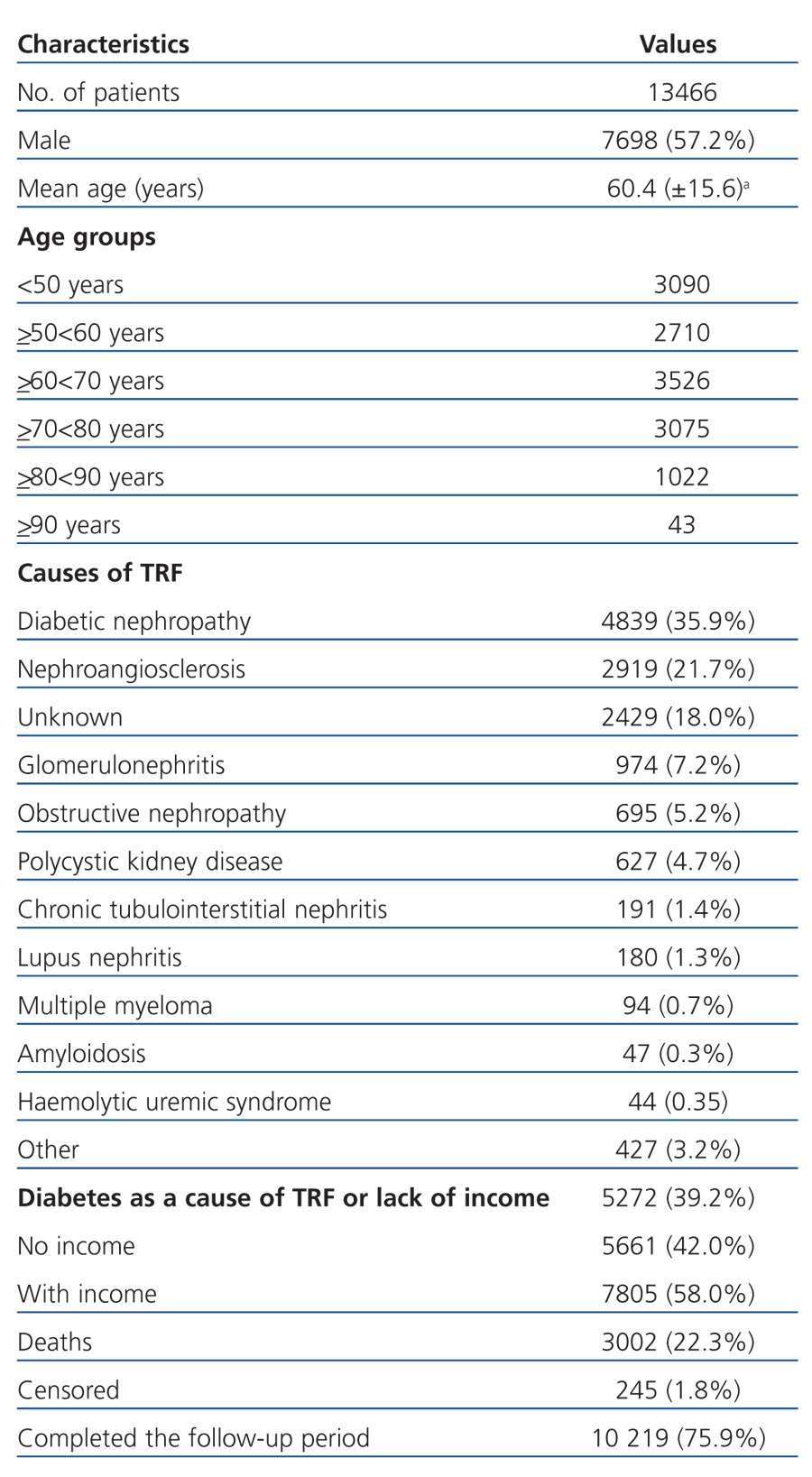
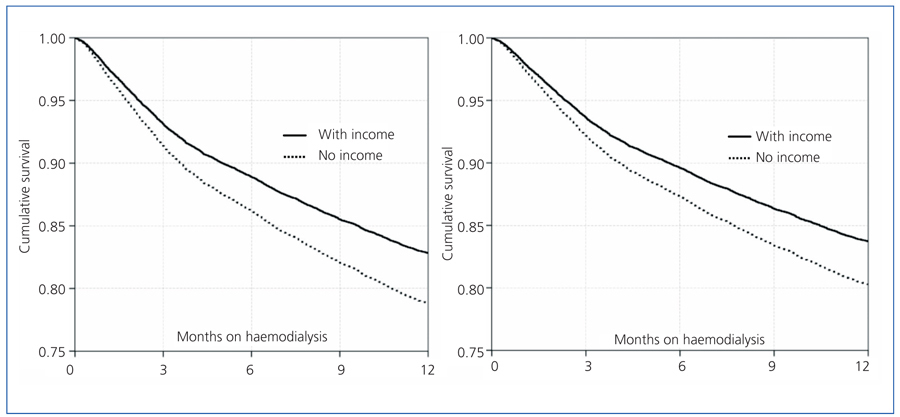
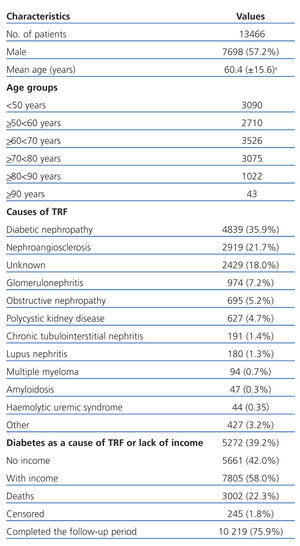
We evaluated a total of 13 466 patients. Table 1 summarises the characteristics of the study population. Upon starting HD, 56.7% of our patients were 60 years of age or older. Diabetes was present as a cause of TRF in 35.9% of the total, although 39.2% of the incident population was diabetic. The patients that reported no income within their household were 42.0% of the total. Overall mortality at 1 year was 22.3%, and 1-year survival was 77.7%. Only 1.8% of patients had to be censored from the study, with 245 recovering renal function.
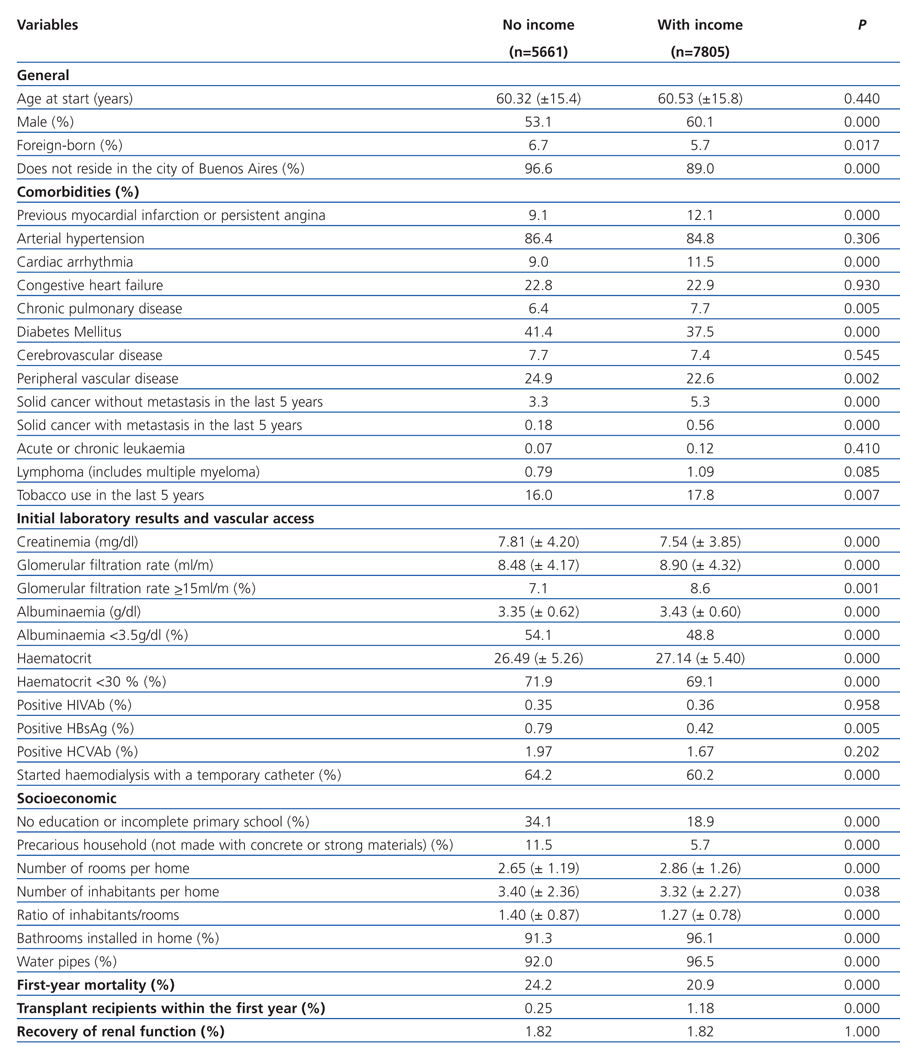
Table 2 displays general patient variables, comorbidities, laboratory results, type of initial vascular access, and the socioeconomic conditions for both groups and the corresponding statistical comparisons between them. The “no income” group had a significantly higher proportion of males, foreigners, people residing outside of Buenos Aires, and a similar mean age as compared to the other group. Upon analysis of the comorbidities present, although the “no income” group had a significantly higher percentage of diabetic patients, we found only one variable (a priori with a worse prognosis) that yielded a significantly higher percentage for this group: the presence of peripheral vascular disease. On the other hand, we observed a significantly lower percentage of angina and previous heart attack, arrhythmia, chronic pulmonary disease, cancer, and tobacco use in the “no income” group.
In terms of laboratory results, the “no income” patients started treatment with significantly worse conditions for almost all variables: lower glomerular filtration rate, lower albuminaemia, lower haematocrit, greater percentage of HBsAg positive, etc. Additionally, the use of a temporary non-tunnelled catheter was significantly more common in this group as the first vascular access point established.
The variables associated with socioeconomic status were also significantly worse for the “no income” group: lower level of education, greater instability in their living situation, and a larger number of people in each home (ratio of inhabitants/rooms), among others.
The mortality rate after one year was significantly greater in the “no income” group: 24.2% vs 20.9%. We observed a very significant difference (P=.000) between the two groups in the number of patients that underwent transplants. In the “no income” group, 0.25% (14/5661) of patients underwent transplants, and in the “with income” group, 1.18% (92/7805). This difference was the basis for performing an intention to treat analysis, considering all transplant recipients with a maximum follow-up period of 12 months.
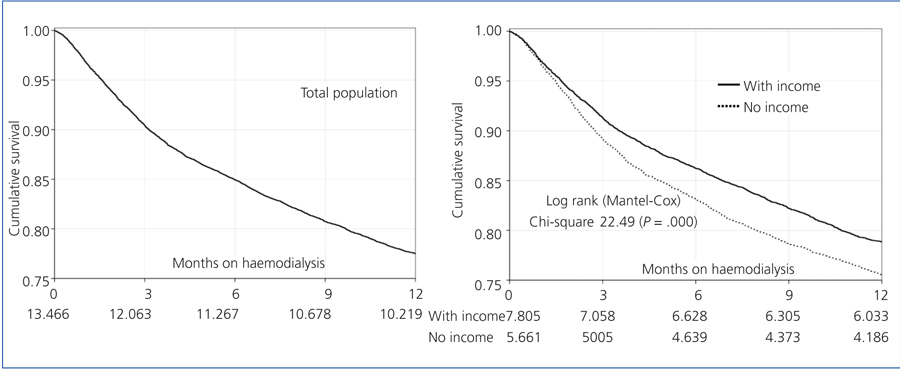
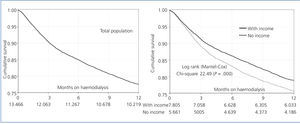
The KM survival curves for the overall population and by group are displayed in Figure 1: total survival after one year was 77.71%. Survival in the “with income” group was significantly higher than in the “no income” group: 79.12% vs 75.76%, and the log-rank test (Mantel-Cox) resulted in a chi-square value of 22.49 (P=.000).
To confirm these findings, we used a univariate Cox regression model that yielded an Exp (B) or hazard ratio (HR) of 1.19 for the “no income” group (95% confidence interval [CI]: 1.11-1.28). Considering other covariates in the equation, we will see whether the result is the same.
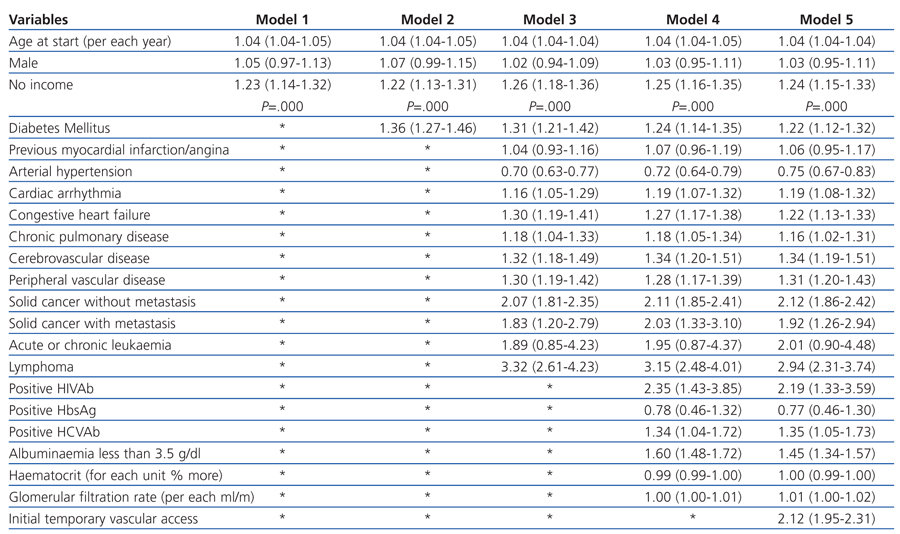
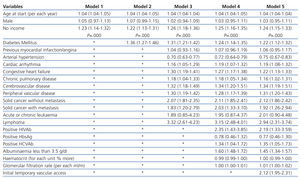
Table 3 displays the HR for the variables included in each of the five multivariate regression models used, with special emphasis on the variable “no income.”
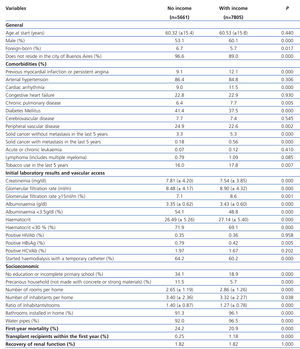
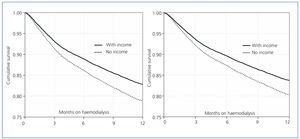
Figure 2 shows the Cox predictive curves for models 3 and 5 for a typical individual (theoretical predictive survival) after adjusting for all covariates for the categorical variable of “with or without income.”
The HR for the “no income” group did not change significantly in any of the five multivariate models. It did improve compared to the univariate model, although this difference did not reach statistical significance. The presence of comorbidities in model 3 produced the highest HR value (1.26), which decreased when the initial laboratory analysis values were added in model 4, and even more so when adjusting for vascular access in model 5. However, the differences are small, which implies that whether with or without adjustment, the lack of income for patients on HD is an immediate factor for a poor prognosis, regardless of the presence of other factors.
Additionally, we performed a sixth Cox multiple regression model, which considered 4 variables: “no education or only incomplete primary school, “unstable living situation”, “male sex”, and “age at the start of treatment”. The two first variables did not enter into models 1 and 5 because of their close correlation with “no income”; for the same reason, “no income” was not evaluated in this sixth model. “Unstable living situation” had an HR of 1.38 (95% CI: 1.21-1.58; P=.000). “No education or only incomplete primary school” had an HR of 1.09 (95% CI: 1.00-1.18; P=.046). This is simply another manner of evaluating poverty-indigence and its repercussions on immediate survival on HD: the absence of an adequate home significantly increased the relative risk of death by 38%, after adjusting for age, sex, and level of education.
DISCUSSION
A home is considered to be poor if the “per capita” income is insufficient to cover the basic needs for food and other amenities (total basic needs) of its inhabitants, including clothing, education, transportation, and health. Additionally, if the home does not have sufficient income to provide adequate sustenance to its members (basic dietary needs), the inhabitants are considered to be indigent or extremely poor.
We cannot consider the declarations of patient income to be absolutely correct; however, this declaration was certified by on-site evaluations in plain view of the living situations in the majority of cases where patients declared that they did not have any income in their households. We have observed in this study that the differences in education and households are notable between those that declare income and those that do not. This variable, therefore, is strongly associated with indigence or poverty. It is quite probable that patients that do not declare income do receive some type of economic subsidy after starting renal replacement therapy. However, this cannot be determined here for lack of data on the subject. Even so, we could observe in our study that the relative risk of death in the first year of hemodialysis treatment was significantly higher (19% to 26%) in patients that declared no income as compared to those that did declare an income.
Diabetes mellitus is a poverty-linked disease; as Table 2 shows, this condition was significantly more prevalent in the “no income” group. Confirming the results from our study, Caskey et al in England and Wales observed that diabetes was a cause of TRF at a much higher rate in the population living in areas of greater social deprivation.7 Also, Lorenzo et al performed an evaluation of the high prevalence of diabetes in the Canary Islands (Spain), and found that, among other causes, poverty and social inequality were causative forces for reduced use of health resources, lower rates of compliance with treatment, and inadequate hygiene-diet habits, leading to increased prevalence of diabetes mellitus in predisposed individuals.11 The initial laboratory results and a greater frequency of non-tunnelled temporary catheters as the first vascular access point provided showed that “no income” patients had worse conditions than “with income” patients, all of which is probably related to delayed contact with the health system.
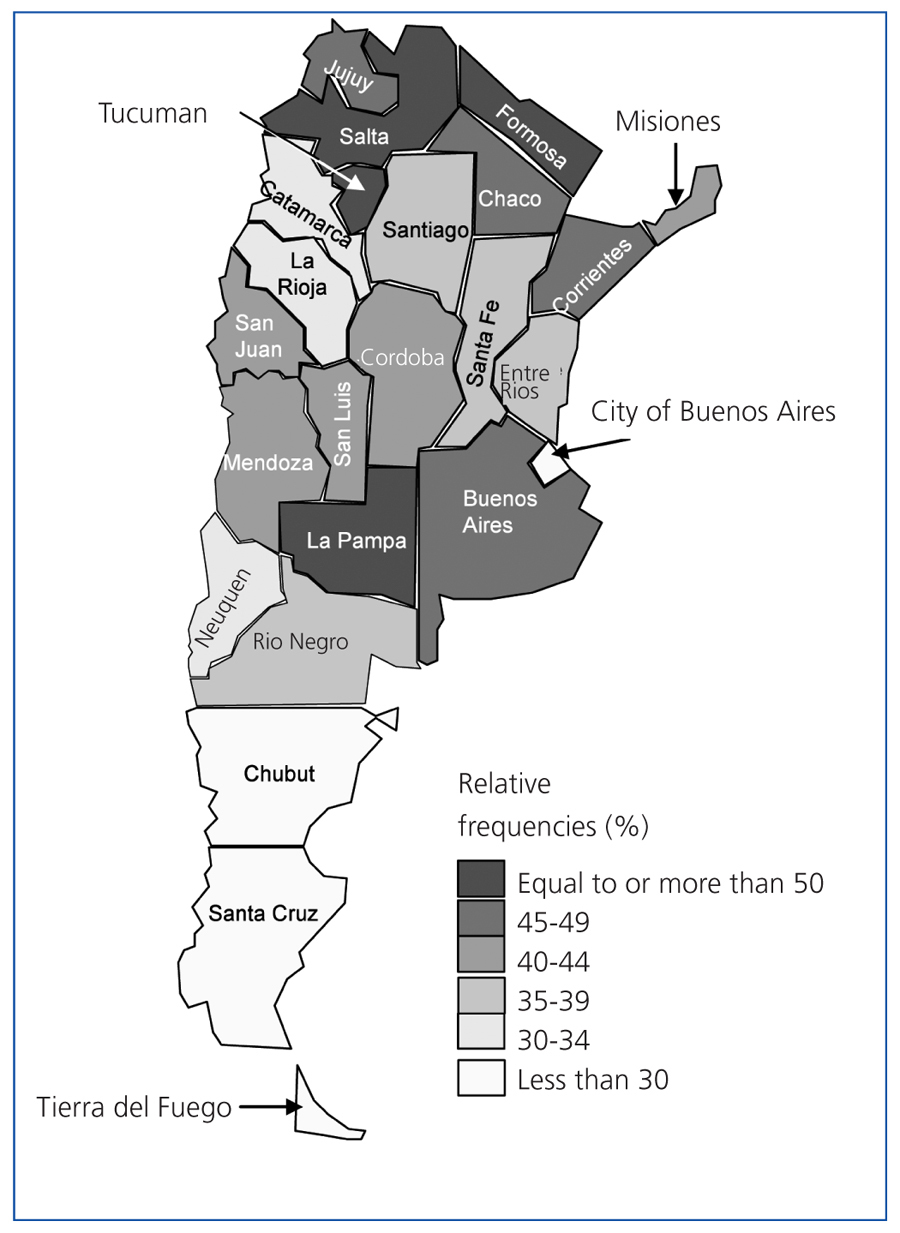
The location of the patient’s residence is also an influential factor: the city of Buenos Aires (not including the outlying urban areas) has been considered in other studies2,3 as the “gold standard” for renal health in Argentina, since it has the best indicators in the entire country: more advanced age upon starting a CD programme (which implies a better treatment of kidney disease and consequent delay in reaching stage 5 TRF), lower incidence rate of CD (due to better prevention methods), a higher rate of kidney transplant, and a better adjusted survival rate of patients on CD. Buenos Aires has the best health infrastructure in Argentina, especially for poor and indigent patients. In our study, we have found that this city is one of the four districts that have the lowest rates of “no income” patients in the entire country, 18.2%, significantly lower than the national mean of 42%.
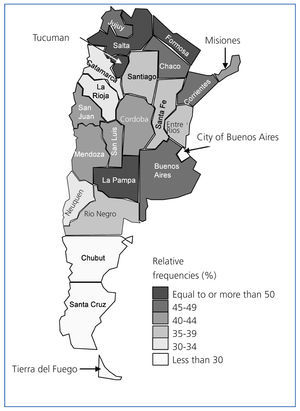
Observing a map of Argentina (Figure 3), we can see major inequality between the different provinces in income in the homes of incident patients on HD. The majority of the north-western provinces (Tucuman, Salta, and Jujuy), all of the north-eastern provinces (Formosa, Chaco, Corrientes, and Misiones), three of the central provinces (La Pampa, Buenos Aires, and Cordoba), and all of the cuyo provinces (Mendoza, San Juan, and San Luis) have percentages greater than 40%. All other provinces have lower percentages, with the lowest observed in the southern provinces of Patagonia (Chubut, Santa Cruz, and Tierra del Fuego) and the city of Buenos Aires.
Some 42% of the Argentinean total corresponds to the incident population on HD between 2004 and 2008. However, it is heartening to know that the percentage of patients with no income declared decreased over time from 61% of incident patients in 2004, to 52% in 2005, 46% in 2006, 35% in 2007, and finally 22% in 2008.
“Lack of income” was demonstrated to be a predictive factor for low survival after one year in patients on HD, although the HR obtained, in spite of its significance (P=.000), appears to be quite low, and we would have expected to observe a value higher than 1.22-1.26. As an explanation for this “relatively low” HR value, we could hypothesise that the lack of economic resources is a reliable reflection of a lifestyle in which the basic needs are not met, and that probably the HR was not higher because, once attended by the health system, the patient moves from being very vulnerable to less vulnerable. Care is provided as soon as he/she starts haemodialysis: social workers are sent to the home, the poor living conditions are recognised, a better household and more food are acquired through the county, provincial, or national government aid systems, and some sort of economic subsidy is provided. That is to say, after starting renal replacement therapy, the patient is often the recipient of several actions that are not considered in our study, and that eventually change the status of the patient from one of very high risk to one of moderate risk in the “no income” population.
Another finding from our study was the fact that the “no income” population had a significantly lower rate of access to kidney transplants than the other group during the first year on HD: 0.25% vs 1.18%. Both values are low, but the value for poor patients is much lower. The causes of this phenomenon are still unknown, but hypothetically, poor patients must go through much more bureaucratic processes (with a greater loss of time) in order to be included on the kidney waiting list.
The quality of health care provided to renal patients, in particular renal replacement therapy, whether through dialysis or transplant, has been the subject of a large number of medical publications. Many authors have dealt with the subject, examining all of the different factors that influence the survival of these patients. However, very few studies have made the attempt to include and evaluate the incidence of socioeconomic factors (for the patient and family members) in the treatment results. In a literature review we observed that some of these studies have certain local and methodological factors that impede the possibility of generalising these results across other populations. The various methods used to measure poverty and low socioeconomic status, for instance, and the different responses of health systems to high dependency patients, such as those with renal failure, makes comparisons difficult. In the USA, a strong relationship was shown between a low socioeconomic status and a high mortality rate,12,13,14 whereas other researchers in the same country could not find these results.8 Abraham et al in southern India examined 558 CD patients, finding that mortality was higher at lower socioeconomic levels (especially among diabetics), as well as a lower level of access to kidney transplants; but the extremely poor access to treatment, the fact that these patients receive treatment at different institutions, and the young age of the prevalent patients does not allow us to make comparisons.6 The study by Caskey et al showed that low-income patients are referred for treatment late in the progression of the disease, have a lower probability of undergoing peritoneal dialysis, undergoing a kidney transplant, and reaching target haemoglobin and phosphorous values after one year of treatment, and have a higher mortality rate under the age of 65 years. This lower survival rate remained significant even after adjusting for age, sex, and the underlying cause of the renal failure, but was corrected when adjusting for comorbidities. The authors inferred that these factors should be responsible for the difference. However, in this study, social deprivation was based solely on the characteristics of the area or neighbourhood where the patient was living, which is a completely indirect method with a high margin of error.7 Our study, which was based on the entire incident population in Argentina during a given period and used a survey taken upon starting HD, with the final result of survival after one year, has certain aspects that have not been explored previously. Our results reinforce the idea that, in addition to the absence of income, an unstable household and low level of education are both statistically significant independent risk factors
Our study did have some limitations: 1) Absence of races and ethnicities. Since colonial times, Argentina has been the site of substantial racial mixing, which was enhanced by the three large waves of immigrants that arrived here between 1880 and 1950. As such, it is difficult to establish patterns of race and ethnicity. The self-recognised indigenous population was only 1.56% of the total population in 2004-2005.15 There are no official data for people of African heritage (Afro-Argentine), but this ethnicity is thought to make up only 0.03% of the total population. 2) The study is not reproducible in societies where the level of poverty and indigence is very low. It is, however, in other Latin American countries where access to renal replacement therapy is also universal and where the patterns of poverty are similar to Argentina: in particular, Uruguay, Chile, and Brazil.16
It is quite probable that the indigent and poor people of Argentina have a very late contact with the health system, which could be due to a lack of information, the need to deal with their basic needs at all times, the lack of time to spend in long lines at public hospitals, or the lack of health centres and public hospitals close to their place of residence. For some or all of these reasons, these patients do not have access to a healthy life. The vulnerability of this population is extreme. This is not just an issue of renal health, or even public health: this is a social problem that has its roots in the highest circles of social health policy, and will not be solved or even improved until it is approached from this perspective. It will improve when the social, cultural, economic, and health status of the population improves, and when the level of inequality is reduced.
High poverty indices were once the exclusive domain of developing countries, but in the economic crisis of the last few years, large portions of the population in developed countries have begun to enter these conditions or are about to. As such, these countries may do well to anticipate these changes by developing containment policies directed at the population with renal failure and a low socioeconomic level.
In conclusion, “lack of income” was shown to be a predictive factor for low survival after one year on HD, after adjusting for age, sex, diabetes, comorbidities, albuminaemia, glomerular filtration rate, haematocrit, and the initial type of vascular access. We propose the consideration of this variable or another similar measure that represents low or absent income in the incident HD patient, adjusted for other factors, in order to adequately predict short-term survival.
Table 1. Basic patient characteristics
Table 2. General variables, comorbidities, initial laboratory results, and socioeconomic conditions of each group
Table 3. Multivariate Cox proportional hazards models
Figure 3. Percentage of incident patients on CHD in 2002-2004 that declared no income (patients and house members). Distribution by Argentine province
Figure 2. Left: Cox predictive curves for Model 3 using the dichotomous variable of with or without income. Right: predictive curves for model 5, also for the dichotomous covariate of with or without income
Figure 1. Kaplan-Meier survival curves