Antecedentes: Estudios sobre la calidad de vida relacionada con la salud (CVRS) en adultos con enfermedad renal crónica (ERC) han demostrado que situaciones clínicas como el número de ingresos o la anemia afectan a su calidad de vida. Existen muy pocos estudios similares en niños. Objetivo: Analizar el impacto de variables analíticas y de la situación clínica en la CVRS de los pacientes pediátricos con ERC. Pacientes y métodos: Estudio transversal utilizando el cuestionario TECAVNER en 71 niños con ERC y en sus padres (33 trasplantados, 11 en diálisis peritoneal, 5 en hemodiálisis, 22 en tratamiento conservador). Se analizaron variables analíticas (nitrógeno ureico en sangre, creatinina, hematocrito, albúmina) y situación clínica (talla baja, hipertensión arterial [HTA], deformidades óseas), número de ingresos y días de ingreso en los seis meses previos a la realización del estudio, así como número de fármacos administrados, restricción de líquidos o dieta. Resultados: uno de los factores que más distorsiona la calidad de vida de nuestros pacientes es la restricción hídrica. La HTA afecta a la función cognitiva de los niños. El hematocrito superior a un 35 % mejora la función y la actividad física. No encontramos relación entre valores de albúmina y CVRS. Conclusiones: Estos resultados confirman las hipótesis previas y contribuyen a dar validez al cuestionario TECAVNER.
Background: Studies examining health-related quality of life (HRQOL) in adults with chronic kidney disease (CKD) have demonstrated that certain clinical situations such as number of hospitalisations and anaemia can affect patient quality of life. Very few such studies have been carried out in children. Objective: To analyse the impact of laboratory variables and various clinical situations on HRQOL of paediatric CKD patients. Patients and Method: We carried out a cross-sectional study using the TECAVNER questionnaire in 71 children with CKD and their parents (33 transplanted patients, 11 on peritoneal dialysis, 5 on haemodialysis, and 22 on conservative treatment). We analysed laboratory variables (blood urea nitrogen, creatinine, haematocrit, and albumin), clinical situation (short stature, arterial hypertension, and bone deformities), number of hospitalisations, and days spent in the hospital in the previous 6 months, as well as number of drugs administered and fluids/diet restrictions. Results: The factor that most heavily affected the quality of life of our patients was water restrictions. In addition, hypertension affected cognitive function in these children. A haematocrit value >35% improved physical activity and functionality. We observed no association between albumin and HRQOL. Conclusions: These results confirm previous hypotheses and contribute to the validity of the TECAVNER questionnaire.
INTRODUCTION
Measuring health related quality of life (HRQOL) allows us to evaluate the functional effects of a disease on a patient as perceived by himself and the aspects of life affected by the disease and treatment.1,2 Functional state would be the objective consequence of state of health, whereas HRQOL could be considered as the subjective consequence of state of health.3,4 HRQOL is concerned with how the patient feels, and is affected by numerous personal, social, and environmental factors, in addition to the medical condition of the patient.
Several metabolic alterations are produced in chronic kidney disease (CKD) that contribute to producing hyperparathyroidism, malnutrition, anaemia, and accelerated arteriosclerosis.5 In addition, the treatment of CKD leads to diet restrictions, in which certain foods are restricted and others are eliminated altogether, fluid restrictions, and pharmacological treatments (generally several drugs with multiple administration schedules). Patients are frequently required to attend clinical control evaluations and are even hospitalised with a certain periodicity, which hinders the patient’s ability to live a normal lifestyle and reduces his quality of life (QOL). Infancy, being a very important stage of growth and development, also implies different clinical aspects, such as bone deformities and short stature, which can also be a detriment to the QOL of paediatric patients. It is important to consider that as the complexity of a treatment regimen increases, so does the difficulty of compliance with the regimen, especially in adolescents. In this context, a lack of adherence to treatment prescriptions is one of the factors that most heavily influences clinical deterioration, and can lead to kidney transplant loss and patient instability, which in turn further hinders HRQOL.
Although the interest in this topic is growing within the medical field, few studies have examined HRQOL in children with CKD because of the difficulty inherent to this type of study, due to the lower prevalence of CKD as compared to the adult population, making it problematic to compile large sample sizes. This is compounded by the lack of questionnaires specifically designed and validated for paediatric patients with this disease, which may lead to discordance between results.6 With this in mind, we designed a specific QOL questionnaire for use in children with CKD (TECAVNER), the only such survey in the Spanish language.7 In 2008, the Goldstein group6-8 published the first questionnaire specifically designed for children with CKD in English, and since then, to the best of our knowledge, no further developments in this field have been made, which serves as an indication of the complexity of this subject. The Spanish group of Riaño et al.9 also examined HRQOL in this disease, but only in adolescents with terminal kidney disease. Since this study used a generic QOL survey that was not specifically designed for use in patients with kidney disease, the differential characteristics unique to this disease were not registered. The same occurred in the largest such study we know of, involving 400 children with CKD, which included patients aged 2 years or more and in early phases of kidney disease, but using a generic questionnaire.10
The majority of studies involving HRQOL in adults and children with CKD have analysed this variable in relation to the modality of the treatment, concluding that the best renal replacement option is kidney transplantation, with some discrepancies found regarding haemodialysis (HD) and peritoneal dialysis (PD),11 although in general, patients on PD tend to have a better QOL.12,13 Our paediatric patients also report a better QOL with kidney transplants, followed by PD and finally HD.14 Of the few studies involving children, the study by Varni et al. stands out,15 in which HRQOL was compared among children with 10 different chronic diseases and healthy subjects through the use of a generic questionnaire. This study concluded that globally, children with CKD have a worse QOL than healthy individuals, and those on HD have a significantly worse QOL in general and inferior physical health than those who had received kidney transplants. The parents of patients on HD also had a worse perception of their children’s health, whereas the parents of children on PD only reported worse emotional effects as compared to children who had received kidney transplants. Riaño reported less satisfaction with state of health in adolescents on dialysis as compared to healthy individuals, but found no differences between transplanted patients and health subjects. This may be due to the use of a generic questionnaire that does not cater to the characteristics specific to the disease. Goldstein, in the only study involving a questionnaire specifically designed for children with terminal kidney disease, also described that parents of children who had received transplants perceived a better QOL in their children than those on dialysis in all aspects, except for physical appearance (perhaps due to the effects of immunosuppressants and corticosteroids). However, their children did not reflect the same differences in terms of treatment type (transplant vs dialysis), except for in the field of interactions with family and friends, which was better among transplanted patients than in those on dialysis.8 This author published discordant results in a previous study in the same population but using a generic questionnaire,16 which tends to be the source of differences found between the majority of publications on the subject. As such, several authors have voiced support for simultaneous use of both types of questionnaires (generic and specific) in addition to taking into account the opinions of the affected children and their relatives for the analysis of this heterogeneous and uncommon population of patients.
By examining HRQOL in our patients, we were interested in analysing not only therapeutic modality, but also the impact of clinical situation, laboratory parameters, and treatment regimens. In this manner, we can act upon these other potentially important factors so as to improve QOL, which in turn translates into improved compliance with treatment and longer survival with improved quality.
PATIENTS AND METHOD
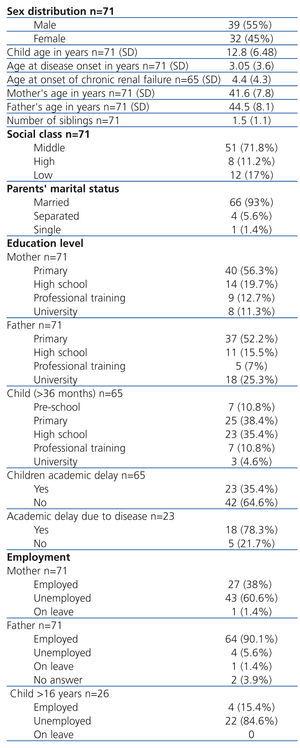
We performed a cross-sectional study in children with CKD in order to examine the influence that clinical and laboratory variables have on HRQOL. Our study population involved children treated at the Gregorio Marañón University Hospital (Madrid) during a five-year study period. A total of 71 patients with CKD were included in the final sample (all with more than 3 months evolution). Of these, 33 had received kidney transplants (Tx), 16 were on renal replacement therapy (11 on PD and 5 on HD), and 22 were on conservative treatment regimens. Of the overall sample, 42 were older than 9 years of age (11 on conservative treatment, 4 on PD, 2 on HD, and 25 with Tx). The sociodemographic variables and clinical situations of each patient are summarised in Table 1 and Table 2.
All patients participated voluntarily in the study after receiving a verbal explanation of the study parameters and giving their consent for inclusion.
We used the TECAVNER questionnaire (QOL test specifically designed for paediatric patients with kidney disease) developed for this study.7 The questionnaire was answered by children 9 years of age or older and their parents, and in the case of children younger than 9 years of age, only by their parents.
We also compiled: a) laboratory variables (blood urea nitrogen, creatinine, haematocrit, albumin, and glomerular filtration rate); b) clinical variables: arterial hypertension, short stature, bone deformations, and number and duration of hospitalisations during the six-month period prior to the study; and c) pharmacological treatment, diet restrictions (protein and/or salt restrictions), and fluid restrictions.
Statistical analysis: we expressed all results in the descriptive analysis as mean and standard deviation for quantitative variables, and as percentages or frequencies in the case of qualitative variables. We then performed a simple or bivariate analysis to reveal associations between variables, using chi-square tests for qualitative variables and Fisher’s exact tests when chi-square test was not an option. We also used ANOVA tests to compare the means of two independent groups. We used SPSS statistical software for all statistical analyses. We also considered a P-value ≤.05 as statistically significant in all cases.
RESULTS
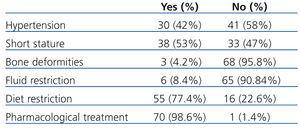
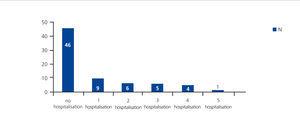
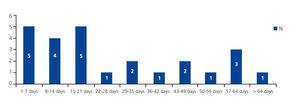
Table 3 shows the results for laboratory parameters. Table 4 summarises the results for hypertension, short stature, bone deformations, pharmacological treatment, and diet and fluid restrictions. Of the 8.4% (6 patients) under fluid restrictions, 100% complied with restrictions and 50% were bothered by them. As regards diet restrictions (salt or protein limitations), these were prescribed in 77.4% of cases, and of these 96.3% complied with restrictions, while 58% were bothered by them. Pharmacological treatment was prescribed in 98.6% of cases, with 100% compliance, and 30% were bothered by drug treatments. Figure 1 and Figure 2 show the distribution of patients according to the number of hospitalisations and number of days hospitalised during the six months prior to the study. Table 5 summarises the TECAVNER results as indicated by the children and their parents (TECAVNERCP), with statistical significance values.
DISCUSSION
It has been shown in adults that several clinical factors, in addition to treatment modality, exert considerable influence on HRQOL. One of the most heavily studied of these factors is anaemia, but we believe that there are several conditions that could also affect QOL in children, such as hypertension, duration of hospitalisation, and short stature.
Since diet prescriptions are a key component of the CKD treatment, with limitations of certain foods and fluid restrictions being very common in these patients, we sought to evaluate whether lifestyle guidelines and treatments influenced the QOL of our paediatric patients, particularly in the form of water restrictions, diet restrictions, and pharmacological treatments. All patients followed our recommendations for fluid restrictions and drug treatments, and almost all complied with diet restrictions, even though half of all patients reported that they were bothered by these regulations, above all by the fluid and diet restrictions. These results indicating extremely high compliance rates could be due in part to the fact that the patients’ mothers were ensuring proper treatment, since inadequate compliance with treatment is very common in daily clinical practice, especially among older adolescents who are independent of their parents. It is worth mentioning that 60% of the mothers of our patients stay at home in order to take care of their children.
We did not observe any significant differences in QOL between diet restriction categories, with 77% of children on some form of diet restriction. We were unable to evaluate significant differences in terms of drug prescriptions, since except for one case, all of our patients received multiple pharmacological treatments. However, the children and their parents stated that they considered it to be very important that the schedule for taking the drugs should adjust to their daily lifestyles and preferred a single administration per day or a maximum of twice per day. This avoids the need for taking medications at school or outside of the home, thus reducing the risk of missing an administration or the need for additional personnel to take responsibility for correct dosing.
Fluid restrictions did represent alterations for the children (TECAVNER) in terms of social function and general health. Physical activity was also affected, according to the opinions of both the children and their parents, with better physical activity reported by those who were not prescribed fluid restrictions.
As such, it appears that fluid restrictions affect the QOL of our patients more than diet restrictions, and this could be one of the factors contributing to the inferior QOL in patients on HD, since all of these are under fluid restrictions. We have not found any studies in the medical literature that assess these variables in paediatric patients.
Hypertension also influenced the QOL of our patients. Hypertension affected cognitive functioning in the questionnaires responded by the paediatric patients, and the fields of physical activity, the effects of the kidney disease, and global QOL in the questionnaires filled out by the parents (TECAVNERCP). No other studies have examined the influence of hypertension on QOL in children.
We observed no significant differences in relation to short stature, despite the fact that, according to the medical literature, this appears to be one of the factors that most heavily influences self-esteem and well-being in children with CKD.9 Our results are in accordance with those obtained by other authors studying the changes in QOL in children with idiopathic short stature treated with human growth hormone as compared to an untreated control group. In this study, whereas the paediatrician considered that QOL improved in the treated group, the patients’ parents did not observe this improvement, and children in the treated group felt the same or even worse than those in the control group. As such, the assumption that treatment with human growth hormone would improve the QOL in these children cannot be supported by this study.17 Another study examined the medical and social evolution of adolescents with kidney disease before the use of human growth hormone. The authors observed an important delay in growth, with 35.6% of these adolescents falling below the third percentile. Surprisingly, this study also found no correlation between short stature and functional state, defined as a state of social and economic independence, personal autonomy, and appropriate social and inter-personal relationships.18 However, in the study by Riaño, patients with short stature had a lower self-esteem and decreased satisfaction with their state of health, perhaps because these patients were all adolescents in which stature is an important psychological factor.9 Our sample also included small children, who perhaps had yet to give much importance to their physical appearance. Gerson, whose study also included patients 2 years of age and older,10 observed an association between short stature and worse COV in terms of physical, emotional, and social function and scholastic activity. As such, it appears that results vary based on the population studied, the type of questionnaire used (generic vs specific), and whether it is the opinion of the patient or the patient’s relatives that are taken into account.
As regards the presence of bone deformities, we observed differences only in the field of autonomy, both in the opinion of the patients and of their parents (P=.001 and P=.0029, respectively). This translates into increased physical dependence of patients with deformities upon their caretakers, making an early and effective treatment of altered bone and mineral metabolism an essential process in these patients.
Studies in adults19 have demonstrated that a greater number and duration of hospitalisations is correlated with deteriorated physical state, and although this relationship did not reach statistical significance in our study, we did observe a tendency for worse physical state in relation to increased number of hospitalisations.
In paediatric patients, it is important to evaluate whether a relationship exists between the number of hospitalisations and delay in academic development, socialisation, and emotional state, as well as the fields of learning and autonomy, as we believe that these factors could be strongly affected by prolonged and frequent hospitalisations.
However, we did not observe significant differences in the fields of scholastic development and learning in correlation with the number or duration of hospitalisations. As expected, there was a relationship with general state of health, which is worse in patients with more hospitalisations, as well as with the amount of time dedicated to health care. Gerson showed that school attendance is inferior in infirm patients, even in early phases of disease, as compared to healthy subjects, which is probably correlated with frequent hospital visits resulting in missed school days and cognitive alterations associated with kidney disease.
Doctors who treat patients with chronic diseases must be aware of the consequences of frequent and prolonged hospital stays, and should make an effort to require as few hospitalisations as possible and to minimise their duration so that children and their families may lead a life as normal as possible and that is compatible with daily activities. This can be achieved by reducing the number and frequency of doctor visits, adjusting them to the family’s schedule, and even attempting telephone consultations in lieu of in-person evaluations.
Of the different laboratory variables analysed, albumin and haematocrit most heavily influence QOL in adults, since these are related to nutritional state and physical capacity. It has been found that physical state is better in patients with haematocrit >35%.19 Patients also have improved functional capacity and well-being following treatment with erythropoietin, regardless of the renal replacement therapy provided, which reflects the increase in energy felt by these patients.20 In general, patients treated with erythropoietin report improved QOL.21-23 In our patients, we also observed improved physical activity and school attendance in the opinion of the children and their parents, and improved cognitive state and effects of kidney disease in the opinion of the children, when haematocrit was >35%. Both the opinions of the children and their parents are in accordance with correlations between physical activity and haematocrit observed in adults with kidney disease. The fact that school attendance also improved in patients with greater haematocrit levels may also be correlated with improved physical activity and the presence of fewer negative effects caused by the kidney disease, leading to an improved cognitive state in these children. The influence of anaemia on HRQOL has been examined by other authors, who demonstrated an inferior QOL as perceived by parents whose adolescent children suffered anaemia, regardless of the severity of kidney disease, with detrimental effects primarily in the field of physical function.24 Riaño9 and Eijseimans25 reported greater physical discomfort and worse physical function, respectively, in anaemic patients.
Along with haematocrit, serum albumin is one of the most important indicators of physical state in adults, which is probably due to the fact that albumin is a marker for malnutrition and inflammation.26,27 Patients with hypoalbuminemia generally report an inferior QOL.19 In our sample of patients, we did not observe a significant correlation between albumin and QOL. Our results are in accordance with those from Morton et al.28 involving 60 stable adult patients on PD using the MOS-SF-20 test, in which albumin appeared to be more closely related to nutrition and technique failure than as an indicator for well-being and QOL.
Altogether, of the factors analysed in our study, we find that regardless of the therapeutic modality, fluid restrictions, hypertension, and haematocrit heavily influence the QOL of children with CKD, and for the most part these can be improved through medical treatments, thus affecting QOL. One of the treatment factors that held the strongest influence on the QOL of our patients was fluid restriction (not diet restrictions), perhaps because in adolescents, this implies an inability to carry out normal social relationships, which is the aspect of QOL most highly valued at this age. As such, when choosing a therapeutic modality (HD vs PD), we must discuss the possible options and impacts with both parents and children, taking into account their opinions regarding social and extracurricular activities. Patients will have greater difficulties with fluid and diet restrictions on HD, which might lead to reduced compliance with treatment regimens and a greater frequency of medical complications. We must also pay special attention to hypertension, since in addition to the cardiovascular risks implied with this condition, it also affects the cognitive state of patients. Thus we must attempt to administer the fewest number of drugs possible and whenever feasible in a single daily dose, so as to ensure compliance with treatment and clinical improvements. As regards stature, it would be advisable to take into account patterns of stature in the patient’s family in addition to the possible effects of chronic renal failure, and the opinions of the parents, children, and paediatricians should all be valued. These opinions often differ but are still complementary, since the opinions of a 9-year old child will be different from those of an adolescent, and it is during these periods of development when information must be obtained from relatives and compared to the patient in question. We must take care to explain to the youngest of these patients that what may appear at the time to be acts of aggression (such as daily growth hormone injections) will provide major psychological and social benefits in the future in the form of an appropriate adult size.
If we make an effort to listen to and understand our patients, perhaps we will be able to improve their QOL as well as compliance with treatment regimens, which is one of the primary issues in caring for these patients. It is well known that non-compliance with treatment is a very important factor that contributes to graft loss, above all in adolescents, those with poor family support, low self-esteem, and psychological complexes. The use of multiple medical treatments, various schedules of administration, female sex, and a previous history of rejection are all important risk factors. Several studies have shown that a lack of adherence to treatment is associated with issues with autonomy and emotional states, such as the “right to be or feel normal” and personal health beliefs, which are often based on unconscious attempts to resolve emotional conflicts.29 If paediatric patients can develop sufficient trust and open communication with their doctor or nurse, facilitating ease of dialogue regarding treatments without fear or guilt about the difficulties of correct compliance with treatment regimens (medications and diet), this would greatly improve rates of compliance.
The objective of our study was to determine how we can improve our clinical activity in the fields of QOL that our patients felt were most heavily affected. While obtaining a Tx is clearly the option that most significantly improves QOL, our objective must be to attend to other important aspects, such as controlling hypertension and anaemia, avoiding bone deformations and short stature by strictly controlling mineral and bone metabolism starting at the onset of disease, optimising the number and/or duration of hospitalisations, and minimising the complexity of pharmacological treatments, seeking ways to provide single-dose drugs with synchronised schedules in order to facilitate compliance.
As such, we can conclude that the QOL of children with CKD is influenced by several laboratory parameters and treatment factors that can be modified with the intent to optimise QOL, with the goal of prolonging patient survival with the greatest possible QOL. We do wish to point out the limitations of this study in the form of a lack of a prior questionnaire specifically validated for these patients, for which we used the TECAVNER, which was created for this study with an appropriate Cronbach’s alpha coefficient. The small number of patients in each different modality of treatment is another limitation, due to the low prevalence of this disease and the wide geographic distribution. A multi-centre study could confirm our results and allow for children with CKD to benefit from the results obtained, and above all could lead to physicians paying greater attention to the opinions of paediatric patients.
Conflicts of interest
The authors state that they have no potential conflicts of interest related to the contents of this article.
Table 1. Sociodemographic variables
Table 2. Clinical situation
Table 3. Laboratory values
Table 4. Arterial hypertension, short stature, bone deformations, fluid restrictions, diet restrictions, and pharmacological treatment
Table 5. TECAVNER-TECAVNERCP results with statistical significance
Figure 1. Distribution of study patients (n=71) according to the number of hospitalisations in a six-month period
Figure 2. Distribution of patients hospitalised (n=25) according to the number of days of hospitalisation in a six-month period