Autosomal dominant polycystic kidney disease (ADPKD) accounts for 6–10% of patients on renal replacement therapy. The renal cysts gradually grow and replace the renal parenchyma, although kidney function remains normal until the third decade of life.1 The main factors involved in the progression glomerular filtration rate (GFR) deterioration are: type of mutation, kidney volume and hypertension (HTN).2PKD1 mutation, and particularly the truncating type, has a worse prognosis, as described in the PRO-PKD model.3 Increase in kidney volume measured by nuclear magnetic resonance (NMR) may be used to classify patients as rapid progressors if they belong to classes 1C, 1D and 1E of the Mayo Clinic model.4
HTN, which appears early, increases cardiovascular morbidity and mortality, which is the leading cause of death in these patients. The main determinant of HTN is activation of the renin–angiotensin system (RAS). The use of RAS inhibitors as antihypertensives also reduce proteinuria, thereby slowing the progression of chronic kidney disease (CKD). As demonstrated by the HALT study, the degree of HTN has an effect on the progression of CKD. Monitoring blood pressure is useful to maintain a control of blood pressure that should be stricter than in the general population (BP 95-110/60-75 mmHg in patients under 50 years of age).5,6
The aim of our study was to show whether number of antihypertensives, as a simple indicator of HTN severity, might also be a factor of CKD progression in adults with PKD.
One hundred and twenty-three patients with an ultrasound and/or genetic diagnosis of PKD followed in outpatients clinics of hereditary kidney diseases were analysed (until the 31st of May 2019). Patients with a GFR < 15 ml/min were excluded. The main clinical characteristics were: mean age 37.29 ± 15.04 years, 48.8% male, mean GFR 84.58 ± 41.22 ml/min, 56.1% were hypertensive, 26.8% taking more than one antihypertensive medication, 56.1% had genetic studies (40.7% PKD1 and 15.4% PKD2), 65% presented enlarged kidneys (renal length on ultrasound >13.5 cm), 39.8% had hepatic cysts, 26% had at least one episode of haematuria, cholesterol 167.22 ± 35.81 mg/dl and urate 5.34 ± 1.72 mg/dl. The distribution of antihypertensives by type was as follows: ACE inhibitors 50.72%, ARBs 47.83%, calcium channel blockers 40.58%, doxazosin 21.74%, beta-blockers 10.14% and diuretics 7.25%.
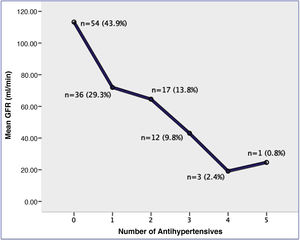
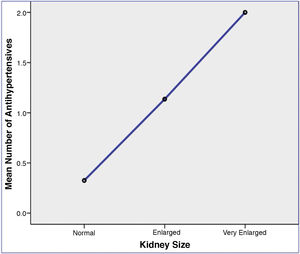
A lower GFR was observed in hypertensive patients (62.12 ± 36.06 vs. 113.28 ± 27.31, p = 0.000) and with notably a greater reduction in GFR the higher the number of antihypertensives (r = −0.642, p = 0.000), with (Fig. 1). Moreover, a statistically significant association was found between being HTN taking a greater number of antihypertensives and increased kidney volume; the hypertensive patients had large kidneys as compared with non-hypertensive patients (73.75% vs. 23.26%, p = 0.0001). Fig. 2 shows that the mean number of antihypertensives medications was significantly associated with an increase in kidney size: 0.33 ± 0.68 in normal kidneys (<13.5 cm), 1.14 ± 1.12 in enlarged kidneys (13.5–16.5 cm) and 2.0 ± 1.18 in very enlarged kidneys (>16.5 cm).
In PKD, it is essential to identify the factors that predict poor prognosis of CKD progression. In most centres, there is limited availability to perform genetic studies (they are performed only indicated in certain situations)2 and many patients do not have regular measurements of kidney volume increase with NMR (as is established in guidelines and the latest published studies).7 Nevertheless, HTN is an accessible factor that can be controlled to slow disease progression.8 With our experience, we have observed that a higher number of antihypertensives is another important factor of progression to take into account in the disease―one that is not recognised by the majority of published articles or predictive models.
To conclude, we are in agreement with other authors that HTN is a leading factor in GFR deterioration in PKD, but it should be highlighted that number of antihypertensives9 a simple indicator of HTN severity, is also a factor for poor prognosis. This parameter is useful and accessible, unlike others such as genetic study or NMR.
FundingThis study received no specific funding from public, private or non-profit organisations.
Conflicts of interestAll the authors of this article declare that they have no conflicts of interest.
Please cite this article as: Martínez Jiménez V, Hernández González AN, López Jiménez I, Rodríguez Peña L, Galbis Martínez L, Santa-Olalla González M, et al. La importancia del número de antihipertensivos en la progresión de la poliquistosis renal autosómica dominante. Nefrologia. 2021;41:362–364.