To compare the predictive capacity of self-reported somatic symptoms and mood (depression and anxiety) on health-related quality of life (HRQoL) in patients with chronic renal disease.
MethodData were obtained from 52 patients undergoing haemodialysis. Measures included (a) the SF-36 health survey, (b) the somatic symptoms scale revised (ESS-R) and (c) the hospital anxiety and depression scale (HADS). Multiple regression was the main method of statistical analysis.
ResultsPatients exhibited HRQoL levels below normative values, with anxiety and depression prevalence at 36.5% and 27%, respectively. Mood was the strongest predictor of physical (β=−.624) and mental (β=−.709) HRQoL. Somatic symptoms were also associated with physical HRQoL, but their predictive value was weaker (β=−.270).
ConclusionsThese results indicate that mood is a superior predictor of the physical and mental components of HRQoL in patients compared with the number and severity of physical symptoms. The data underline the importance of assessing negative emotional states (depression and anxiety) in kidney patients as a basis for intervention, which may facilitate reduction of the impact of chronic renal disease on HRQoL.
Comparar la capacidad predictiva de los síntomas somáticos informados y el estado anímico (depresión y ansiedad) sobre la calidad de vida relacionada con la salud (CVRS) en pacientes con enfermedad renal crónica.
MétodoSe evaluó a 52 pacientes en tratamiento de hemodiálisis mediante: a) la escala de funcionamiento y calidad de vida (SF-36), b) la escala de síntomas somáticos-revisada (ESS-R) y c) la escala de ansiedad y depresión en hospital (HAD). Los datos fueron analizados mediante análisis de regresión múltiple.
ResultadosLos pacientes mostraron niveles de CVRS inferiores a los valores normativos del instrumento, así como un 36,5% de prevalencia de ansiedad y un 27% de depresión. El estado anímico fue el predictor más significativo de la CVRS, tanto en su componente físico (β=−0,624) como mental (β=−0,709). Los síntomas somáticos predijeron, con menor fuerza asociativa, el componente de salud física (β=−0,270).
ConclusionesEl estado anímico es un mejor predictor de los componentes físico y mental de la CVRS que el número e intensidad de los síntomas físicos informados por los pacientes. Estos resultados señalan la importancia de evaluar e intervenir sobre los estados emocionales negativos (depresión y ansiedad) en los pacientes renales. Estas intervenciones pueden repercutir en una menor interferencia de la enfermedad sobre la CVRS en el paciente en hemodiálisis.
Health-related quality of life (HRQoL) has been defined as the evaluation made by the individual regarding his or her health and level of functioning in going about day-to-day activities, including physical, psychological and social function; general perception of health; mobility; and emotional well-being.1,2 HRQoL has become an essential concept for comprehensive care of the patient with a chronic disease.2,3 It is a useful variable for predicting potential adverse consequences in the course of the disease and for evaluating treatment efficacy.4 The HRQoL measurement is being used to evaluate the repercussions and impact that the disease causes in patients’ day-to-day life. It provides additional information of major importance to the simple diagnosis of the disease.5
Several studies have evaluated HRQoL in chronic kidney disease (CKD) and in patients on haemodialysis (HD) treatment.1,2,6,7 These works have shown that CKD and HD treatment interfere with the patient's life, and that HRQoL decreases if this is not borne in mind and addressed.2,8 The kidney patient has a lower HRQoL than that found in the general population,9,10 and this deterioration in HRQoL has been associated with clinical variables,11,12 sociodemographic variables,2,13,14 dialysis characteristics,14 physical symptoms, social support and disease impact.4 In addition, these studies have shown a close relationship between HRQoL indicators and morbidity/mortality indices.7,15
Some previous works have focused on the importance of physical deterioration in the determination of HRQoL.2,4,6,10,16 The kidney patient's physical problems modulate the assessments made by the patient of his or her adaptive capacity and condition as a sick person. The most common symptoms reported by kidney patients are musculoskeletal, gastrointestinal, immunological, cardiovascular and skin/allergy-related.17 These symptoms could be accounted for in part by the long-term effect of anaemia, malnutrition, cardiovascular complications typical in the kidney patient and complications or insufficient doses of dialysis.18 However, many properly dialysed patients, with good haematocrit levels and good clinical chemistry management, continue to have “widespread” physical discomfort that affects their well-being, for which no clear aetiology is found,14 and which does not respond appropriately to the treatments prescribed.19 One possible explanation for these symptoms and this “widespread” discomfort could lie in psychological and emotional considerations. For example, level of anxiety is an independent predictor of the report of somatic symptoms. This accounts for the 25% variance in total symptoms reported.17 Other variables associated with the report of somatic symptoms in the kidney patient in dialysis treatment are depression, degree of concern and passive strategies for coping with stress (fatalism and helplessness/hopelessness), while level of self-efficacy, social support and active coping strategies (such as a fighting spirit) are associated with lower reports of physical symptoms.17
Several works have assigned major importance to emotional disturbances in the determination of the HRQoL of the kidney patient.10–12,20–23 These emotional disturbances may be caused by the numerous losses the kidney patient has to face (loss of renal function, loss of well-being, loss of place in the family and at work, loss of financial resources and loss of sexual function), the continuous uncertainty that he or she experiences (regarding survival, dependence on medical technology, etc.), the stress inherent to dialysis sessions, serious dietary restrictions, etc.
Depression is one of the factors that negatively affect HRQoL20–25 in the kidney patient. Some studies have found that depression is the main predictor of HRQoL21: it is negatively associated with all its components and accounts for percentages of variance of around 50% for physical function, physical role, vitality, social function and mental health.10 Less importantly, degree of concern regarding the disease, as well as passive strategies for coping with stress, are also associated with lower HRQoL levels.10 By contrast, self-efficacy, optimism, social support and a fighting spirit are related to greater HRQoL levels.10 The UK National Institute for Health and Care Excellence has explicitly recognised the importance of depression in kidney disease.26 Depression tends to be more refractory to treatment when it occurs in the context of another medical disease.27,28 Thus, depression has a greater prevalence and is more resistant to treatment in the kidney patient in dialysis than in the general population.29
Based on the previous review, the 2 factors that seem to most affect the HRQoL of the kidney patient in HD treatment are somatic symptoms and mood (depression and anxiety). However, we have not found any studies that have analysed the combined and interactive influence of these 2 factors on the HRQoL of the kidney patient. In this context, the objective of this study was to compare the relative predictive capacity of somatic symptoms reported by the patient and his or her mood (depression and anxiety) with respect to HRQoL in patients with CKD in HD treatment, distinguishing between the HRQoL subcomponents of physical health and mental health. The potential interaction between somatic symptoms and mood in the determination of HRQoL was also analysed.
MethodParticipantsThe sample included 52 patients in chronic HD (38 men and 14 women). The type of dialysis received was on-line, 3 sessions per week, 4h each (plus one extra session to remove the overweight of patients who had gained weight relative to the previous session). Table 1 shows sociodemographic and clinical characteristics of patients included. The inclusion criteria were: 60 years old or younger, in treatment with dialysis for more than 6 months, not having suffered from serious clinical situations in the last 6 months (prolonged hospital stays or recent vascular access obstruction) and not suffering from any psychiatric disorder or intellectual disability. These criteria were used to ensure appropriate understanding of the tools for evaluation used and reduce the possibility of the patient's clinical state interfering with the results. The research study was offered to 100% of the patients available in the health district (Haemodialysis Unit at Hospital Médico Quirúrgico, Centro de Hemodiálisis de Santa Catalina, NefroLinares and Centro de Diálisis Playa de la Victoria) who met the inclusion criteria (59 patients). Of these, 52 (88.13%) patients ultimately agreed to participate in the research study. Patient loss was due to a refusal to participate by 3 patients (5.1%) and clinical problems during the research study in 4 patients (6.7%).
Sociodemographic and clinical characteristics of the sample of patients used.
| Variables | N | % |
|---|---|---|
| Age (years) | ||
| 20–29 | 2 | 3.8 |
| 30–39 | 8 | 15.4 |
| 40–49 | 27 | 51.9 |
| 50–60 | 15 | 28.8 |
| Level of education | ||
| No schooling | 6 | 11.5 |
| Primary | 30 | 57.7 |
| Secondary | 9 | 17.3 |
| University | 7 | 13.5 |
| Time in dialysis (years) | ||
| 0.5–5 | 23 | 44.2 |
| 6–10 | 17 | 32.7 |
| 11–20 | 8 | 15.4 |
| ≥21 | 4 | 7.7 |
| Causes of CKD | ||
| Chronic glomerulonephritis | 19 | 36.5 |
| Vascular | 9 | 17.3 |
| Diabetes mellitus | 9 | 17.3 |
| Polycystic kidney disease | 6 | 11.5 |
| Pyelonephritis | 6 | 11.5 |
| Unknown | 3 | 5.8 |
| Previous transplant | ||
| No | 35 | 67.3 |
| Yes | 17 | 32.6 |
The following instruments were administered:
- -
SF-36 Functioning and Quality-of-Life Scale,30 in the Spanish version by Alonso, Prieto and Antó.31 This instrument evaluates the impact of disease on adaptive functioning and provides a state-of-health profile. It contains 36 items with a 2-, 3-, 5- and 6-point Likert response format, depending on the item, with a range from 0 to 100: the higher the score, the better the state of health. It comprises 8 dimensions: physical function, physical role, body pain, general health, vitality, social function, emotional role and mental health. By aggregating these dimensions, 2 components were calculated: a physical health component (PHC) and a mental health component (MHC). The internal consistency (Cronbach's α) of the different scales ranged between 0.7 and 0.94.31 For the PHC, Cronbach's α was 0.94, and for the MHC, it was 0.89.32
- -
Revised Somatic Symptom Scale (ESS-R).33 This instrument evaluates physical health based on symptoms corresponding to the most important somatic/physiological systems. It contains 90 items with a 5-point Likert response format with a range from 0 to 4: the higher the score, the greater the symptoms. They are classified according to the following subscales: general immunological, cardiovascular, respiratory, gastrointestinal, sensorineural, skin/allergy-related, musculoskeletal, female reproductive and genitourinary. The latter 2 subscales were removed from the study. The internal consistency (Cronbach's α) of the different scales ranged between 0.79 and 0.84.33
- -
Hospital Anxiety and Depression Scale (HAD)34 in the Spanish version by Caro and Ibáñez35. This instrument evaluates anxiety and depression levels without taking somatic symptoms into account, and so it limits the possibility that symptoms specific to the disease will contribute to scores. It contains 14 items with a 4-point Likert response format with a range from 0 to 3: the higher the score, the greater the anxiety or depression. It comprises 2 subscales: one for anxiety and one for depression. The instrument had good internal consistency, with a Cronbach's α coefficient of 0.82 for the anxiety subscale and 0.84 for the depression subscale.34
For patient selection, the dialysis centres in the Spanish province of Jaén were contacted (see section: Participants). Once the protocol had been approved by the sites, the nephrologists selected the patients who met the inclusion criteria. The objectives of the study were explained to these patients, and those who agreed to participate signed an informed consent form. Information on sociodemographic and clinical variables was collected during HD sessions through an interview with the patient. Next, a booklet with the questionnaires used in the study was given according to a counterbalanced order. Data was collected during the months of February to June 2014.
Statistical analysisTo increase reliability, reduce the number of statistical analyses and minimise the likelihood of a type I error, statistical analyses were performed with the total scores for each instrument. The 8 dimensions of the SF-36 were reduced to the PHC, the MHC and a total score for HRQoL, based on the average of the 2 subcomponents. A total score was obtained from the ESS-R with the sum of all the symptoms reported. A general score for mood was obtained from the HAD with the sum of the scores in depression and anxiety.
The analysis of the associations between the variables considered to be predictive (somatic symptoms and mood) and the variables identified as dependent (HRQoL in its physical component, its mental component and total) was performed using an exploratory correlational analysis through bivariate Pearson correlations and, subsequently, with a multiple regression analysis. In the regression analysis, as a first step, the variables of age and time in dialysis were entered to control their effect on the subsequent analyses. As a second step, somatic symptoms and mood were entered jointly. In a prior analysis, the interaction factor of somatic symptoms×mood was calculated and entered in the regression analyses. These analyses did not show any interaction effect and were omitted from the results report. To compare the HRQoL levels of the patients with CKD in HD with those of the general Spanish population, the difference in means between each patient's score and the reference values for the SF-36 in the Spanish population was calculated.36 The difference in means obtained was analysed using Student's t test for one sample. The level of significance was set at p<0.05. The data were analysed with the SPSS v. 19.0 statistics program.
ResultsLevels of health-related quality of life, anxiety, depression and somatic symptomsTable 2 shows the scores for HRQoL in its physical component, its mental component and total, together with the reference values for the Spanish population. As may be observed, the HRQoL levels shown by the patients remained below those obtained by the instrument normative sample. Moreover, the levels shown for the PHC were significantly lower than the levels shown for the MHC (t=−4.81; p<0.0001).
Means and standard deviations (SDs) for HRQoL in its physical component (PHC), its mental component (MHC) and total.
| Kidney patients | Spanish population | Comparison of means (t-test) | |||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Dif. in means | t | p | |
| PHC | 53.66 | 22.77 | 84.75 | 21.96 | −31.08 | −9.84 | <0.0001 |
| MHC | 63.60 | 25.18 | 84.81 | 18.54 | −21.21 | −6.07 | <0.0001 |
| Total HRQoL | 58.63 | 22.82 | 84.78 | 20.25 | −26.15 | −8.26 | <0.0001 |
The results are presented as direct scores together with the reference values in the general Spanish population. The result of the comparison of means using Student's t test is also presented.
Table 3 shows the scores for anxiety, depression and overall mood. Definite and likely cases of anxiety comprised 36.5% of the sample, while those of depression comprised 27% of the sample evaluated. The value for total somatic symptoms reported was 83.17, with a standard deviation of 45.51.
Means and standard deviations (SDs) for anxiety, depression and overall mood.
| Anxiety | Depression | Overall score | |||
|---|---|---|---|---|---|
| Mean (±SD) | 7.13 (4.41) | 5.50 (4.26) | 12.63 (7.78) | ||
| Scale criteria | Cases | Percentage | Cases | Percentage | |
| Normality | 33 | 63.5 | 38 | 73 | |
| Probable case | 6 | 11.5 | 7 | 13.5 | |
| Definite case | 13 | 25 | 7 | 13.5 | |
The number and percentage of patients who met the scale's criteria for normality, probable case and definite clinical case are indicated.
Table 4 shows the correlations between HRQoL in its physical and mental component, as well as total, with mood and total somatic symptoms. The results showed a significant negative association between HRQoL, mood and somatic symptoms (p<0.01 in all the correlations). The correlations of HRQoL in its 3 components were higher with mood than with somatic symptoms.
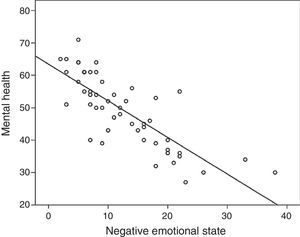
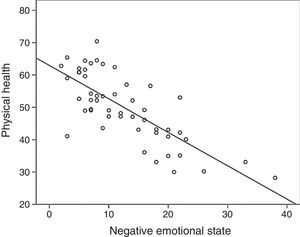
Multiple regression analysis to predict health-related quality of lifeTable 5 presents the results of the multiple regression analysis to predict HRQoL. Age and time in dialysis were not significantly associated with any of the HRQoL indicators. The results obtained showed that mood was the most significant predictor (negative association) of the 3 HRQoL indicators. Total somatic symptoms also negatively predicted the PHC component of HRQoL and overall HRQoL, but with a lower associative capacity than mood. To illustrate these associations, Figs. 1 and 2 show the scatered plots and the regression line that correlates mood to the PHC and the MHC, respectively. Using a stepwise regression procedure for the 2 predictors accurately reproduced the results.
Results of the multiple regression analysis to predict HRQoL in its physical component (PHC), its mental component (MHC) and total, after statistically controlling for the influence of age and time in dialysis.
| Predictive v. | B | r2 | t | p |
|---|---|---|---|---|
| PHC | ||||
| Total symptoms | −0.270 | 0.620 | −2.56 | 0.014 |
| Mood | −0.624 | −5.89 | <0.001 | |
| MHC | ||||
| Total symptoms | −0.177 | 0.639 | −1.73 | 0.091 |
| Mood | −0.709 | −6.87 | <0.001 | |
| Total QoL | ||||
| Total symptoms | −0.231 | 0.680 | −2.39 | 0.021 |
| Mood | −0.691 | −7.12 | <0.001 | |
Our main objective was to compare the predictive capacity of somatic symptoms reported and mood with respect to HRQoL in patients with CKD in HD. First, the possibility of there being an interactive effect among the variables was analysed. The results were negative: both variables exerted additive rather than interactive effects. Given that prior studies have shown that age and time in dialysis may affect quality of life,2,37,38 we performed a statistical control of the effect of both variables. Neither age nor time in dialysis was found to be significantly associated with HRQoL in any of the regression analyses performed. One potential explanation for that may lie in the limited range of variability for both variables in our sample.
The results of the regression analyses showed that mood was the main predictor of HRQoL, both in the PHC and in the MHC. Given that the association was negative, a more negative mood was associated with a decrease in HRQoL indicators. In addition, with a lower degree of association, somatic symptoms also negatively predicted the physical component of HRQoL and overall HRQoL. Taken together, mood and somatic symptoms accounted for 68% of variance in total HRQoL, 64% of variance in the MHC and 62% of variance in the PHC. Given the magnitude of the standardised β statistics observed (between −0.624 and −0.709), these results showed convincing evidence about the influence of mood on the determination of quality of life. These results were consistent with those found in prior studies that have shown the negative influence of anxiety and depression on HRQoL.12,21–24
Our results agree with findings from previous studies2,20,36,37,39,40 that have shown that the HRQoL levels reported by patients, in both its physical component and its mental component, are well below the reference values of the SF-36 questionnaire in the Spanish population.36 It should be noted that the PHC obtained an average significantly lower than the MHC. This indicated that patients with CKD in HD perceive and are aware of the physical limitations deriving from the disease,16 beyond the potential repercussions in the social and emotional sphere. These results were consistent with prior studies, in which it has been observed that, in advanced CKD in the HD phase, the patient has physical limitations, that cannot be attributed to other comorbid conditions.41 Symptoms specific to the disease limit physical activity, interfere with daily activities, intensify pain and its effect on usual work, and lead the patient to make a worse assessment of his or her state of health. Regarding mood, probable-certain cases of anxiety comprised 36.5% of the sample, and those of depression comprised 27% of the sample. Therefore, it should be noted that there were higher values for abnormalities linked to anxiety than to depression. It is known that physiological manifestations linked to anxiety (muscle tension, sympathetic hyperarousal, parasympathetic inhibition, etc.), when they occur for long periods of time, may promote somatic complications such as hypertension42 and foster a greater report of physical symptoms in patients with CKD.17 The percentages observed for the two disorders were greater than the reported prevalence of disorders of anxiety and depression in the general Spanish population43 and agree with prior studies on the prevalence of anxiety and depression in patients in dialysis, which according to other studies have been around 27%44 for anxiety and between 20% and 30% for depression.45 Focusing on the somatic symptoms reported, the levels shown by our sample of patients in HD are considered to be high as compared with the results obtained, with the same evaluation tool, in a group of healthy people with similar sociodemographic characteristics (M=49.30; SD=22.14).17
It must be emphasised that CKD and HD treatment are highly stressful life events.20 Given the duration of the disease and its prognosis, the stress is chronic. This chronic stress leads to anxiety and depressive states with uncertainty about the future (dialysis or transplant for survival) and fear of losing control of his or her life are essential matters.46 Anxiety is a common problem in the kidney patient that is present since the initiation of HD treatment11,47 and it is associated to a lower quality of life.48 Similarly, vital stress and the limitations imposed by a chronic disease such as CKD induce powerlessness and loss of hope that, depending on how patients cope with them, may lead to depression. If the depressive symptoms of the patient in dialysis become chronic or recurrent, they may lead the patient to experience a substantial decrease in his or her capacity to take care of day-to-day responsibilities, to assess his or her current and future health more negatively, to perceive more tiredness and exhaustion, to experience intensified body pain and to suffer a decline in his or her social life and mental health.10
In chronic kidney diseased patients there is a high comorbidity between anxiety and depression.49 Given that the origin of this anxious/depressive mood normally results from the difficulty of adapting to a stressful life event, which requires profound changes in the patient's life (CKD itself), the most common and correct psychiatric diagnosis is adjustment disorder with mixed anxiety and depressed mood.14 This study analysed mood as comprised of the combined influence of anxiety and depression. The results showed that a worse mood predicts a decrease in the kidney patient's quality of life. These results were along the lines of other studies that have shown the effect of emotional disturbances in CKD and their interference with how patients think, feel and act regarding the disease.11,14,23 Negative mood may intensify the manifestations of the disease and worsen its course and progression, as well as interfere with treatment, as it is associated with non-adherence behaviours.12,23,39 When the renal patient has a negative mood (anxiety and depression), he or she loses perceived control over the disease and its treatment. This low perceived self-efficacy may derive from engagement in counterproductive behaviours such as low adherence, abusive use of medical services and improper performance of nephrology indications and required care. These behaviours may cause serious consequences for the patient, including malnutrition, neuropathies, bone diseases, heart failure, etc.,50 and lead to a more pronounced deterioration in quality of life12 and an increased risk of mortality.11,12,39 These results noted the importance of early evaluation51 and treatment of negative moods (anxiety and depression) in kidney patients, as a form of promoting better clinical results and lowering the disease's interference with HRQoL. Therefore, for comprehensive care of the kidney patient, it is very important to address negative moods. This may modulate the disease's interference with the patient's adaptive functioning.
One limitation of our study lay in the inclusion criterion of being 60 years of age or younger, given that the population in dialysis is generally older. This inclusion criterion reduced the sample size. The objective of this criterion was to ensure optimal understanding of psychological tests and therefore achieve greater validity. Consequently, our results could not be directly extrapolated to other age ranges. Another limitation lay in the procedure used to measure somatic symptoms, using self-report scales. It would be advisable to replicate the results obtained with other more direct health indicators. However, the scale used to measure somatic symptoms had good psychometric properties and validity consistent with external measures of state of health, such as self-reports on diseases and external criteria for health such as clinical diagnoses,33 and such scales have become indispensable for research in health.
In conclusion, the kidney patient's mood (anxiety and depression) is a powerful predictor of HRQoL, in both its physical and mental components, while somatic symptoms are a predictor of PHC. Bearing in mind the high prevalence of anxiety and depression in the kidney patient, their negative effect on HRQoL and their importance in the determination of rates of morbidity/mortality due to various diseases,20 these results have shown the need for the kidney patient to be evaluated and addressed preventively51 as early as the predialysis phase to equip him or her with coping resources to manage stress and the needs for adaptation imposed by his or her disease.26,52 This may result in lower subsequent interference by the disease with HRQoL and foster an improvement in the course and progression of the disease, by promoting adaptive behaviours associated with greater adherence to treatment and the patient's more active involvement in disease management.52
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Perales Montilla CM, Duschek S, Reyes del Paso GA. Calidad de vida relacionada con la salud en la enfermedad renal crónica: relevancia predictiva del estado de ánimo y la sintomatología somática. Nefrologia. 2016;36:275–282.