The number of elderly patients with advanced chronic kidney disease (ACKD) has increased in recent years, and the best therapeutic approach has not been determined due to a lack of evidence.
ObjectivesTo observe the progression of elderly patients with ACKD (stages 4 and 5) and to compare the survival of stage 5 CKD patients with and without dialysis treatment.
Material and methodsAll patients ≥70 years who began ACKD follow-up from 01/01/2007 to 31/12/2008 were included, and their progression was observed until 31/12/2013. Demographic data, the Charlson comorbidity index, history of ischaemic heart disease (IHD) and diabetes mellitus (DM) were assessed.
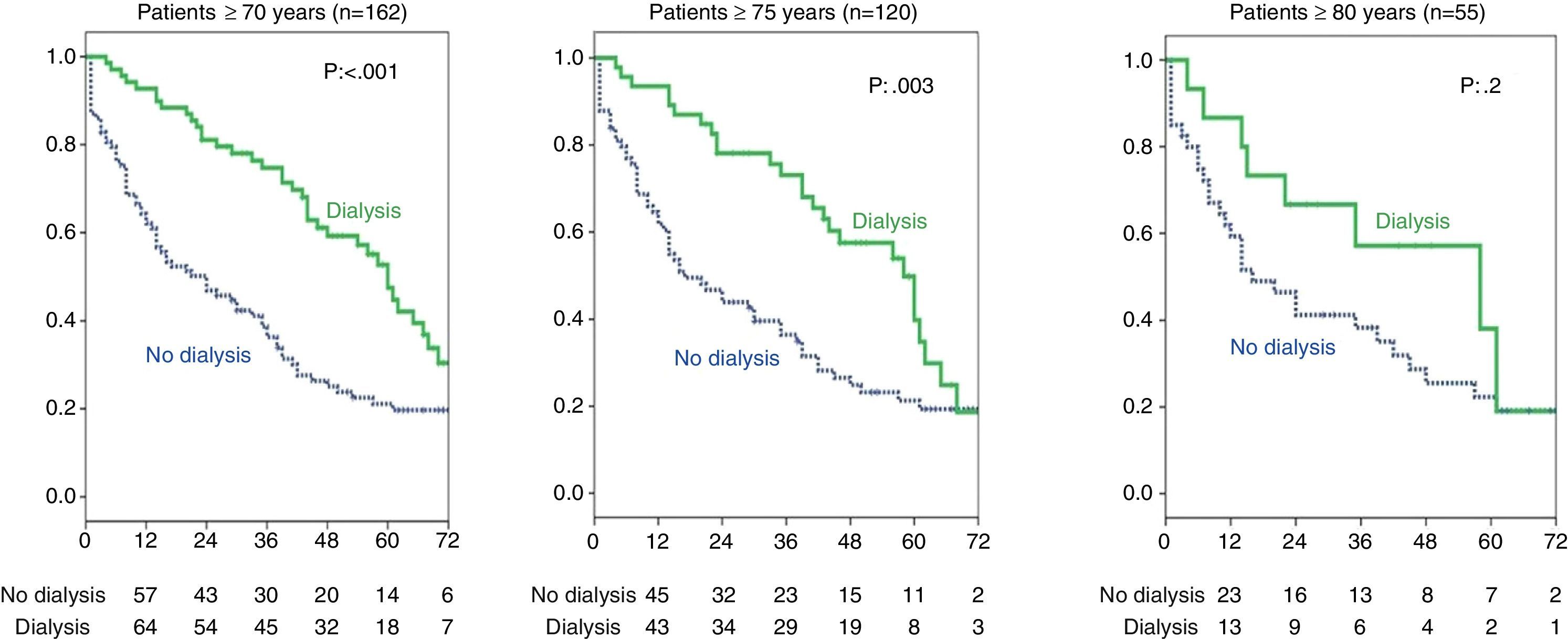
ResultsA total of 314 patients ≥70 years with stages 4 and 5 CKD were studied. Of these patients, 162 patients had stage 5 CKD at the beginning of follow-up or progressed to stage 5 during the study, and 69 of these patients were treated with dialysis. In the stage 5 group, median age was 77 years (74–81); 48% had IHD; 50% had DM, Charlson 7 (6–9). Kaplan–Meier survival analysis: ≥70 years (93 vs. 69 patients with dialysis, log rank: 15 p<0.001); patients ≥75 years (74 vs. 46 patients with dialysis, log rank: 8.9 p=0.003); patients ≥80 (40 vs. 15 patients with dialysis) and p=0.2. Patients receiving dialysis were younger, with a lower Charlson comorbidity index and shorter follow-up time.
ConclusionsOur study shows that dialysis treatment improves survival, although this benefit is lost in patients ≥80 years.
Los pacientes de edad avanzada que llegan a enfermedad renal crónica avanzada (ERCA) se han incrementado en los últimos años. No hay evidencia de la mejor actitud terapéutica en estos pacientes.
ObjetivosObservar la evolución de pacientes ancianos en consulta de ERCA (estadios 4 y 5) y comparar la supervivencia de los pacientes con ERC estadio 5 tratados con diálisis o no.
Material y métodosSe incluyó a todos los pacientes con ≥70 años que iniciaron seguimiento en consulta de ERCA desde el 1-1-2007 hasta el 31-12-2008 y se observó su evolución hasta el 31-12-2013. Se recogieron datos demográficos, índice de comorbilidad de Charlson, antecedentes de cardiopatía isquémica (CI) y diabetes mellitus (DM).
ResultadosSe estudió a 314 pacientes con ERC estadios 4 y 5 con ≥70 años, 162 de los cuales estaban en el momento del inicio del seguimiento o a lo largo del mismo en estadio 5; 69 de estos pacientes recibieron tratamiento con diálisis. En el grupo estadio 5: mediana de edad de 77 años (74-81); 48% CI; 50% DM; Charlson 7 (6-9). Supervivencia Kaplan-Meier: ≥70 años (93 vs. 69 pacientes con diálisis) log rank: 15 (p<0,001), con ≥75 años (74 vs. 46 pacientes con diálisis; log rank: 8,9; p=0,003), con ≥80 años (40 vs. 15 pacientes con diálisis) y p=0,2. Los pacientes que recibieron tratamiento con diálisis tenían menor edad e índice de Charlson y el tiempo de seguimiento en consulta era inferior.
ConclusionesEn nuestro estudio el tratamiento con diálisis mejora la supervivencia, si bien esta ventaja se pierde en los pacientes con ≥80 años.
The number of elderly patients with advanced chronic kidney disease (ACKD), estimated glomerular filtration rate (eGFR) under 30ml/min/1.73m2, stages 4 and 5 according to the DOQI classifications,1 has increased dramatically.2 In some series, it has doubled during the last 25 years.3 In our area, according to the 2013 data from the Kidney Transplant Coordination Data System of Andalusia (SICATA), a database of kidney patients treated with dialysis and transplantation in Andalusia, patients over 70 accounted for 38% of the incident patients and 41.4% of the prevalent patients in dialysis programmes.4 Among the ACKD consultations in our hospital in 2013, adults 70 or older accounted for 58% of incident patients and up to 66% of the prevalent patients. Longer life expectancies and medical advances have contributed to the increased period of time for the development of renal atherosclerosis and diabetes mellitus (DM). During the past years, these patients died before reaching an advanced stage of CKD.5 It is currently unclear whether in this group of patients renal replacement therapy (RRT) is the best option as compared with conservative treatment, since a large proportion of them present an increased fragility, with high indices of dependence and higher comorbidity, including DM, atherosclerosis in several locations, heart disease, with or without heart failure, difficult vascular access, etc. Therefore RRT may not improve their survival11–13 much less their quality of life. In this regard, it should be taken into account how a specific patient is affected by the change in lifestyle from the dialysis technique itself (exchanges in peritoneal dialysis, travel to dialysis centres, following schedules, dependence on other caretakers or family members, etc.) and its complications (decreased function after sessions, high rate of hospitalisations, use of venous catheters and their complications, etc.).14,15
Currently, there is a growing interest in evaluating the possibility of a more conservative treatment for elderly ACKD patients.7 It must be specified that conservative treatment in this patient group should not entail an “absence of treatment” or less specialised medical care.8–10 Conservative treatment implies patient care in ACKD clinics with multidisciplinary approach to provide the best quality of life possible to end-stage kidney disease patients not eligible for dialysis therapy.
Our objectives in this study were to discover the long-term progression of elderly incident ACKD (stages 4 and 5) patients in our out patient clinics and to retrospectively compare survival in the group of CKD stage 5 patients who underwent dialysis with those who followed a conservative treatment.
MethodsRetrospective, observational study including all patients 70 or older who began follow-up in the ACKD clinic of the Nephrology Department of the Hospital Universitario Virgen del Rocío in Seville (hospital area includes 1,400,000 habitants) from January 1, 2007 through December 31, 2008 and whose progress was observed for a 5-year period; the end of observational period was December 31, 2013. The database from our own office was used to identify patients and collect follow-up information. The DAE system (electronic data platform) used by the public health system of Andalusia was also employed to support the electronic medical records along with the SICATA registry.
Kidney function at the first visit to the ACKD clinic was computed as baseline estimated GFR using the MDRD-4 equation. Renal function was also computed when patients entered stage 5 (eGFR<15ml/min/1.73m2), in the case that the patient reached this stage during the follow-up period. The following data were extracted from their medical records: cause of kidney disease, vascular access in the case of patients who started haemodialysis, history of DM, ischaemic heart disease (understood as an ischaemic episode), Charlson comorbidity index calculation, follow-up period in the clinic before they left, and their reason for leaving (death, dialysis, or end of the observation period on December 31, 2013). For patients who died, the date and cause were recorded when it occurred in our hospital or at home after a previously known disease process. We were not able to determine the cause of death if patient died in another hospital.
A descriptive analysis was conducted on the different quantitative variables using the median and the 25th and 75th percentiles, since they did not show a normal distribution; qualitative variables were expressed as the number and percentages. The Mann–Whitney U test and chi-squared test were used to analyse the difference between patients with <15ml/min/1.73m2 who received dialysis and those who did not, and between the patients who died and those alive at the end of the follow-up. The analysis was performed in both the entire group (314 patients) and in stage 5 patients (162 patients). The Kaplan–Meier and log-rank methods were used to estimate and compare survival in both groups. The Cox proportional hazards regression was used to investigate the impact of dialysis and other independent variables on survival. First, the correlation between each variable (age, eGFR, history of DM, history of ischaemic heart disease, Charlson index, and dialysis treatment) and survival (dependent variable) was independently analysed in a bivariate regression analysis. Then, the variables that were significant and those considered to have specific clinical significance were included in the Cox regression analysis. The IBM SPSS-19 statistical package was used.
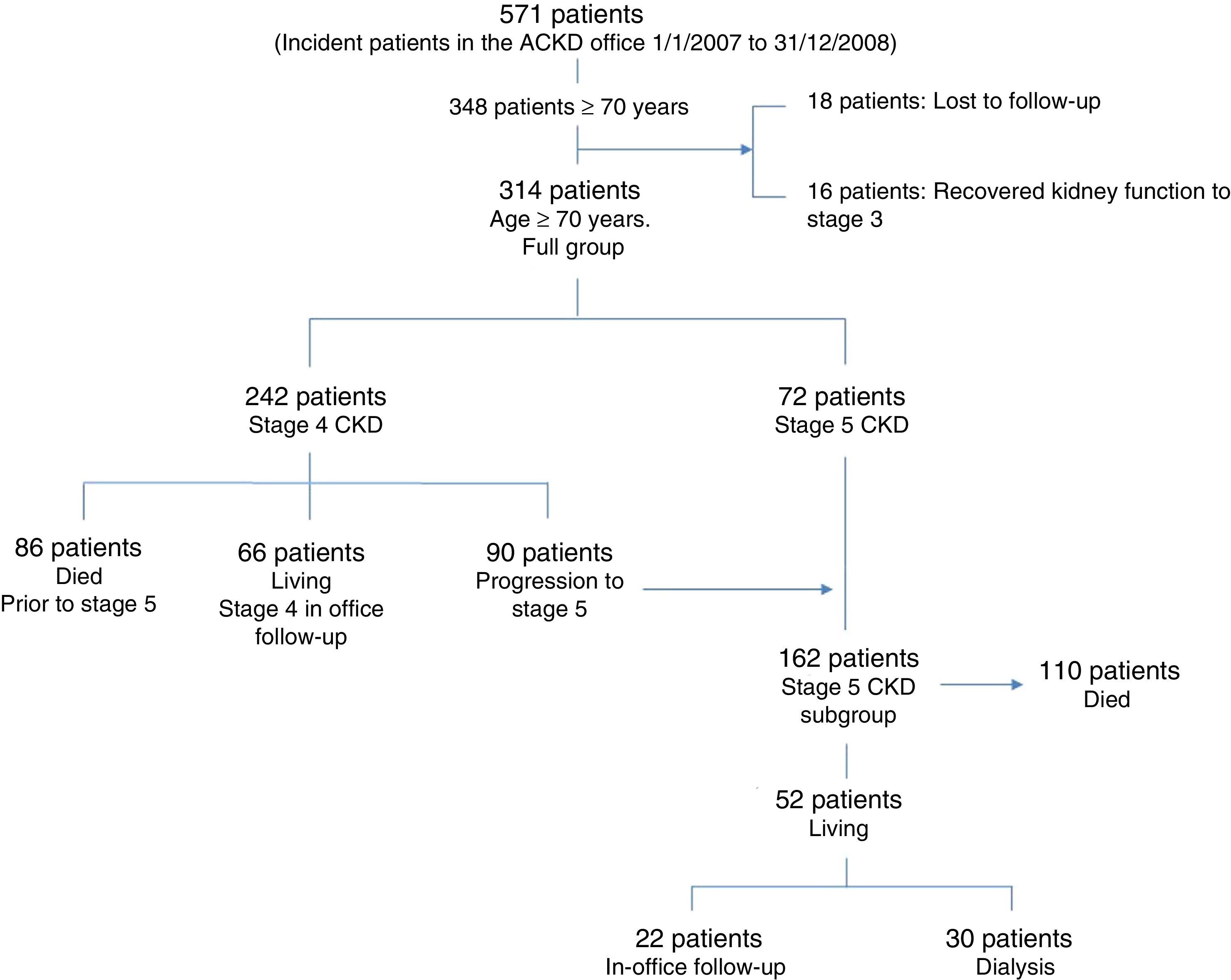
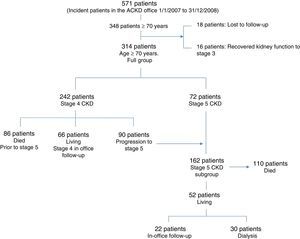
ResultsInitially 348 patients were studied who were 70 or older seen for the first time in the ACKD office successively during the specified follow-up period. During the follow-up, 16 patients recovered kidney function and went/returned to the General Nephrology clinic. Similarly, 18 patients were lost to follow-up. These 348 patients accounted for 61% of all 571 patients of all ages seen for the first time during the inclusion period. The final sample was made up of 314 patients; of these, 242 began their follow-up in stage 4 CKD and 90 (37%) progressed to stage 5. At the time of their first visit (in the case of 72 patients) or during the follow-up (in the case of the 90 patients mentioned above) 162 patients reached stage 5 (eGFR<15ml/min/1.73m2). Fig. 1 displays this information schematically.
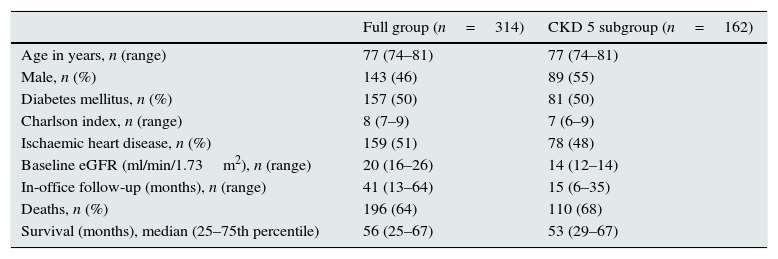
None of the patients was discarded, despite the fact that in some cases their eGFR was greater than 30ml/min/1.73m2 as there was a slight transitory improvement. In the case where this improvement lasted, they were sent back to the General Nephrology clinic. The demographic data and other characteristics for both the full group (314 patients) and the subgroup of patients with stage 5 CKD (162) are shown in Table 1. Table 2 shows the survival in the 2 groups by year of follow-up and the overall survival from the first visit (baseline) until the end of the follow-up period or death. As for the 90 patients who started with an eGFR in stage 4 and progressed to stage 5, survival was considered since the time the eGFR was under 15cc/m/1.73m2.
Demographic data.
| Full group (n=314) | CKD 5 subgroup (n=162) | |
|---|---|---|
| Age in years, n (range) | 77 (74–81) | 77 (74–81) |
| Male, n (%) | 143 (46) | 89 (55) |
| Diabetes mellitus, n (%) | 157 (50) | 81 (50) |
| Charlson index, n (range) | 8 (7–9) | 7 (6–9) |
| Ischaemic heart disease, n (%) | 159 (51) | 78 (48) |
| Baseline eGFR (ml/min/1.73m2), n (range) | 20 (16–26) | 14 (12–14) |
| In-office follow-up (months), n (range) | 41 (13–64) | 15 (6–35) |
| Deaths, n (%) | 196 (64) | 110 (68) |
| Survival (months), median (25–75th percentile) | 56 (25–67) | 53 (29–67) |
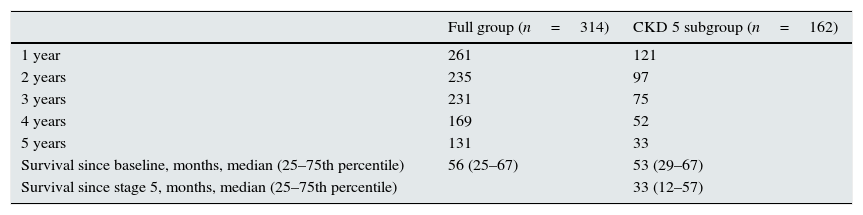
Survival by year of follow-up and total.
| Full group (n=314) | CKD 5 subgroup (n=162) | |
|---|---|---|
| 1 year | 261 | 121 |
| 2 years | 235 | 97 |
| 3 years | 231 | 75 |
| 4 years | 169 | 52 |
| 5 years | 131 | 33 |
| Survival since baseline, months, median (25–75th percentile) | 56 (25–67) | 53 (29–67) |
| Survival since stage 5, months, median (25–75th percentile) | 33 (12–57) |
In the group of 69 patients who underwent dialysis (87% haemodialysis, 13% peritoneal dialysis), 35 patients (51%) had a vascular access, 18 patients (26%, in 10 cases vascular access was requested) started with a transitory venous catheter, type of access was unknown in 7 patients (10%), and 9 patients had a peritoneal catheter (13%). The median time in dialysis was 27 months (9–51) for the entire group of ≥70 y.o., 30 months (14–46) for the 46 patients ≥75 y.o., and 14 months (2–39) for the 15 patients ≥80 y.o. For the subgroup of 54 patients 70–80 y.o., the median time in dialysis was 30 months (10–52). None of the patients received a transplant.
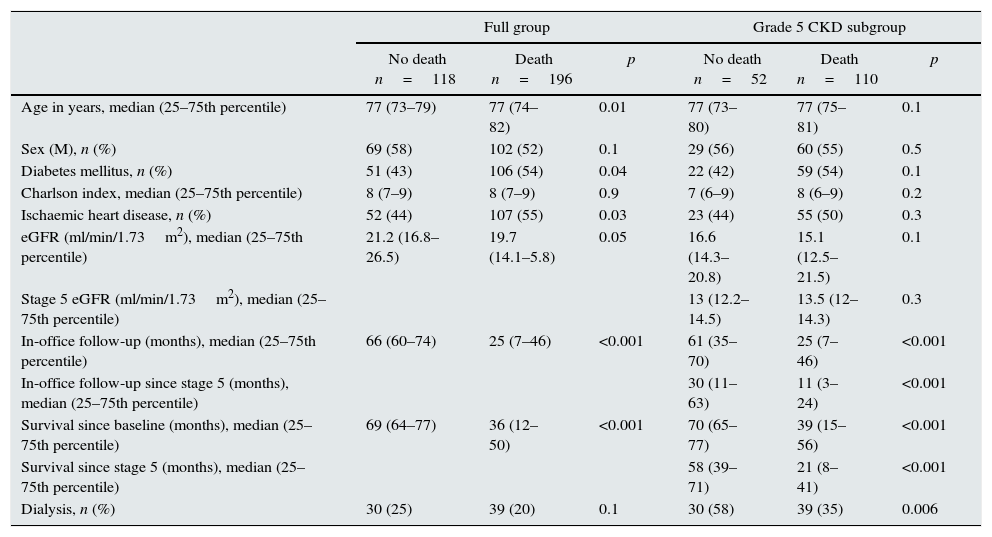
Comparison of deaths vs. surviving patients (full group and stage 5 subgroup)The difference between patients who died and alive was analysed; Table 3 displays the results in both the full group and in the subgroup with stage 5 CKD. The most frequent causes of death in the full group (196 deaths) were: cardiovascular disease in 137 patients (70%) and cancer in 24 patients (12%). Data regarding the cause of death was not available in 15 patients (8%).
Death vs. no death.
| Full group | Grade 5 CKD subgroup | |||||
|---|---|---|---|---|---|---|
| No death n=118 | Death n=196 | p | No death n=52 | Death n=110 | p | |
| Age in years, median (25–75th percentile) | 77 (73–79) | 77 (74–82) | 0.01 | 77 (73–80) | 77 (75–81) | 0.1 |
| Sex (M), n (%) | 69 (58) | 102 (52) | 0.1 | 29 (56) | 60 (55) | 0.5 |
| Diabetes mellitus, n (%) | 51 (43) | 106 (54) | 0.04 | 22 (42) | 59 (54) | 0.1 |
| Charlson index, median (25–75th percentile) | 8 (7–9) | 8 (7–9) | 0.9 | 7 (6–9) | 8 (6–9) | 0.2 |
| Ischaemic heart disease, n (%) | 52 (44) | 107 (55) | 0.03 | 23 (44) | 55 (50) | 0.3 |
| eGFR (ml/min/1.73m2), median (25–75th percentile) | 21.2 (16.8–26.5) | 19.7 (14.1–5.8) | 0.05 | 16.6 (14.3–20.8) | 15.1 (12.5–21.5) | 0.1 |
| Stage 5 eGFR (ml/min/1.73m2), median (25–75th percentile) | 13 (12.2–14.5) | 13.5 (12–14.3) | 0.3 | |||
| In-office follow-up (months), median (25–75th percentile) | 66 (60–74) | 25 (7–46) | <0.001 | 61 (35–70) | 25 (7–46) | <0.001 |
| In-office follow-up since stage 5 (months), median (25–75th percentile) | 30 (11–63) | 11 (3–24) | <0.001 | |||
| Survival since baseline (months), median (25–75th percentile) | 69 (64–77) | 36 (12–50) | <0.001 | 70 (65–77) | 39 (15–56) | <0.001 |
| Survival since stage 5 (months), median (25–75th percentile) | 58 (39–71) | 21 (8–41) | <0.001 | |||
| Dialysis, n (%) | 30 (25) | 39 (20) | 0.1 | 30 (58) | 39 (35) | 0.006 |
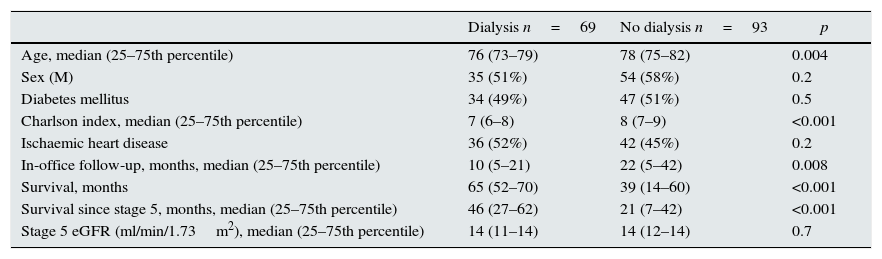
Table 4 shows the demographic data for the group comparing those who received dialysis and those who did not.
Dialysis vs. no dialysis stage 5 CKD subgroup (n=162).
| Dialysis n=69 | No dialysis n=93 | p | |
|---|---|---|---|
| Age, median (25–75th percentile) | 76 (73–79) | 78 (75–82) | 0.004 |
| Sex (M) | 35 (51%) | 54 (58%) | 0.2 |
| Diabetes mellitus | 34 (49%) | 47 (51%) | 0.5 |
| Charlson index, median (25–75th percentile) | 7 (6–8) | 8 (7–9) | <0.001 |
| Ischaemic heart disease | 36 (52%) | 42 (45%) | 0.2 |
| In-office follow-up, months, median (25–75th percentile) | 10 (5–21) | 22 (5–42) | 0.008 |
| Survival, months | 65 (52–70) | 39 (14–60) | <0.001 |
| Survival since stage 5, months, median (25–75th percentile) | 46 (27–62) | 21 (7–42) | <0.001 |
| Stage 5 eGFR (ml/min/1.73m2), median (25–75th percentile) | 14 (11–14) | 14 (12–14) | 0.7 |
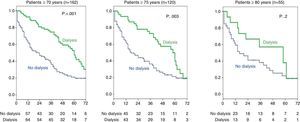
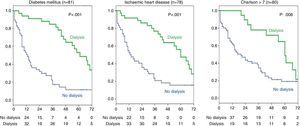
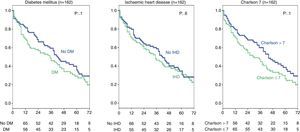
The Kaplan–Meier analysis confirmed that the survival was better in patients that were dialyzed: 69 vs. 93 patients in conservative treatment aged 70 or older (log-rank: 15.4; p<0.001). An additional sub-analysis was performed in 120 patients aged 75 or older (median 77; 25–75th percentile: 74–81 years) (46 vs. 74 patients without dialysis), survival being higher in patients receiving dialysis (log-rank: 8.9; p=0.003). Similarly, the group of 55 patients aged 80 or over was analysed (median 82; 25–75th percentile: 81–84 years, 15 vs. 40 without dialysis); in this group patients receiving dialysis did not show statistical increase in survival as compared with conservative treatment (log-rank: 1.6; p=0.2). Fig. 2 shows the survival curves for the 3 patient groups by age.
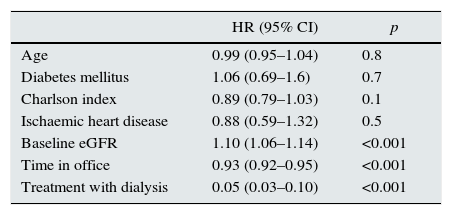
Cox regression (subgroup of 162 stage 5 patients)To determine which variables influence survival in this group over time, a Cox regression analysis was completed, using survival time as the dependent variable. Among the variables initially assessed independently using bivariate regression, we found the following results: follow-up time in the office (HR: 0.95; p<0.001), baseline eGFR (MDRD-4) (HR: 0.96; p=0.001), age (HR: 1.04; p=0.008), dialysis (HR: 1.68; p=0.01). There was no statistically significant correlation with sex, comorbidity as measured by the Charlson index, history of diabetes, or history of ischaemic heart disease.
The statistically significant variables in the bivariate regression with survival and the non-significant variables that have clinical relevance (ischaemic heart disease and DM) were included to determine the effect that each one has in the Cox regression model: age, kidney function as measured by the MDRD-4 eGFR, dialysis, and time in the office. History of ischaemic heart disease, history of DM, and age were not statistically significant in the multivariate analysis. The resulting hazard ratios indicate that, in our study, dialysis, follow-up time in the office, and baseline kidney function were the most important variables for survival in our group of patients (Table 5).
Cox regression: variables influencing survival over time.
| HR (95% CI) | p | |
|---|---|---|
| Age | 0.99 (0.95–1.04) | 0.8 |
| Diabetes mellitus | 1.06 (0.69–1.6) | 0.7 |
| Charlson index | 0.89 (0.79–1.03) | 0.1 |
| Ischaemic heart disease | 0.88 (0.59–1.32) | 0.5 |
| Baseline eGFR | 1.10 (1.06–1.14) | <0.001 |
| Time in office | 0.93 (0.92–0.95) | <0.001 |
| Treatment with dialysis | 0.05 (0.03–0.10) | <0.001 |
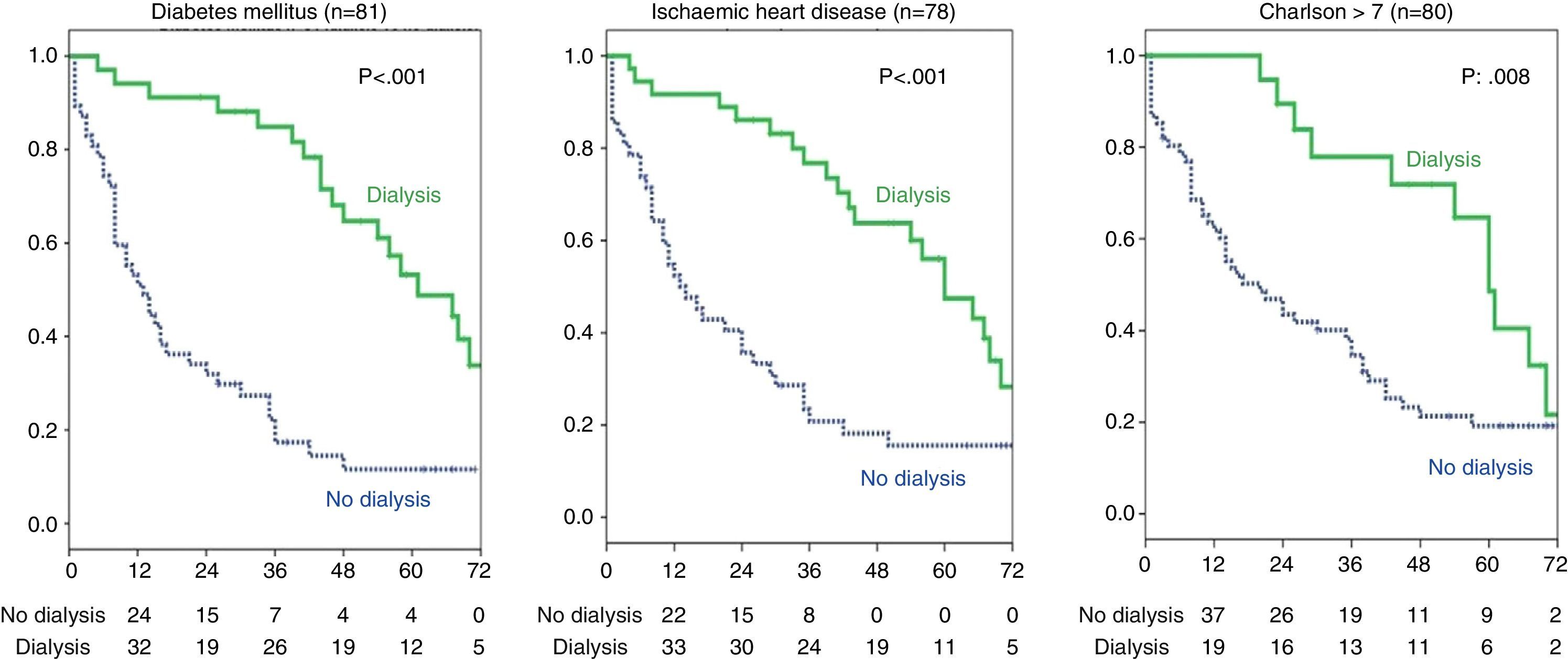
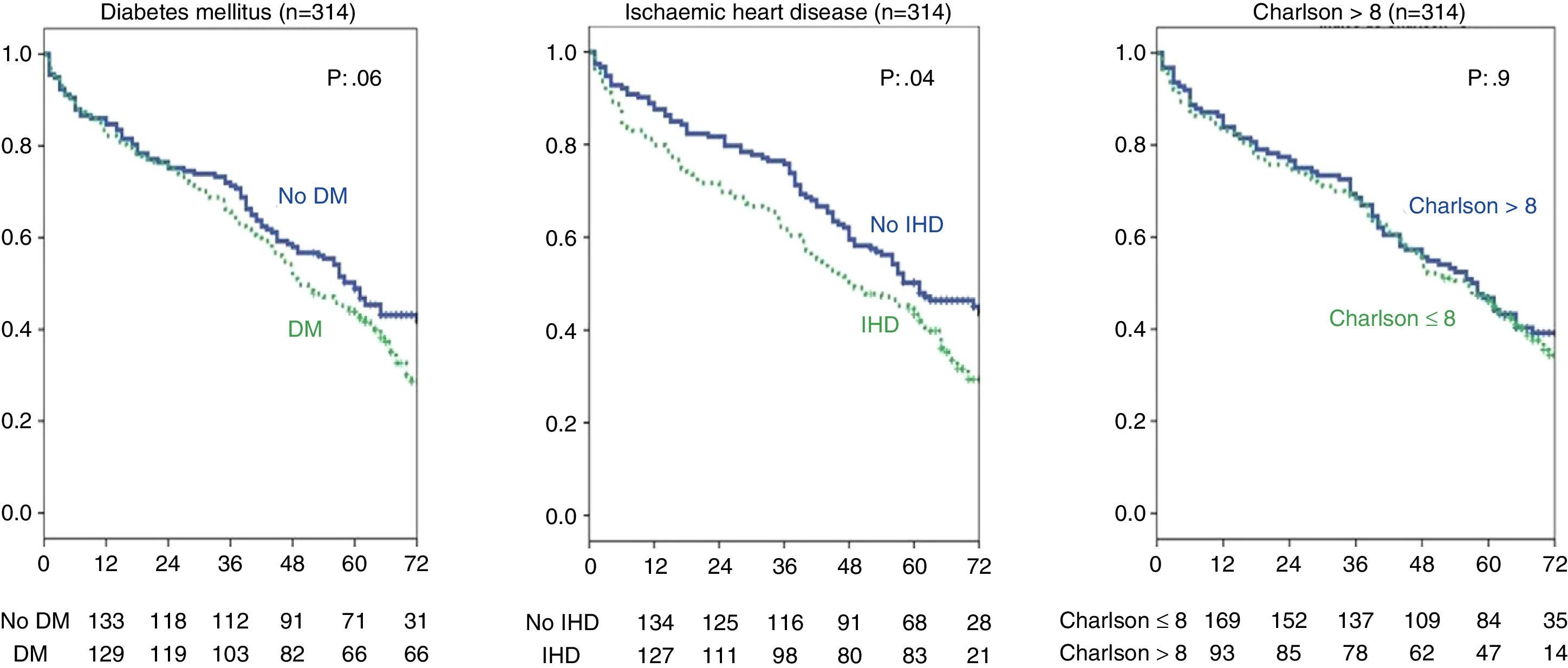
An additional survival analysis was performed (Fig. 3) among the group of stage 5 patients with ischaemic heart disease (n=78) to determine whether dialysis still had a favourable effect on survival in this subgroup of patients. The results showed that dialysis did favour survival (36 dialysis vs. 42 without dialysis; log-rank 14.7; p<0.001). Similarly, the effect of dialysis in the group of patients with DM (n=81) was analysed, demonstrating that patients treated with dialysis had a better survival (34 vs. 47 patients without dialysis; log-rank 26; p<0.001). Among the patients (n=80) with a high Charlson index (over 7, the group median), the difference in survival with dialysis was also significant (log-rank 6.9; p=0.008).
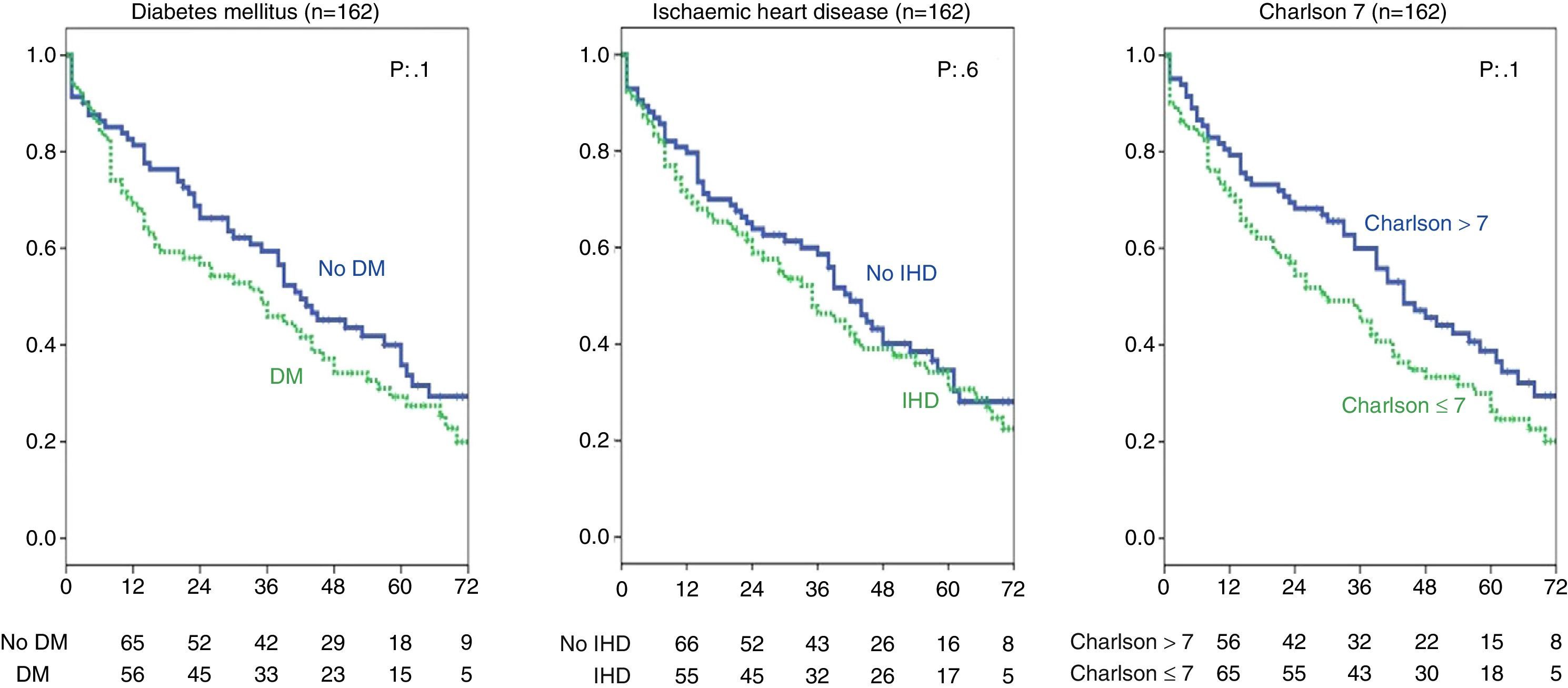
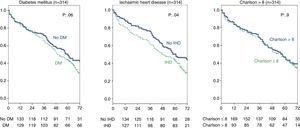
The effect of a history of DM or ischaemic heart disease and a high Charlson index in stage 5 CKD patients was also analysed and no significant differences were found (Fig. 4). In the entire group (314 patients) this analysis showed that ischaemic heart disease did affect survival (as seen with the Chi-squared test, Table 2) log-rank 4.2; p=0.04. As for DM, the difference is close to statistical significance (log-rank 3.3; p=0.06), and there were no differences in survival for a Charlson index over 8 (group median) (Fig. 5).
The results from our study in patients with advance age (≥70 years) with stage 5 CKD show that survival was higher in those treated with dialysis than in a conservative treatment; however this advantage is lost in patients ≥80 years. In addition to dialysis, survival in stage 5 patients was improved inpatients with a long time of follow up in the outpatient clinic and was not changed in relation to a higher comorbidity as measured by the Charlson index and a history of DM or ischaemic heart disease. Considering all patients (314 patients, stages 4 and 5), survival was lower in patients with a history of DM and ischaemic heart disease.
For ethical and technical reasons randomised studies are not possible in this field; several studies, all observational, mostly conducted in the United Kingdom, have observed the clinical outcome of elderly patients included in dialysis programmes, and a few reports have compared clinical outcome in elderly on dialysis vs. conservative treatment. In general, it was shown that patients have better survival on dialysis, although this advantage is lost in patients with medical history of ischaemic heart disease.11 Comorbidity as measured by the Charlson index16 or in patients with several mortality risk factors considered six months after starting dialysis.17 Similarly, longer survival may not be significant if hospitalisation days or those dedicated to dialysis sessions are subtracted, as shown in the work by Da Silva-Gane.16 The 404-day difference in survival in patients treated with dialysis is to some extent lost if the 326 days allocated to haemodialysis sessions are subtracted. The case of peritoneal dialysis has different interpretation, since patients do not need to travel.
The results from this study are very similar to those previously published. In the study by Hussain,18 with a group of patients very similar to ours in which survival in patients over 70 years with eGFR of 15ml/min/1.73m2 was compared to patients treated conservatively vs. those treated with dialysis, overall survival was improved, although, like in our study, it was lost in those patients older than 80 years and in patients with higher comorbidity, as measured by the Charlson index, among others. The study by Murtagh,11 like ours, also observed that survival was longer in patients treated with dialysis, especially in patients referred early to ACKD outpatient clinics with a higher eGFR. It is unclear if this advantage in survival comes from the dialysis itself or from correctly screening and care of patients in those visits. However, this benefit was substantially lost in those cases that presented higher comorbidity indices, particularly with the presence of ischaemic heart disease. Conversely, in our study we did not find any differences relating to comorbidity in the stage 5 CKD group (we did observe a difference in our full group of 314 patients in stages 4 and 5), and in patients with DM and ischaemic heart disease the positive effect of dialysis on survival was still present. One explanation may be the lower number of patients, which lowers the statistical power; also many patients have both DM and ischaemic heart disease. So the sample of patients is homogeneous. There was also no difference in the prevalence of DM and ischaemic heart disease among those who received dialysis and those who did not, but there was a difference in being younger and in the Charlson index of the patients treated with dialysis, which implies that the patients were screened and those who were younger and had a lower comorbidity were included in dialysis which favoured survival in addition to the treatment. This is in line with previous studies which warned about the importance of personalising the treatment (dialysis vs. conservative) in each elderly patients based on their comorbidity.6–10,14–16
In our study patients (the full group with stages 4 and 5 CKD as well as in the stage 5 CKD group) that visited our outpatient clinics for long period of time have better survival in both the individual analysis as well as after adjusting for the different variables in the multivariate analysis. Our results are similar to other previously published results, such as the paper by De Nicola,19 in which patients seen for ACKD were followed for one year. They concluded that patients seen for a longer time had a lower risk of mortality. Previous follow-up in ACKD offices is an important factor in preparing these patients to choose the dialysis modality according to each patient's situation which may condition the short- and mid-term prognosis in RRT.20–22 A short period of visits to the office correlated with serious non-CKD-related comorbid processes that caused the early death, unrelated to follow-up in the office.
Another noteworthy point is the slow deterioration in kidney function in our patients despite significant deterioration at baseline, with a median eGFR near 20ml/min/1.73m2 (after 5 years of follow-up: 27% did not reach stage 5; 35% died before progressing to stage 5; 37% progressed to stage 5). This evolution has been previously described and it may be justified in part or in many cases by the absence of albuminuria, more common in patients with concomitant low filtration rate and albuminuria.23,24 In any case, current knowledge does not enable us to identify patients with ACKD who will progress and those who will not. In our study, the possibility of dying was similar to that of progressing to stage 5 in patients who started follow-up in stage 4. In other studies, the risk of dying was higher than progressing to end-stage CKD.25,26 It is possible that, had we considered a lower eGFR in our study, such as 8–10ml/min/1.73m2 instead of 15ml/min/1.73m2, the probability of dying would have been clearly higher than that of progressing and considering treatment with dialysis.
The limitations of the present study include the unavailability of additional data that could potentially condition mortality or survival, such as family support, autonomy, quality of life data after starting RRT or conservative treatment. The scarce number of patients in the older subgroups treated with dialysis must also be pointed out. This study was performed in a single centre, and findings might not apply fully to other patient groups. Missing from our study is information on patients who did not receive dialysis, whether they had abandoned the treatment, refused it, or had a medical contraindication. The results, which show higher ages and Charlson index in patients who received dialysis, make this last option more likely, since the patients were clearly screened.
The study was conducted in a single centre, so it has the advantage of being a homogeneous population of patients and that the treatment applied was uniform in all patients according to our current CKD patient handling guidelines. The inclusion period was short, and this favoured a similar treatment for all patients with similar criteria and same drugs available. It is also important that the follow-up time was long, more than 5 years.
Patients of other studies were compared based on the intention to treat or the initial decision on either RRT or conservative treatment. Our study compares outcomes of treatment followed by the patient, which reflects reality and increases its usefulness of our data that can be used as a tool for counselling patients. Patients ask about specific outcomes, so they can decide on modality of treatment: Dialysis or conservative treatment. Treatment with dialysis in many cases involves a worsening of quality of life, and according to our study in some cases did not even extend survival as compared with those who followed a conservative treatment; therefore treatment must always be personalised. Innovative strategies such as home care for elderly ACKD patients who accept or choose conservative treatment for kidney failure in its most advanced phase may improve the quality of life of the patients and their family, as it has been doing in some hospitals in our country.27
In conclusion, in our group of elderly patients (≥70 years), we have observed that dialysis treatment improves survival in screened patients, with lower ages and comorbidity indices. This result was favoured by extended follow-up periods in the ACKD office.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Martínez Echevers Y, Toapanta Gaibor NG, Nava Pérez N, Barbosa Martin F, Montes Delgado R, Guerrero Riscos MÁ. Supervivencia de pacientes de edad avanzada (≥70 años) con enfermedad crónica estadios 4-5: diálisis vs tratamiento conservador. Nefrología. 2016;36:283–291.